Hard to believe #PGY4 is here! Grateful for the opportunity to share more about #HAES and #IntuitiveEating with fellow trainees in #peds today for my senior talk. I learned so much along the way I thought I might create a brief #tweetorial of the summary of my literature review. https://twitter.com/UABMedPeds/status/1285363975916531719">https://twitter.com/UABMedPed...
#HAES or health at every size is a method of nutrition counseling focused on promoting body acceptance, encouraging nutrition  https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍎" title="Roter Apfel" aria-label="Emoji: Roter Apfel">, and gentle movement
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍎" title="Roter Apfel" aria-label="Emoji: Roter Apfel">, and gentle movement  https://abs.twimg.com/emoji/v2/... draggable="false" alt="💪" title="Angespannter Bizeps" aria-label="Emoji: Angespannter Bizeps"> without an aim of weight loss.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💪" title="Angespannter Bizeps" aria-label="Emoji: Angespannter Bizeps"> without an aim of weight loss.
In brief: pursuing health-promoting habits at any weight/body size.
In brief: pursuing health-promoting habits at any weight/body size.
A 2013 study in @JAMAPediatrics showed children whose parents used “weight-centered” language were more likely to diet frequently, binge eat, or have eating disorders as teens.
Parents that focused on healthy eating ONLY had a protective effect on all the above for their teens.
Parents that focused on healthy eating ONLY had a protective effect on all the above for their teens.
Another review from @AmerAcadPeds in 2016 showed dieting w/ the intent of weight loss was the #1️⃣ risk factor for developing an eating disorder as well as predictive of weight gain.
In fact a normal BMI 9th grade girl who diets is more likely to be overweight by 12th grade. https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤯" title="Explodierender Kopf" aria-label="Emoji: Explodierender Kopf">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤯" title="Explodierender Kopf" aria-label="Emoji: Explodierender Kopf">
In fact a normal BMI 9th grade girl who diets is more likely to be overweight by 12th grade.
The same study showed that children exposed to “weight talk” in any form—I.e.
“I have to lose 20 lbs before I can wear a swimsuit https://abs.twimg.com/emoji/v2/... draggable="false" alt="👙" title="Bikini" aria-label="Emoji: Bikini">”
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👙" title="Bikini" aria-label="Emoji: Bikini">”
Or
“Did you see how much weight Sarah’s mom gained this summer?”
Were more likely to have significant weight gain at 5 year follow up.
“I have to lose 20 lbs before I can wear a swimsuit
Or
“Did you see how much weight Sarah’s mom gained this summer?”
Were more likely to have significant weight gain at 5 year follow up.
Children exposed to #weightstigma or #weightteasing via parents https://abs.twimg.com/emoji/v2/... draggable="false" alt="👨" title="Mann" aria-label="Emoji: Mann">, peers
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👨" title="Mann" aria-label="Emoji: Mann">, peers  https://abs.twimg.com/emoji/v2/... draggable="false" alt="👧" title="Mädchen" aria-label="Emoji: Mädchen">, or physicians
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👧" title="Mädchen" aria-label="Emoji: Mädchen">, or physicians  https://abs.twimg.com/emoji/v2/... draggable="false" alt="👩⚕️" title="Woman health worker" aria-label="Emoji: Woman health worker">were more likely to develop binge eating/purging behaviors or weight gain at 5 year follow-up.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👩⚕️" title="Woman health worker" aria-label="Emoji: Woman health worker">were more likely to develop binge eating/purging behaviors or weight gain at 5 year follow-up.
Weight teasing is also associated with decreased likelihood to exercise in children.
Weight teasing is also associated with decreased likelihood to exercise in children.
