Excited to share our new study in @JAMANetworkOpen-more evidence that value-based incentive programs function as a disproportionate penalty system for safety-net hospitals without meaningful benefits for patients: http://ja.ma/2ZRnrRa
This">https://ja.ma/2ZRnrRa&q... is #StructuralRacism in action. https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧵" title="Thread" aria-label="Emoji: Thread"> 1/
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧵" title="Thread" aria-label="Emoji: Thread"> 1/
This">https://ja.ma/2ZRnrRa&q... is #StructuralRacism in action.
2/ Value-based incentive programs aim to  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> healthcare quality and
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> healthcare quality and  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten"> cost by linking $$ (incentives or penalties) to hospital performance (sounds great, right?), but there can be unintended consequences for safety-net hospitals & their patients. http://shorturl.at/iqvIJ ">https://shorturl.at/iqvIJ&quo...
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten"> cost by linking $$ (incentives or penalties) to hospital performance (sounds great, right?), but there can be unintended consequences for safety-net hospitals & their patients. http://shorturl.at/iqvIJ ">https://shorturl.at/iqvIJ&quo...
3/ First, what is a safety-net hospital? By mission or mandate, safety-net hospitals provide healthcare to a disproportionate share of people without the means to pay or who are insured by Medicaid. https://www.bmc.org/healthcity/policy-and-industry/critical-role-safety-net-health-systems-podcast">https://www.bmc.org/healthcit...
4/ Because of #StructuralRacism, safety-net hospitals care disproportionately for Black, Latinx, Indigenous, and other people of color. Here’s a good primer if you want more historical background: https://www.theatlantic.com/politics/archive/2016/05/americas-health-segregation-problem/483219/">https://www.theatlantic.com/politics/...
5/ Safety-net hospitals have lower operating margins AND are more likely to be penalized when participating in value-based incentive programs than non-safety-net hospitals: https://bit.ly/3eq006A ">https://bit.ly/3eq006A&q... and https://jamanetwork.com/journals/jama/fullarticle/2411284">https://jamanetwork.com/journals/...
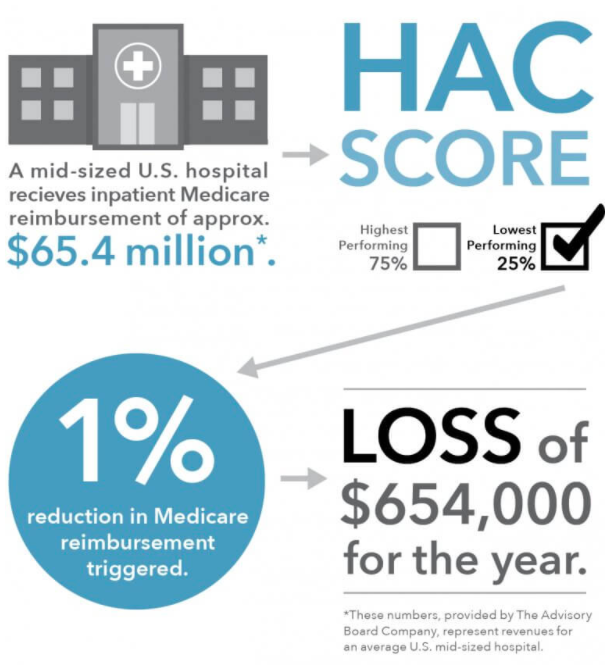
6/ Our study looked at 2 federal value-based incentive programs that target healthcare-associated infections: Hospital Value-Based Purchasing ( #HVBP) & Hospital-Acquired Conditions Reduction Program ( #HACRP). If you& #39;re interested, here& #39;s how HACRP works:
7/ We used an interrupted time series design to assess the association between #HACRP and #HVBP with changes in targeted infection rates in safety-net and non-safety-net hospitals & disparities in infection rates between safety-net and non-safety-net hospitals
8/ We included 618 hospitals that participated in #HVBP & #HACRP and mandated @CDCgov National Healthcare Safety Network healthcare-associated infection surveillance https://www.cdc.gov/nhsn/about-nhsn/index.html">https://www.cdc.gov/nhsn/abou...
