Last week I presented to the WHO Guidelines Development Group. It was targeted towards infectious disease epidemiologists, but many folks have asked me to share the presentation.
So, here& #39;s a video discussion. Read the thread below to see each slide. 1/ https://youtu.be/WFrLdJ1Rpyg ">https://youtu.be/WFrLdJ1Rp...
So, here& #39;s a video discussion. Read the thread below to see each slide. 1/ https://youtu.be/WFrLdJ1Rpyg ">https://youtu.be/WFrLdJ1Rp...
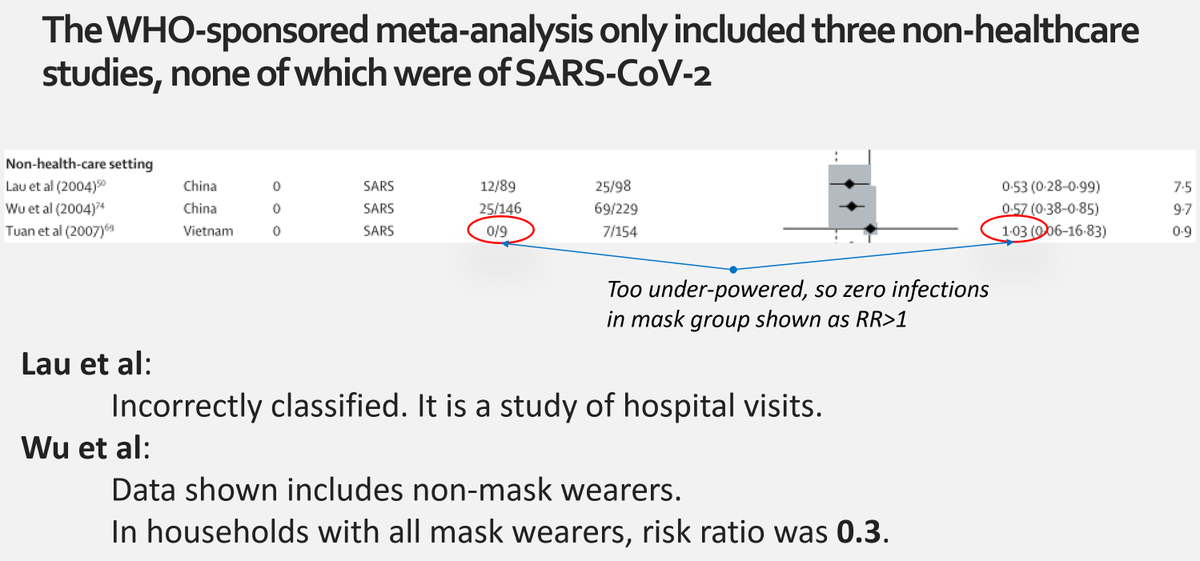
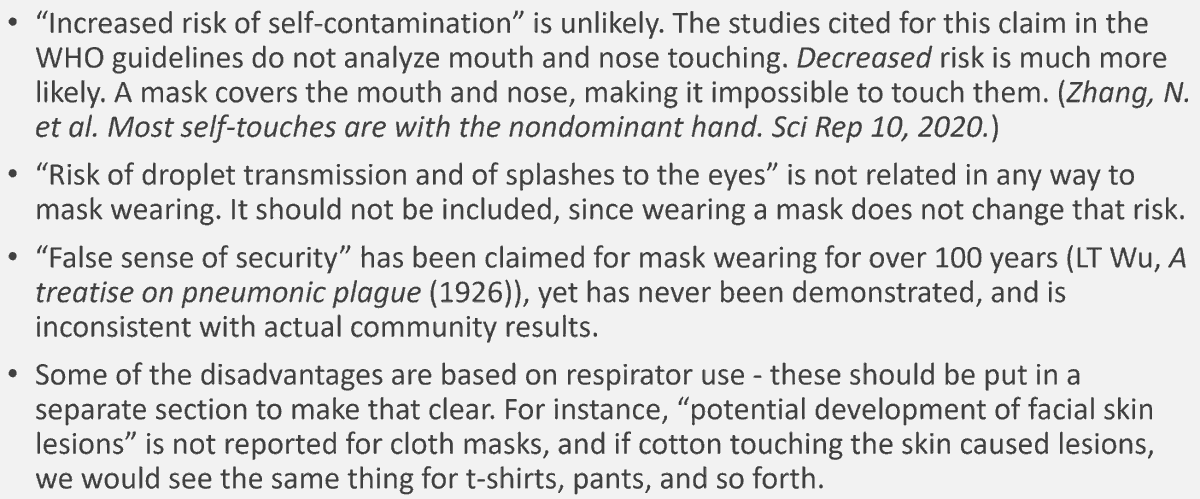
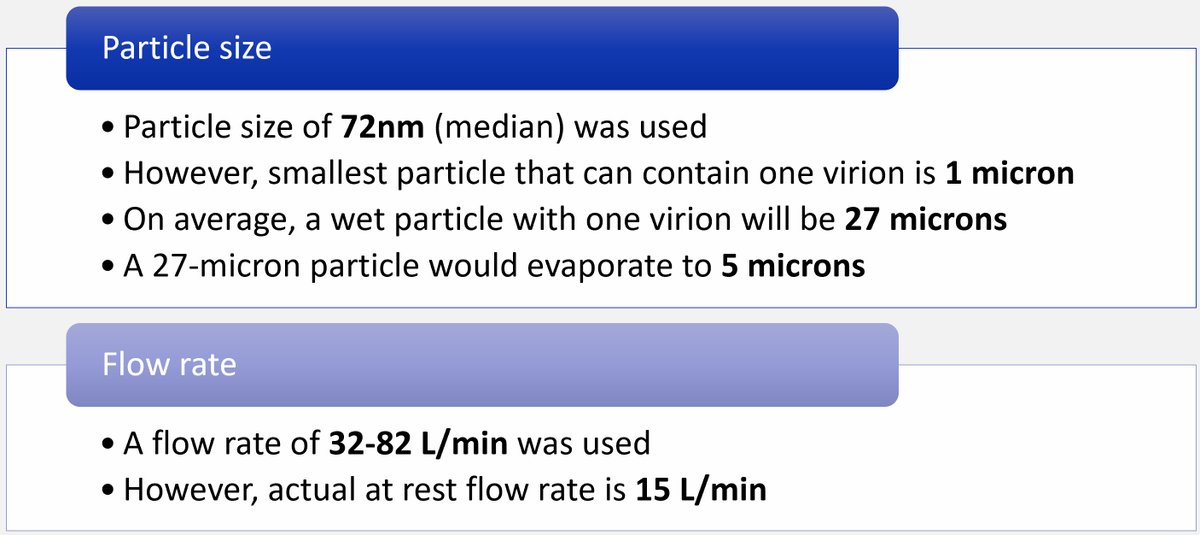
The evidence that WHO relies on for its mask guidelines has many problems. For instance, the meta-analysis they sponsored only has 3 non-healthcare studies, 1 of which is wrongly categorized, and one of which is under-powered. None studied COVID-19.