On the other hand eating at least one meal  https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍽" title="Gabel und Messer mit Teller" aria-label="Emoji: Gabel und Messer mit Teller"> with family
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍽" title="Gabel und Messer mit Teller" aria-label="Emoji: Gabel und Messer mit Teller"> with family  https://abs.twimg.com/emoji/v2/... draggable="false" alt="👨👩👧👦" title="Normale Familie (Mann, Frau, Mädchen, Junge)" aria-label="Emoji: Normale Familie (Mann, Frau, Mädchen, Junge)"> 7 days a week was predictive of increased
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👨👩👧👦" title="Normale Familie (Mann, Frau, Mädchen, Junge)" aria-label="Emoji: Normale Familie (Mann, Frau, Mädchen, Junge)"> 7 days a week was predictive of increased  https://abs.twimg.com/emoji/v2/... draggable="false" alt="🥦" title="Brokkoli" aria-label="Emoji: Brokkoli">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🥦" title="Brokkoli" aria-label="Emoji: Brokkoli"> https://abs.twimg.com/emoji/v2/... draggable="false" alt="🥕" title="Karotte" aria-label="Emoji: Karotte">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🥕" title="Karotte" aria-label="Emoji: Karotte"> https://abs.twimg.com/emoji/v2/... draggable="false" alt="🥬" title="Leafy green" aria-label="Emoji: Leafy green">intake, long term healthy eating patterns, and protective against EDs, bing eating, and dieting.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🥬" title="Leafy green" aria-label="Emoji: Leafy green">intake, long term healthy eating patterns, and protective against EDs, bing eating, and dieting.
Patients that had healthy body image (regardless of BMI) were also more likely to pursue healthy activities like exercise  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⛹️♀️" title="Woman bouncing ball" aria-label="Emoji: Woman bouncing ball">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⛹️♀️" title="Woman bouncing ball" aria-label="Emoji: Woman bouncing ball"> https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤸♀️" title="Woman cartwheeling" aria-label="Emoji: Woman cartwheeling">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤸♀️" title="Woman cartwheeling" aria-label="Emoji: Woman cartwheeling"> https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧘" title="Person im Lotossitz" aria-label="Emoji: Person im Lotossitz">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧘" title="Person im Lotossitz" aria-label="Emoji: Person im Lotossitz"> https://abs.twimg.com/emoji/v2/... draggable="false" alt="🏊♀️" title="Schwimmerin" aria-label="Emoji: Schwimmerin"> and eat healthfully
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🏊♀️" title="Schwimmerin" aria-label="Emoji: Schwimmerin"> and eat healthfully  https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍉" title="Wassermelone" aria-label="Emoji: Wassermelone">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍉" title="Wassermelone" aria-label="Emoji: Wassermelone"> https://abs.twimg.com/emoji/v2/... draggable="false" alt="🥝" title="Kiwi fruit" aria-label="Emoji: Kiwi fruit">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🥝" title="Kiwi fruit" aria-label="Emoji: Kiwi fruit"> https://abs.twimg.com/emoji/v2/... draggable="false" alt="🥑" title="Avocado" aria-label="Emoji: Avocado">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🥑" title="Avocado" aria-label="Emoji: Avocado"> https://abs.twimg.com/emoji/v2/... draggable="false" alt="🥔" title="Kartoffel" aria-label="Emoji: Kartoffel">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🥔" title="Kartoffel" aria-label="Emoji: Kartoffel"> https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍳" title="Kochen" aria-label="Emoji: Kochen">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍳" title="Kochen" aria-label="Emoji: Kochen"> https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍞" title="Brot" aria-label="Emoji: Brot"> without the desire to change their body size.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍞" title="Brot" aria-label="Emoji: Brot"> without the desire to change their body size.
What can we do as #pediatricians
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="1️⃣" title="Tastenkappe Ziffer 1" aria-label="Emoji: Tastenkappe Ziffer 1">Use #MI to encourage behavior changes rather than weight changes.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="1️⃣" title="Tastenkappe Ziffer 1" aria-label="Emoji: Tastenkappe Ziffer 1">Use #MI to encourage behavior changes rather than weight changes.
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="2️⃣" title="Tastenkappe Ziffer 2" aria-label="Emoji: Tastenkappe Ziffer 2">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="2️⃣" title="Tastenkappe Ziffer 2" aria-label="Emoji: Tastenkappe Ziffer 2">  https://abs.twimg.com/emoji/v2/... draggable="false" alt="🗣" title="Silhouette eines sprechenden Kopfes" aria-label="Emoji: Silhouette eines sprechenden Kopfes"> Language Matters: Use weight-neutral language in visits.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🗣" title="Silhouette eines sprechenden Kopfes" aria-label="Emoji: Silhouette eines sprechenden Kopfes"> Language Matters: Use weight-neutral language in visits.