9/ We found:
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🚫" title=""Betreten verboten!"-Zeichen" aria-label="Emoji: "Betreten verboten!"-Zeichen">No change in surveillance-based rates of targeted infections associated with #HVBP & #HACRP in either safety-net or non-safety-net hospitals
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🚫" title=""Betreten verboten!"-Zeichen" aria-label="Emoji: "Betreten verboten!"-Zeichen">No change in surveillance-based rates of targeted infections associated with #HVBP & #HACRP in either safety-net or non-safety-net hospitals
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="☑️" title="Kästchen mit Häkchen" aria-label="Emoji: Kästchen mit Häkchen"> Persistent disparities in infection rates (safety-net hospital rates > non-safety-net)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="☑️" title="Kästchen mit Häkchen" aria-label="Emoji: Kästchen mit Häkchen"> Persistent disparities in infection rates (safety-net hospital rates > non-safety-net)
10/ Why does this matter? If value-based incentive programs don’t improve outcomes & disparities in targeted quality metrics are persistent, then the programs are functioning as a disproportionate penalty system for the safety-net without any demonstrated benefit to patients.
11/ Disproportionate financial penalization may affect the financial stability of the safety-net & consequently the quality of health care for the patients served (i.e., expect an outsized impact on BIPOC & rural communities). #StructuralRacism
12/ The healthcare safety-net& #39;s financial wellbeing is particularly relevant right now: With #COVID19, >5 million Americans lost health insurance in 2020. This is devastating for individuals & will also  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> uncompensated care costs for safety-net hospitals https://www.familiesusa.org/resources/the-covid-19-pandemic-and-resulting-economic-crash-have-caused-the-greatest-health-insurance-losses-in-american-history">https://www.familiesusa.org/resources...
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> uncompensated care costs for safety-net hospitals https://www.familiesusa.org/resources/the-covid-19-pandemic-and-resulting-economic-crash-have-caused-the-greatest-health-insurance-losses-in-american-history">https://www.familiesusa.org/resources...
13/ And the CARES Act, even with recent modifications, likely has not sufficiently addressed financial shortfalls for safety-net hospitals
http://disq.us/t/3pouv4y ">https://disq.us/t/3pouv4y... and http://shorturl.at/mIPQR ">https://shorturl.at/mIPQR&quo...
http://disq.us/t/3pouv4y ">https://disq.us/t/3pouv4y... and http://shorturl.at/mIPQR ">https://shorturl.at/mIPQR&quo...
14/ Despite #COVID19, planned cuts to Disproportionate Share Hospital (DSH) payments (federal $ meant to offset uncompensated care costs & low Medicaid reimbursement) are continuing mostly unabated ($4 billion in 2021 then $8 billion/yr thru 2025) https://www.aha.org/advisory/2020-03-25-senate-white-house-reach-agreement-relief-package-responding-covid-19">https://www.aha.org/advisory/...
15/ Without even accounting for the COVID19-related shortfalls & increases in uncompensated care, planned cuts to DSH payments will drive the average operating margin of safety-net hospitals into the red https://essentialhospitals.org/institute/essential-data-our-hospitals-our-patients/">https://essentialhospitals.org/institute...
16/ So, what to do? Structural problem → structural solutions! We must advocate for:
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen">Stopping ALL planned DSH cuts
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen">Stopping ALL planned DSH cuts
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen">More CARES Act attn to safety-net
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen">More CARES Act attn to safety-net
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen">Medicaid expansion
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen">Medicaid expansion
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">Medicaid reimbursement
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">Medicaid reimbursement
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen">decoupling health insurance & employment https://www.usa.gov/elected-officials">https://www.usa.gov/elected-o...
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen">decoupling health insurance & employment https://www.usa.gov/elected-officials">https://www.usa.gov/elected-o...
17/ As for #HVBP and #HACRP, we probably need a total overhaul to drive real change, but at minimum, CMS should stratify hospitals by safety-net status before assessing financial penalties & stop double-counting infections in both #HVBP & #HACRP.
18/ Want more research on the healthy equity implications of value-based care? Check out our session @AcademyHealth virtual #ARM20 on 8/4. Also not to miss:  https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔥" title="Feuer" aria-label="Emoji: Feuer">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔥" title="Feuer" aria-label="Emoji: Feuer"> https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔥" title="Feuer" aria-label="Emoji: Feuer">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔥" title="Feuer" aria-label="Emoji: Feuer"> https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔥" title="Feuer" aria-label="Emoji: Feuer"> plenary on 7/28: "Race, Research and the Power and Peril of Big Data" from @ruha9 @RRHDr @ShreyaKangovi & David Asch
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔥" title="Feuer" aria-label="Emoji: Feuer"> plenary on 7/28: "Race, Research and the Power and Peril of Big Data" from @ruha9 @RRHDr @ShreyaKangovi & David Asch
19/19 Thank you to @The_BMC Health City for amplifying! @BUmedicine @AHRQnews @DeptPopMed @GleeHMS @DAGoldmann @StephenSoumerai @ashishkjha https://www.bmc.org/healthcity/research/value-based-payments-incentives-are-not-improving-care-outcomes">https://www.bmc.org/healthcit...