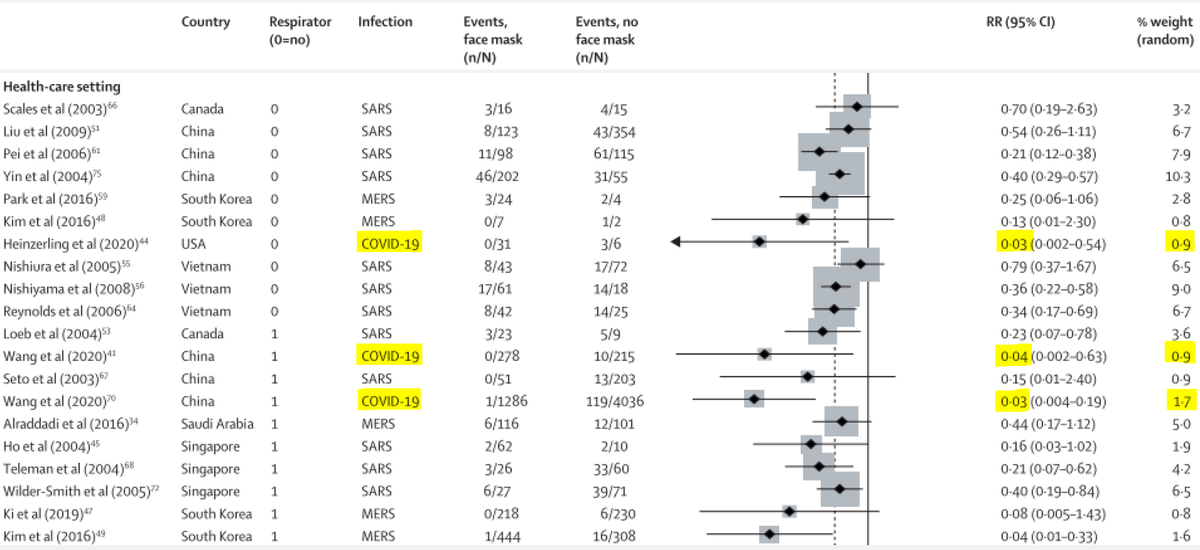
The review had three studies of SARS-CoV-2 in healthcare, but largely ignored them, by using inappropriate statistical techniques. (See the tiny weights in the right-most column.)
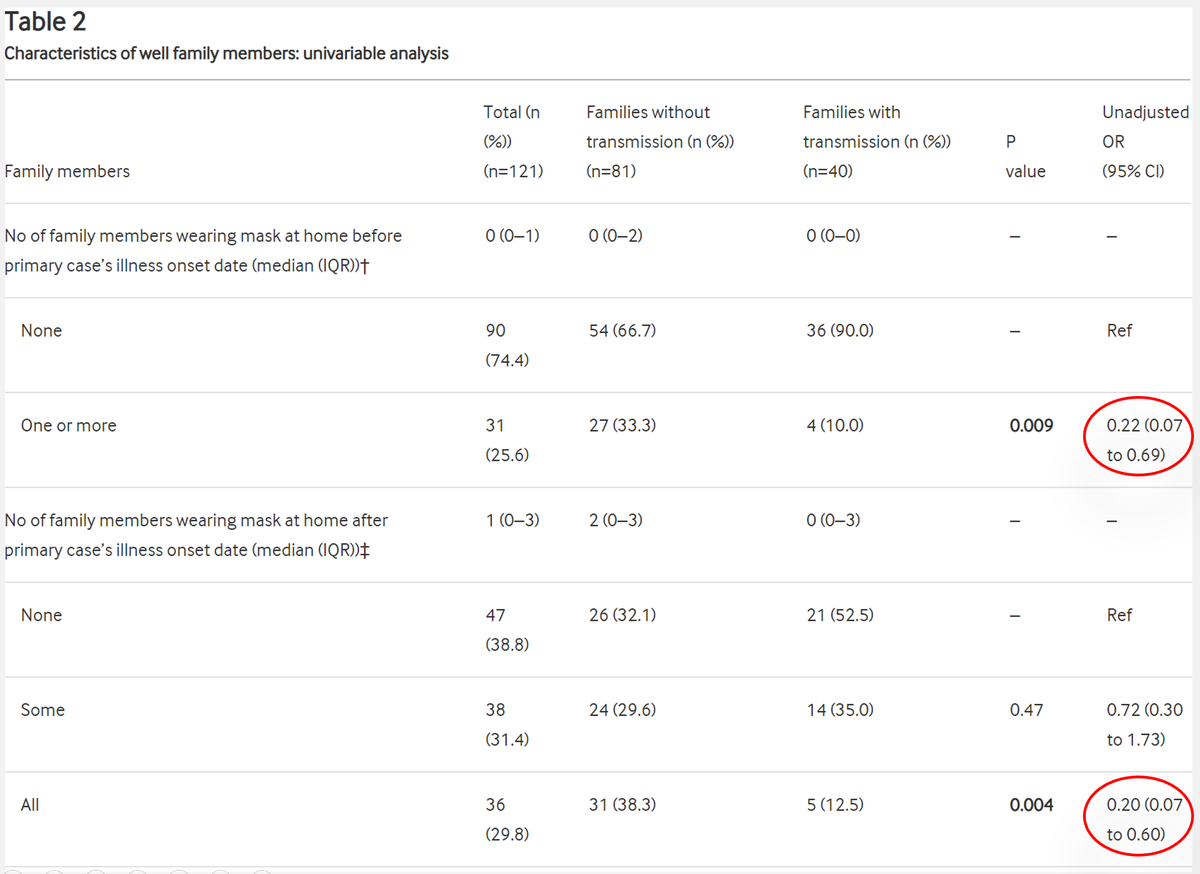
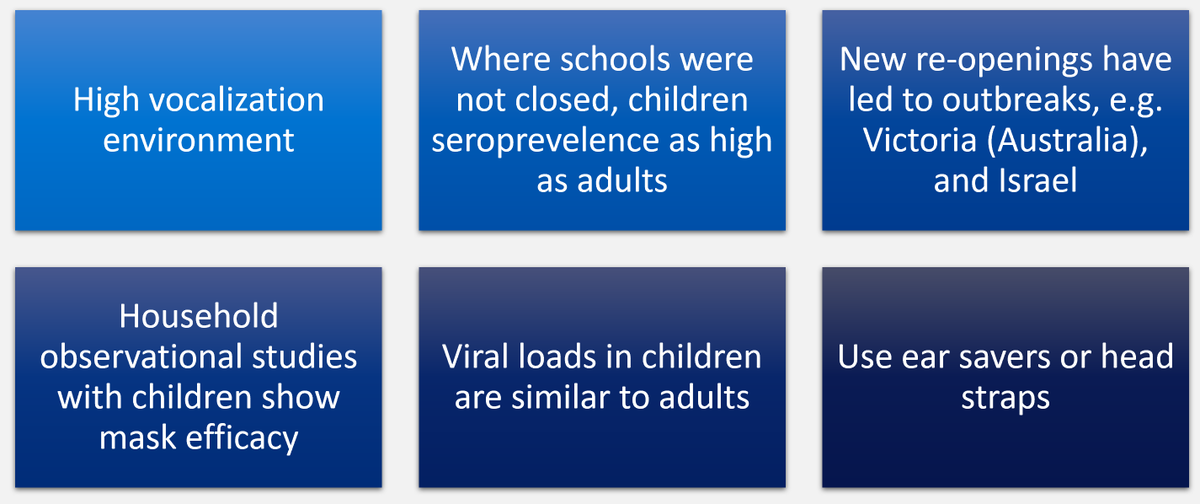
There has been a study of mask wearing in households for reducing