“Moving your body is a great way to have fun and strengthen your muscles!” https://abs.twimg.com/emoji/v2/... draggable="false" alt="💪" title="Angespannter Bizeps" aria-label="Emoji: Angespannter Bizeps">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💪" title="Angespannter Bizeps" aria-label="Emoji: Angespannter Bizeps">
“Moving your body is a great way to have fun and strengthen your muscles!”
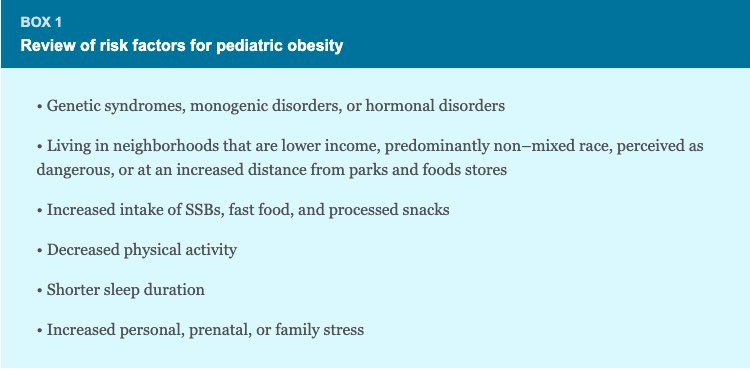
-Access to fresh foods
-Distance to parks
-Neigborhood safety
To name a few directly correlated with #pediatricobesity.
- weight teasing
- poor body image
- dieting behaviors
- binge eating
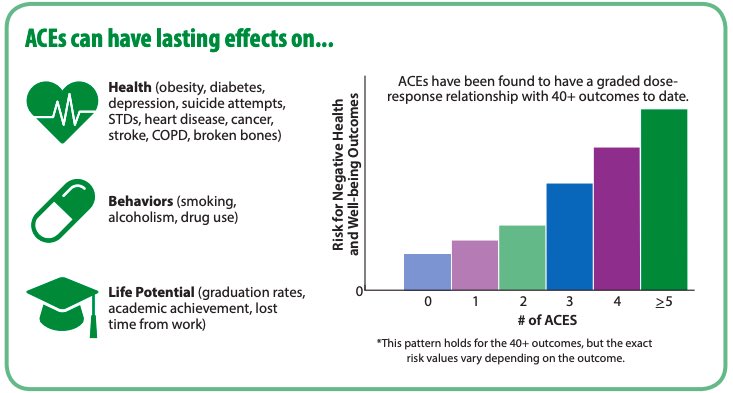
- family/personal stressors
- mental illness
- lack of family meals
Bottom line:
The factors that contribute to weight are far beyond https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍴" title="Messer und Gabel" aria-label="Emoji: Messer und Gabel">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍴" title="Messer und Gabel" aria-label="Emoji: Messer und Gabel"> https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍔" title="Hamburger" aria-label="Emoji: Hamburger">and
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍔" title="Hamburger" aria-label="Emoji: Hamburger">and  https://abs.twimg.com/emoji/v2/... draggable="false" alt="🏃" title="Person running" aria-label="Emoji: Person running">.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🏃" title="Person running" aria-label="Emoji: Person running">.
Addressing systemic and familial barriers to health including #ACEs and providing stigma-free health education should be our priority as physicians—not changing children’s bodies!
The factors that contribute to weight are far beyond
Addressing systemic and familial barriers to health including #ACEs and providing stigma-free health education should be our priority as physicians—not changing children’s bodies!