 Read on Twitter
Read on Twitter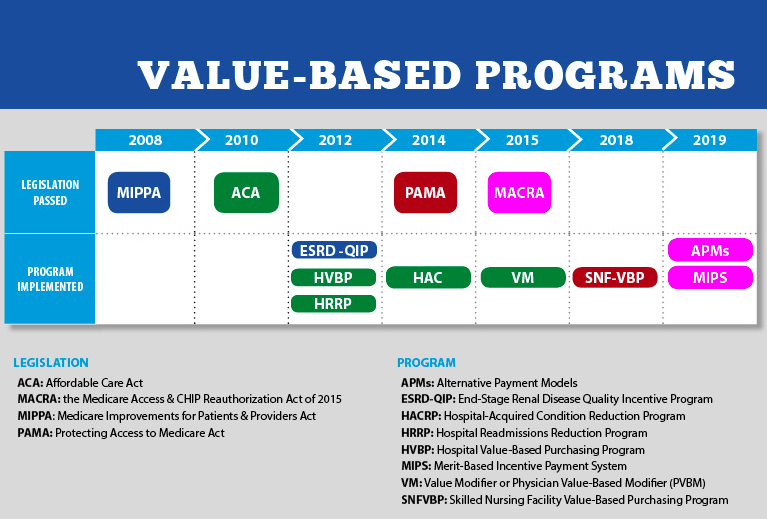 healthcare quality and https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten"> cost by linking $$ (incentives or penalties) to hospital performance (sounds great, right?), but there can be unintended consequences for safety-net hospitals & their patients. https://shorturl.at/iqvIJ&quo..." title="2/ Value-based incentive programs aim to https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> healthcare quality and https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten"> cost by linking $$ (incentives or penalties) to hospital performance (sounds great, right?), but there can be unintended consequences for safety-net hospitals & their patients. https://shorturl.at/iqvIJ&quo..." class="img-responsive" style="max-width:100%;"/>
healthcare quality and https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten"> cost by linking $$ (incentives or penalties) to hospital performance (sounds great, right?), but there can be unintended consequences for safety-net hospitals & their patients. https://shorturl.at/iqvIJ&quo..." title="2/ Value-based incentive programs aim to https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> healthcare quality and https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten"> cost by linking $$ (incentives or penalties) to hospital performance (sounds great, right?), but there can be unintended consequences for safety-net hospitals & their patients. https://shorturl.at/iqvIJ&quo..." class="img-responsive" style="max-width:100%;"/>

 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔥" title="Feuer" aria-label="Emoji: Feuer">https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔥" title="Feuer" aria-label="Emoji: Feuer"> plenary on 7/28: "Race, Research and the Power and Peril of Big Data" from @ruha9 @RRHDr @ShreyaKangovi & David Asch" title="18/ Want more research on the healthy equity implications of value-based care? Check out our session @AcademyHealth virtual #ARM20 on 8/4. Also not to miss: https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔥" title="Feuer" aria-label="Emoji: Feuer">https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔥" title="Feuer" aria-label="Emoji: Feuer">https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔥" title="Feuer" aria-label="Emoji: Feuer"> plenary on 7/28: "Race, Research and the Power and Peril of Big Data" from @ruha9 @RRHDr @ShreyaKangovi & David Asch" class="img-responsive" style="max-width:100%;"/>
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔥" title="Feuer" aria-label="Emoji: Feuer">https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔥" title="Feuer" aria-label="Emoji: Feuer"> plenary on 7/28: "Race, Research and the Power and Peril of Big Data" from @ruha9 @RRHDr @ShreyaKangovi & David Asch" title="18/ Want more research on the healthy equity implications of value-based care? Check out our session @AcademyHealth virtual #ARM20 on 8/4. Also not to miss: https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔥" title="Feuer" aria-label="Emoji: Feuer">https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔥" title="Feuer" aria-label="Emoji: Feuer">https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔥" title="Feuer" aria-label="Emoji: Feuer"> plenary on 7/28: "Race, Research and the Power and Peril of Big Data" from @ruha9 @RRHDr @ShreyaKangovi & David Asch" class="img-responsive" style="max-width:100%;"/>