COVID-19 transmission, which showed around 80% reduction in transmission.
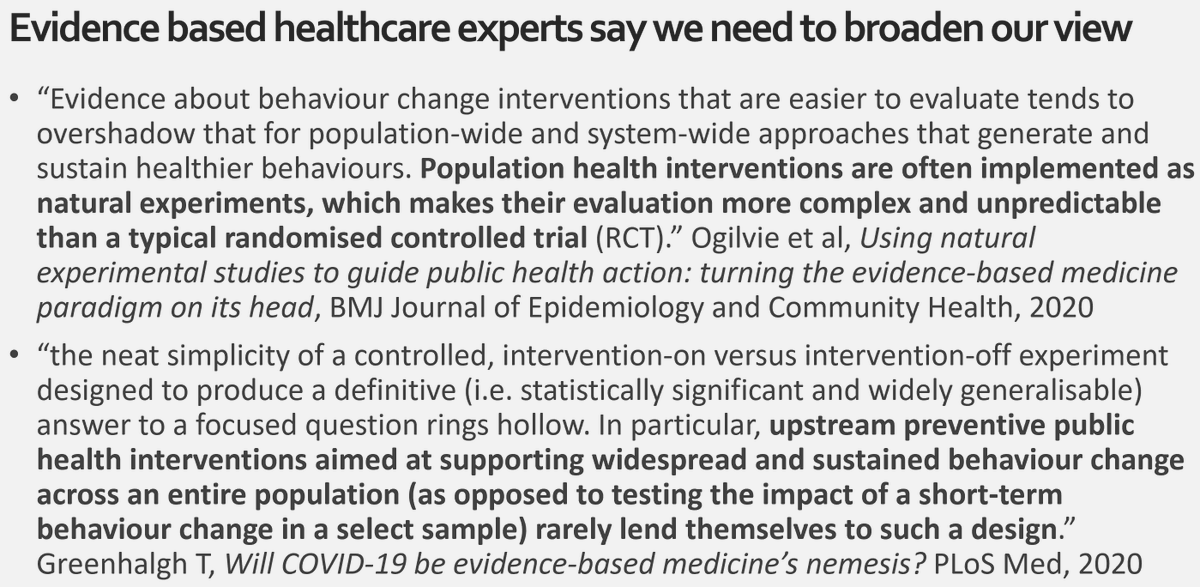
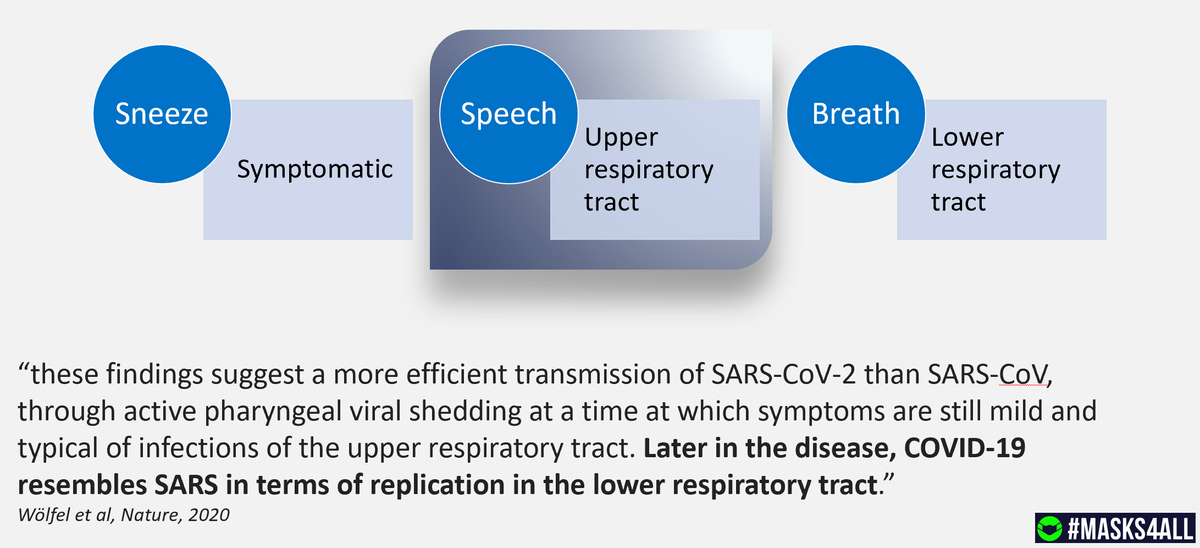
Classic epidemiological studies can never really tell us if masks reduce community transmission, because if I (for instance) wear a mask, how do you know which people I contact avoided getting sick because of me?