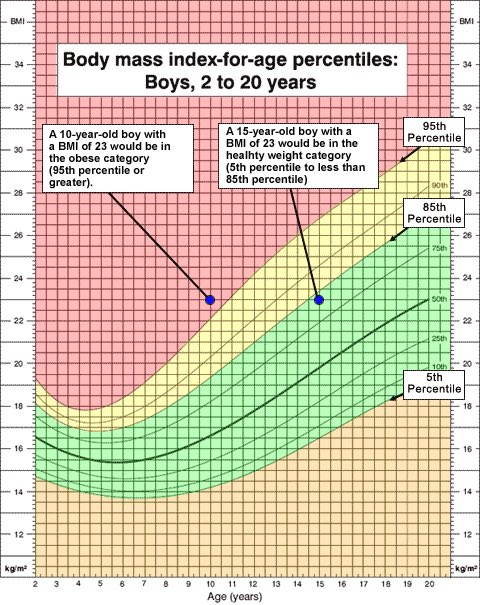
One final note on BMI:
The pediatric BMI scale utilized by clinicians is based on expert recommendation only. While it can be a useful tool for screening for the above risk factors and comorbidities “healthy BMI” ≠ health nor does “obese BMI” = lack of health.
The pediatric BMI scale utilized by clinicians is based on expert recommendation only. While it can be a useful tool for screening for the above risk factors and comorbidities “healthy BMI” ≠ health nor does “obese BMI” = lack of health.
Takeaways:
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍊" title="Mandarine" aria-label="Emoji: Mandarine">Avoid weight talk with pediatric patients
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍊" title="Mandarine" aria-label="Emoji: Mandarine">Avoid weight talk with pediatric patients
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍓" title="Erdbeere" aria-label="Emoji: Erdbeere">Focusing on health behaviors > weight loss efforts.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍓" title="Erdbeere" aria-label="Emoji: Erdbeere">Focusing on health behaviors > weight loss efforts.
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍍" title="Ananas" aria-label="Emoji: Ananas">Health thinness nor does obesity=comorbidities
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍍" title="Ananas" aria-label="Emoji: Ananas">Health thinness nor does obesity=comorbidities
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍅" title="Tomate" aria-label="Emoji: Tomate">Consider background factors contributing to weight
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍅" title="Tomate" aria-label="Emoji: Tomate">Consider background factors contributing to weight
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🥦" title="Brokkoli" aria-label="Emoji: Brokkoli">Provide weight-neutral, evidence-based education to ALL patients
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🥦" title="Brokkoli" aria-label="Emoji: Brokkoli">Provide weight-neutral, evidence-based education to ALL patients
Thanks for following along!
Resources to learn more about #HAES and #intuitiveeating in pediatrics and beyond:
@IntuitiveEat @chr1styharrison @FeedingLittles @Etribole @ElyseResch to name a few!
Would love to hear what other physicians are doing in this area!
Resources to learn more about #HAES and #intuitiveeating in pediatrics and beyond:
@IntuitiveEat @chr1styharrison @FeedingLittles @Etribole @ElyseResch to name a few!
Would love to hear what other physicians are doing in this area!

 Read on Twitter
Read on Twitter , and gentle movement https://abs.twimg.com/emoji/v2/... draggable="false" alt="💪" title="Angespannter Bizeps" aria-label="Emoji: Angespannter Bizeps"> without an aim of weight loss. In brief: pursuing health-promoting habits at any weight/body size." title=" #HAES or health at every size is a method of nutrition counseling focused on promoting body acceptance, encouraging nutrition https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍎" title="Roter Apfel" aria-label="Emoji: Roter Apfel">, and gentle movement https://abs.twimg.com/emoji/v2/... draggable="false" alt="💪" title="Angespannter Bizeps" aria-label="Emoji: Angespannter Bizeps"> without an aim of weight loss. In brief: pursuing health-promoting habits at any weight/body size." class="img-responsive" style="max-width:100%;"/>
, and gentle movement https://abs.twimg.com/emoji/v2/... draggable="false" alt="💪" title="Angespannter Bizeps" aria-label="Emoji: Angespannter Bizeps"> without an aim of weight loss. In brief: pursuing health-promoting habits at any weight/body size." title=" #HAES or health at every size is a method of nutrition counseling focused on promoting body acceptance, encouraging nutrition https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍎" title="Roter Apfel" aria-label="Emoji: Roter Apfel">, and gentle movement https://abs.twimg.com/emoji/v2/... draggable="false" alt="💪" title="Angespannter Bizeps" aria-label="Emoji: Angespannter Bizeps"> without an aim of weight loss. In brief: pursuing health-promoting habits at any weight/body size." class="img-responsive" style="max-width:100%;"/>

 " title="Another review from @AmerAcadPeds in 2016 showed dieting w/ the intent of weight loss was the #1️⃣ risk factor for developing an eating disorder as well as predictive of weight gain.In fact a normal BMI 9th grade girl who diets is more likely to be overweight by 12th grade. https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤯" title="Explodierender Kopf" aria-label="Emoji: Explodierender Kopf">" class="img-responsive" style="max-width:100%;"/>