So we have to broaden our evidence base.
So we have to broaden our evidence base.
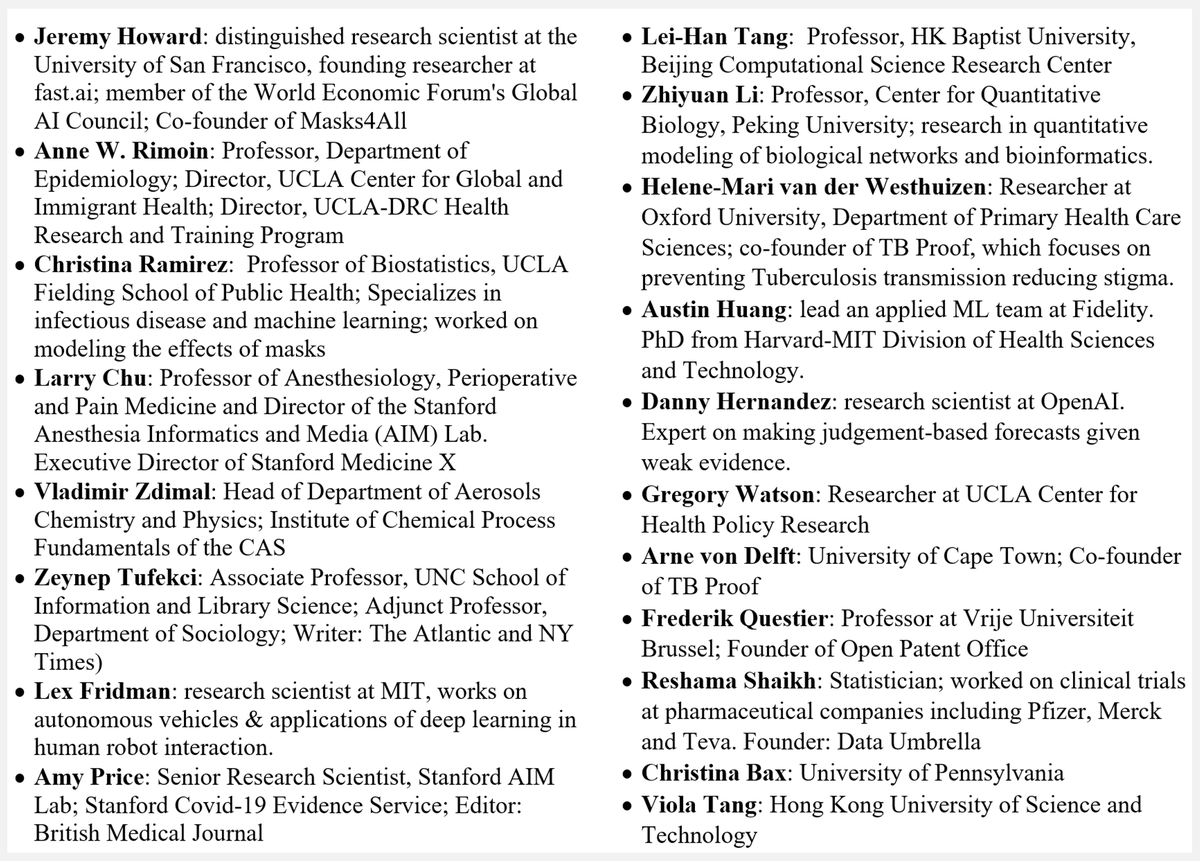
Our review of the evidence for masks, from 155 references, is the most viewed paper ever on http://preprints.org"> http://preprints.org . It is now being reviewed at PNAS.
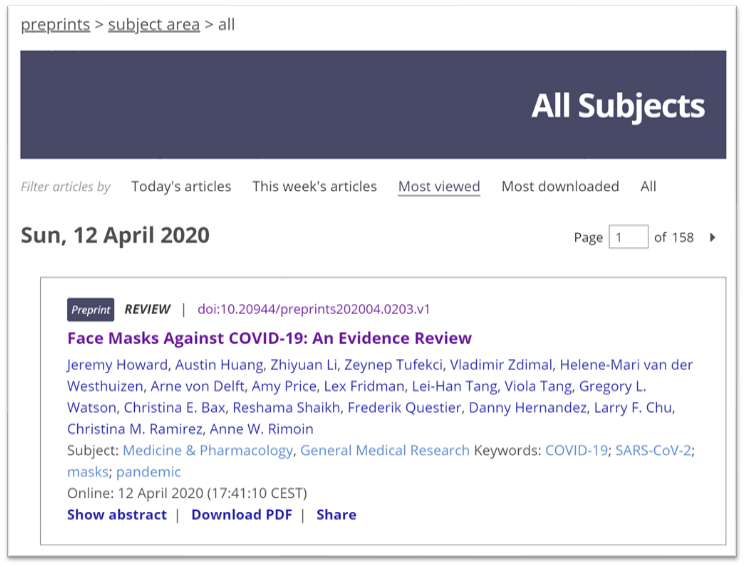
>80% of the world now lives in regions that require masks, plus most of the US. These means there are many natural experiments we can analyze.
Sometime epidemiologists assume that& #39;s not useful, due to the "ecological fallacy", but there& #39;s decades of research on good approaches
Sometime epidemiologists assume that& #39;s not useful, due to the "ecological fallacy", but there& #39;s decades of research on good approaches
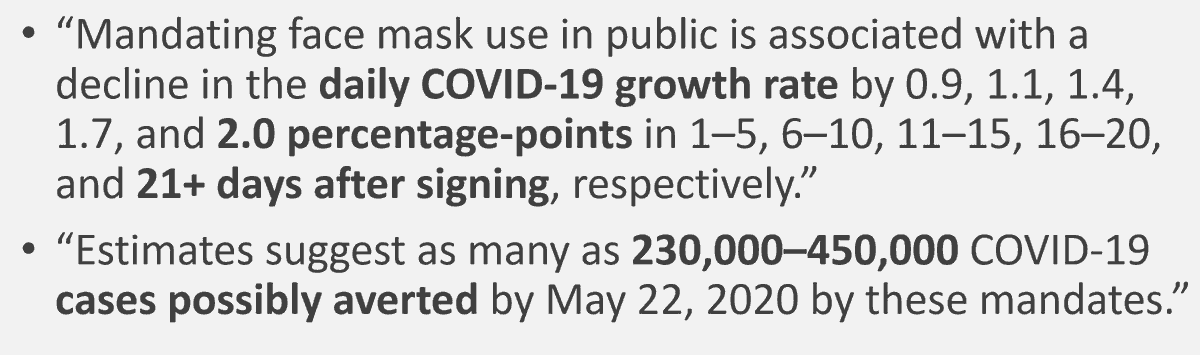
Leffler ( @ChrisLefflerMD) et al looked at nearly 200 countries, adjusted for dozens of confounders. Mask use was associated in a 5-10x decrease in transmission rate.
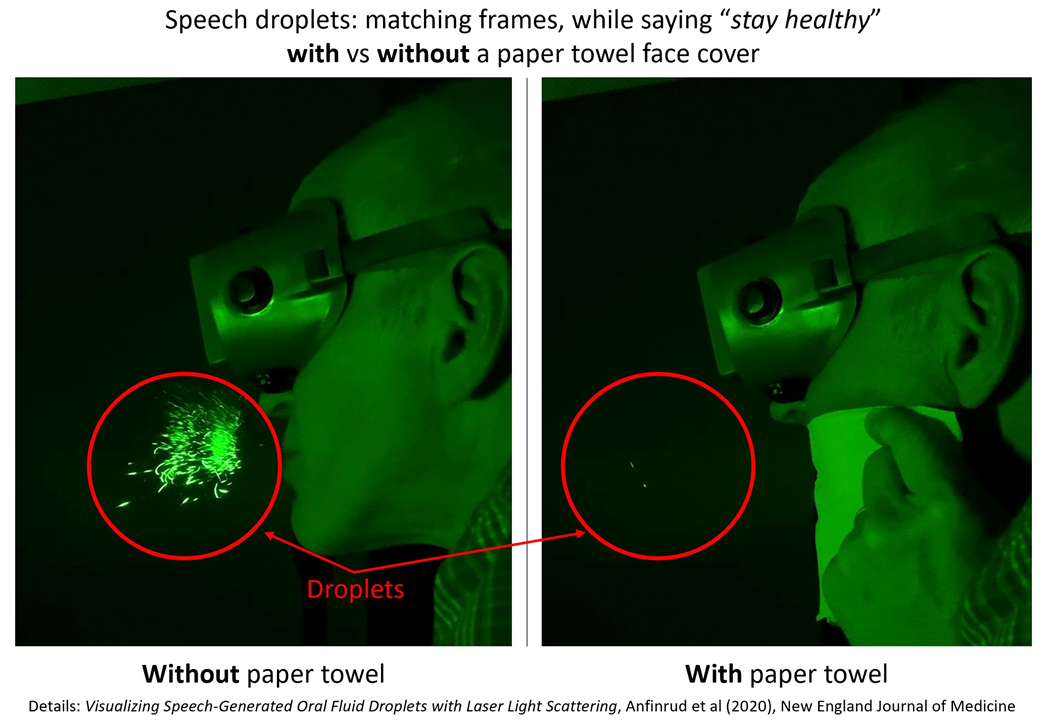
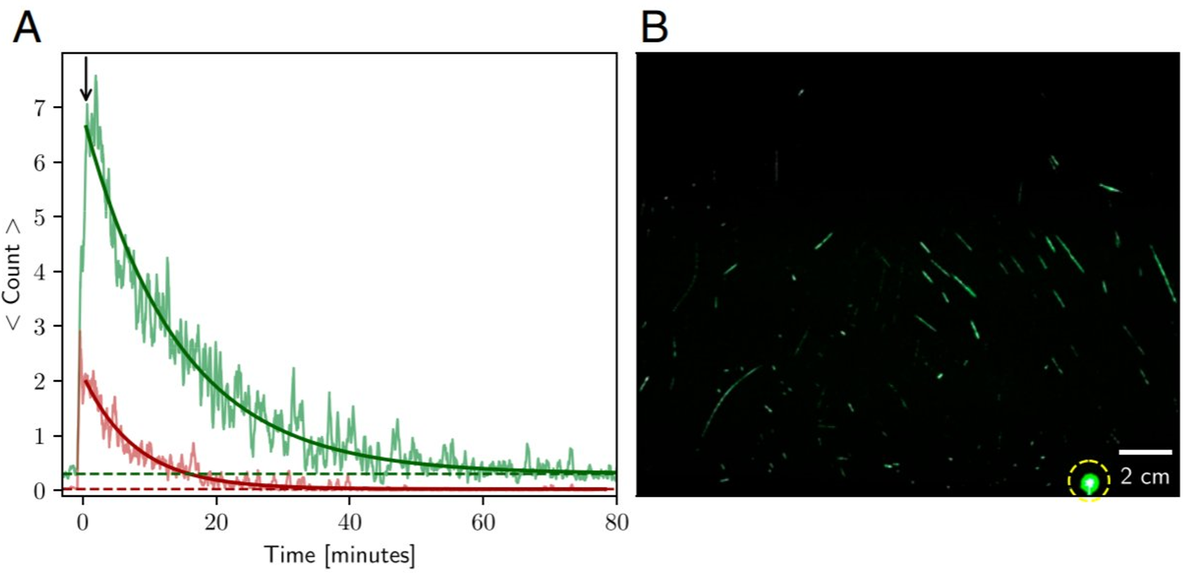
We also have great lab evidence, including videos and images directly showing a simple piece of kitchen paper towel blocking nearly all speech droplets, which are believed to be responsible for a lot of transmission
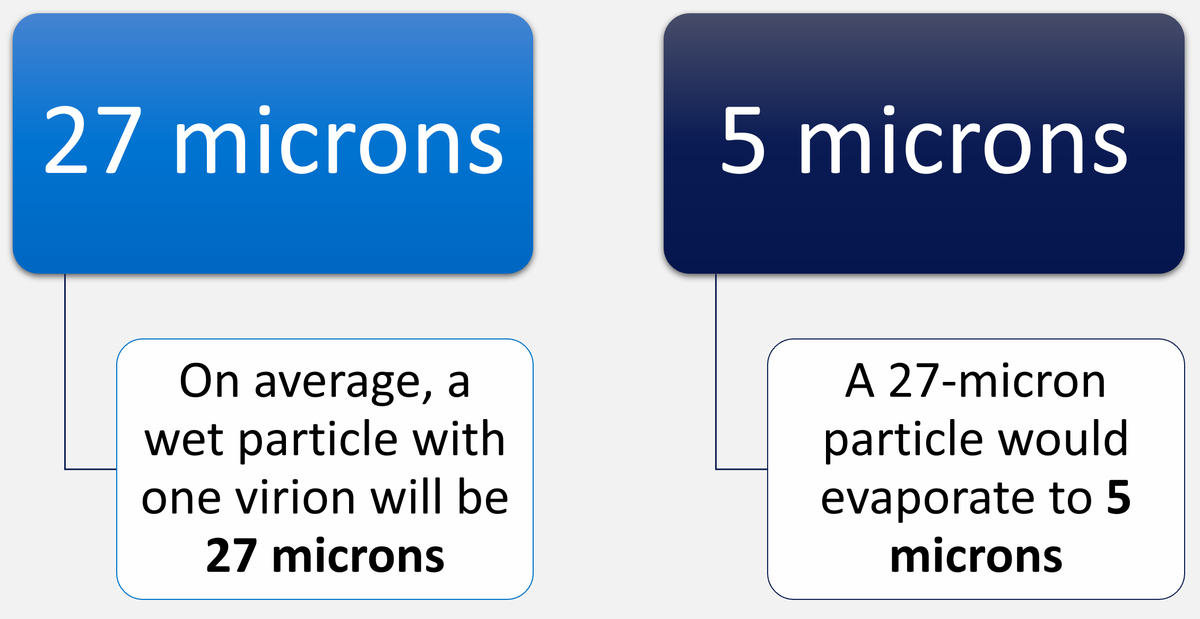
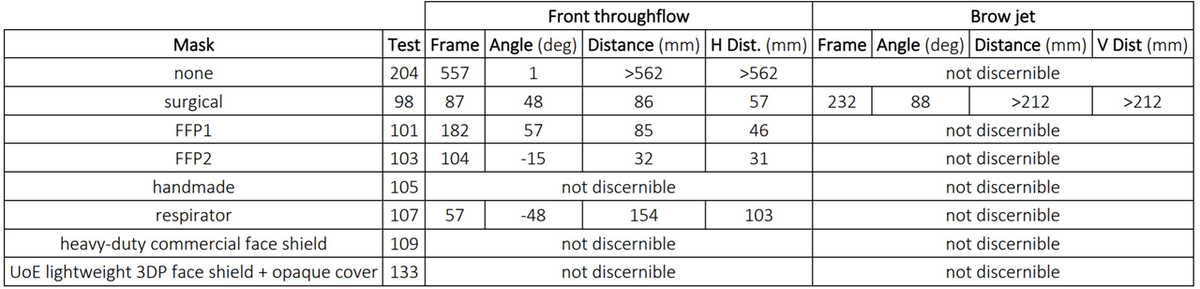