" title="Another review from @AmerAcadPeds in 2016 showed dieting w/ the intent of weight loss was the #1️⃣ risk factor for developing an eating disorder as well as predictive of weight gain.In fact a normal BMI 9th grade girl who diets is more likely to be overweight by 12th grade. https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤯" title="Explodierender Kopf" aria-label="Emoji: Explodierender Kopf">" class="img-responsive" style="max-width:100%;"/>
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍔" title="Hamburger" aria-label="Emoji: Hamburger">and https://abs.twimg.com/emoji/v2/... draggable="false" alt="🏃" title="Person running" aria-label="Emoji: Person running">.Addressing systemic and familial barriers to health including #ACEs and providing stigma-free health education should be our priority as physicians—not changing children’s bodies!" title="Bottom line:The factors that contribute to weight are far beyond https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍴" title="Messer und Gabel" aria-label="Emoji: Messer und Gabel">https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍔" title="Hamburger" aria-label="Emoji: Hamburger">and https://abs.twimg.com/emoji/v2/... draggable="false" alt="🏃" title="Person running" aria-label="Emoji: Person running">.Addressing systemic and familial barriers to health including #ACEs and providing stigma-free health education should be our priority as physicians—not changing children’s bodies!">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍔" title="Hamburger" aria-label="Emoji: Hamburger">and https://abs.twimg.com/emoji/v2/... draggable="false" alt="🏃" title="Person running" aria-label="Emoji: Person running">.Addressing systemic and familial barriers to health including #ACEs and providing stigma-free health education should be our priority as physicians—not changing children’s bodies!" title="Bottom line:The factors that contribute to weight are far beyond https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍴" title="Messer und Gabel" aria-label="Emoji: Messer und Gabel">https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍔" title="Hamburger" aria-label="Emoji: Hamburger">and https://abs.twimg.com/emoji/v2/... draggable="false" alt="🏃" title="Person running" aria-label="Emoji: Person running">.Addressing systemic and familial barriers to health including #ACEs and providing stigma-free health education should be our priority as physicians—not changing children’s bodies!">
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍔" title="Hamburger" aria-label="Emoji: Hamburger">and https://abs.twimg.com/emoji/v2/... draggable="false" alt="🏃" title="Person running" aria-label="Emoji: Person running">.Addressing systemic and familial barriers to health including #ACEs and providing stigma-free health education should be our priority as physicians—not changing children’s bodies!" title="Bottom line:The factors that contribute to weight are far beyond https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍴" title="Messer und Gabel" aria-label="Emoji: Messer und Gabel">https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍔" title="Hamburger" aria-label="Emoji: Hamburger">and https://abs.twimg.com/emoji/v2/... draggable="false" alt="🏃" title="Person running" aria-label="Emoji: Person running">.Addressing systemic and familial barriers to health including #ACEs and providing stigma-free health education should be our priority as physicians—not changing children’s bodies!">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍔" title="Hamburger" aria-label="Emoji: Hamburger">and https://abs.twimg.com/emoji/v2/... draggable="false" alt="🏃" title="Person running" aria-label="Emoji: Person running">.Addressing systemic and familial barriers to health including #ACEs and providing stigma-free health education should be our priority as physicians—not changing children’s bodies!" title="Bottom line:The factors that contribute to weight are far beyond https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍴" title="Messer und Gabel" aria-label="Emoji: Messer und Gabel">https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍔" title="Hamburger" aria-label="Emoji: Hamburger">and https://abs.twimg.com/emoji/v2/... draggable="false" alt="🏃" title="Person running" aria-label="Emoji: Person running">.Addressing systemic and familial barriers to health including #ACEs and providing stigma-free health education should be our priority as physicians—not changing children’s bodies!">