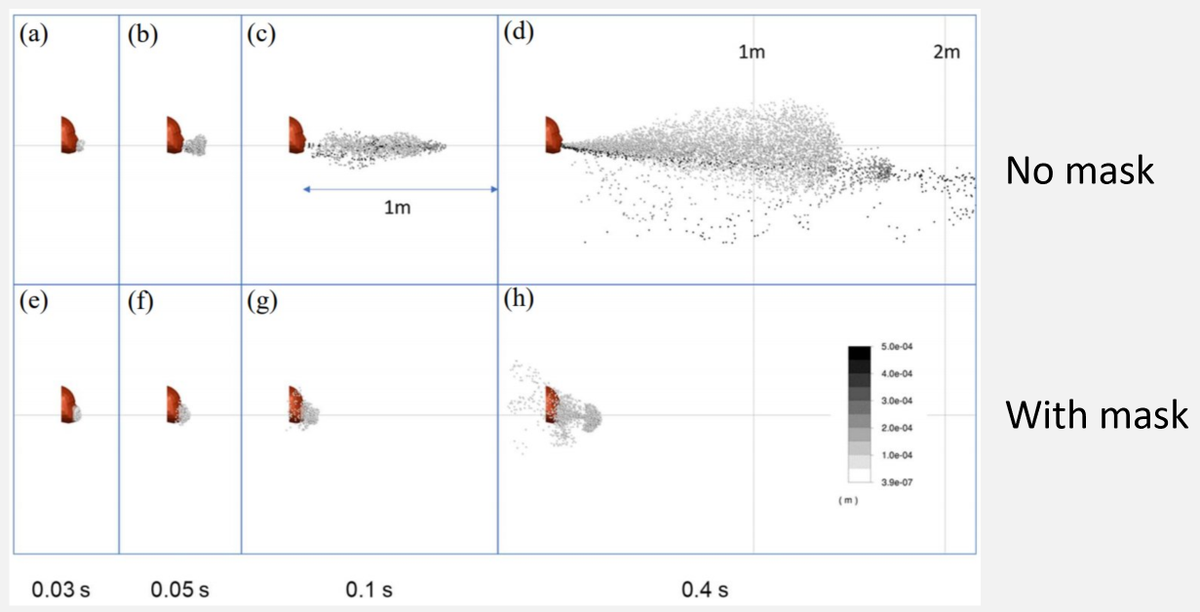
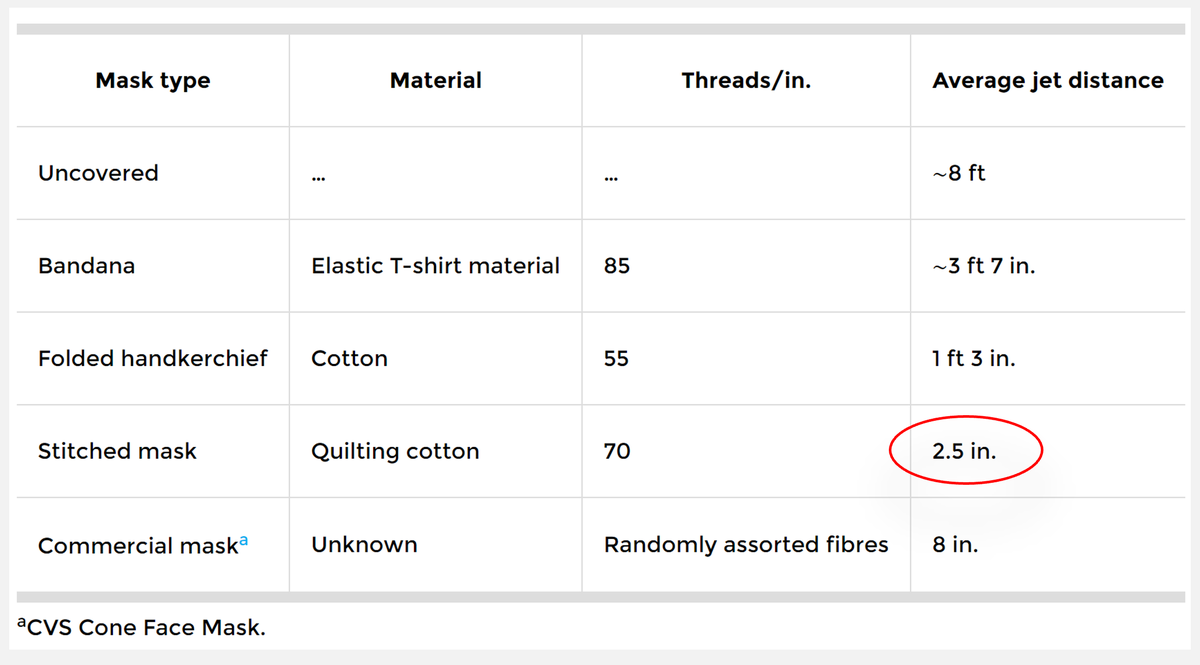
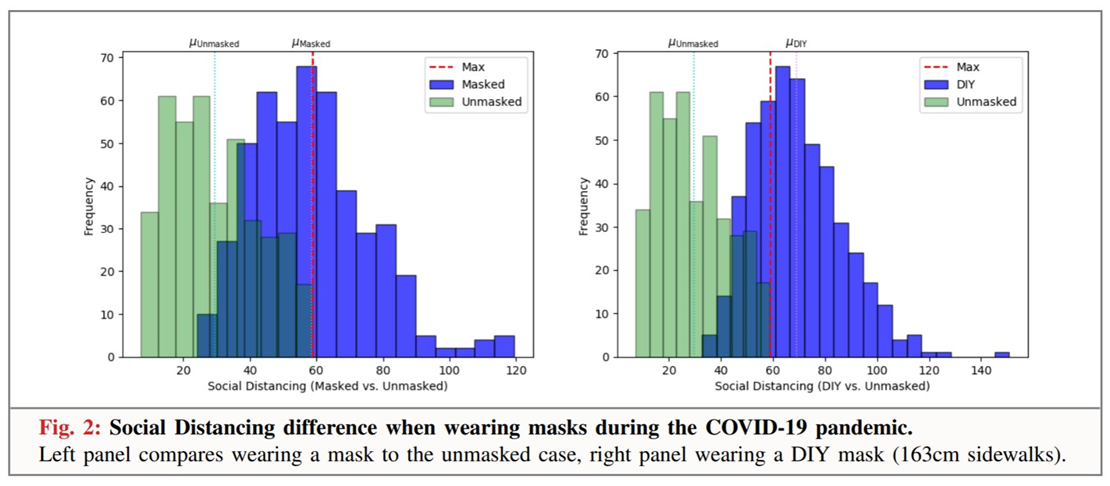
Fluid dynamics analysis supports the finding that cloth masks decrease the radius of the droplet cloud
Masks can improve the effectiveness of distancing, both due to the smaller droplet cloud, and though social signaling
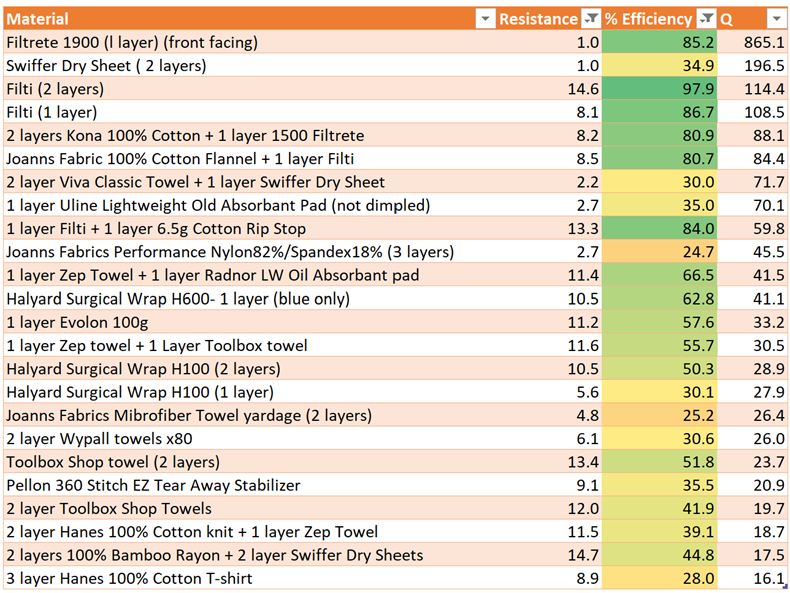
Even for PPE, WHO& #39;s table is missing the highest quality materials, such as these:
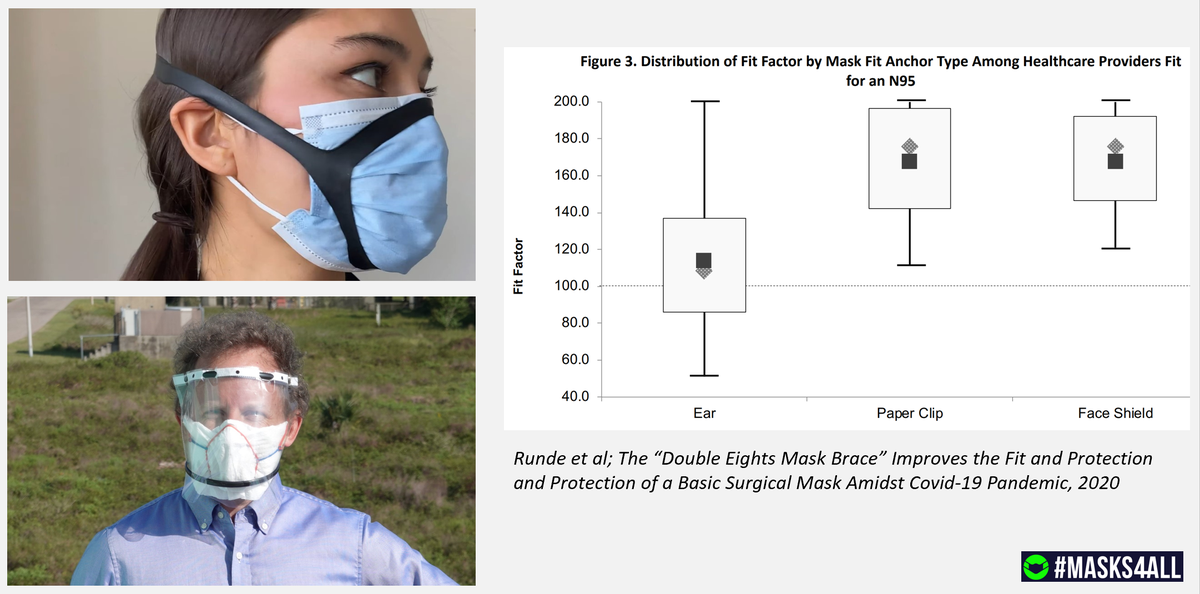
WHO& #39;s guidelines also fail to discuss the most effective DIY mask designs
For references to the papers, and more details, please see the full video. https://youtu.be/WFrLdJ1Rpyg ">https://youtu.be/WFrLdJ1Rp...
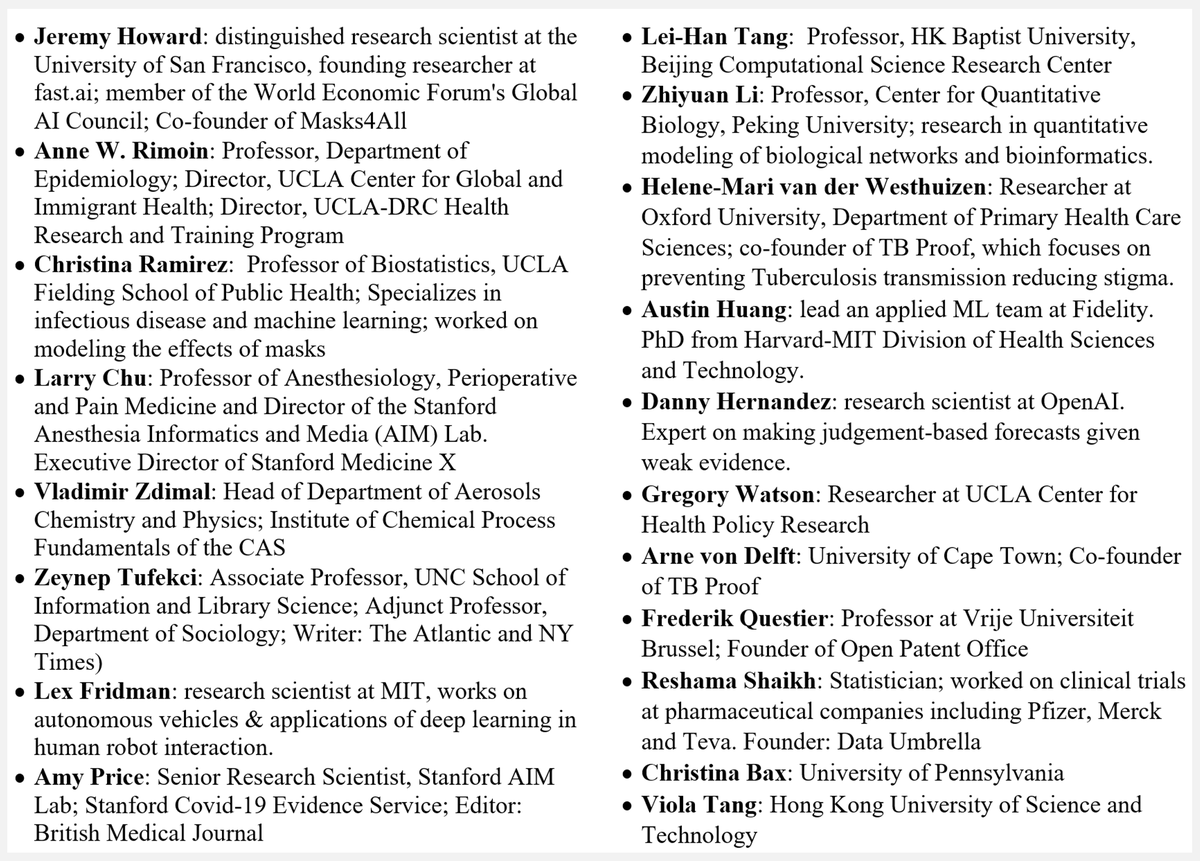
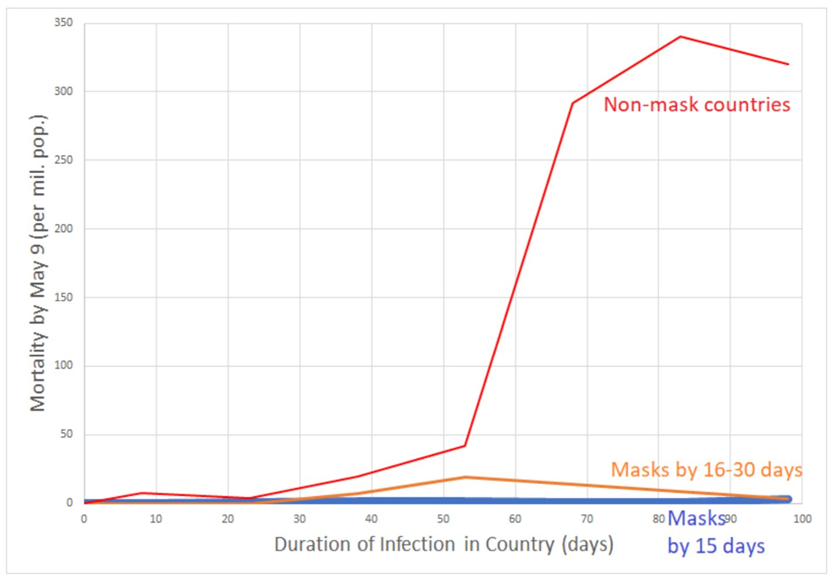
Huge thanks too all my great co-authors, @arimoin, @larrychu, @zeynep, @lexfridman, @austinvhuang, @hernandez_danny, @arnedelft, @HeleneMarivdW, @AmyPricePhD, @reshamas, Z. Li, C. Ramirez, L. Tang, V. Zdimal, C. Bax, G. Watson & V. Tang.
& to @VincentRK @trishgreenhalgh & more!
& to @VincentRK @trishgreenhalgh & more!
Here& #39;s the unrolled thread in a single web page: https://threadreaderapp.com/thread/1285618568793591814.html">https://threadreaderapp.com/thread/12...

 Read on Twitter
Read on Twitter