1/
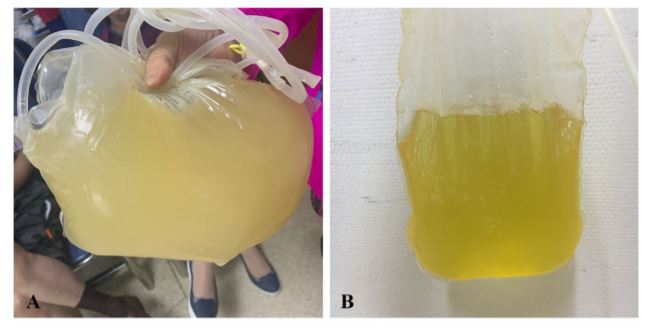
75M with ESRD on continuous ambulatory peritoneal dialysis admitted with 1 wk of abd pain and cloudy PD effluent
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧍" title="Stehende Person" aria-label="Emoji: Stehende Person">VS stable
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧍" title="Stehende Person" aria-label="Emoji: Stehende Person">VS stable
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧪" title="Test tube" aria-label="Emoji: Test tube">WBC 5k, 78%N
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧪" title="Test tube" aria-label="Emoji: Test tube">WBC 5k, 78%N
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧪" title="Test tube" aria-label="Emoji: Test tube">Effluent: WBC 1537, LDH 55, Glc 20
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧪" title="Test tube" aria-label="Emoji: Test tube">Effluent: WBC 1537, LDH 55, Glc 20
Empiric tx choice?
#MedTwitter #IDTwitter #NephTwitter
75M with ESRD on continuous ambulatory peritoneal dialysis admitted with 1 wk of abd pain and cloudy PD effluent
Empiric tx choice?
#MedTwitter #IDTwitter #NephTwitter
2/
Today’s #tweetorial = PERITONITIS, which can include several different types:
Primary
Secondary
Tertiary
PD-associated
We’ll focus on SBP and PD-associated peritonitis mostly today!
Today’s #tweetorial = PERITONITIS, which can include several different types:
Primary
Secondary
Tertiary
PD-associated
We’ll focus on SBP and PD-associated peritonitis mostly today!
3/
For primary peritonitis, think of spontaneous bacterial peritonitis (SBP) in a pt with liver cirrhosis, ascites
Clinical presentation = acute illness with fever, abd pain. May have altered mental status and hypotension as well.
Other pathogens (eg TB) rare, more indolent
For primary peritonitis, think of spontaneous bacterial peritonitis (SBP) in a pt with liver cirrhosis, ascites
Clinical presentation = acute illness with fever, abd pain. May have altered mental status and hypotension as well.
Other pathogens (eg TB) rare, more indolent
4/
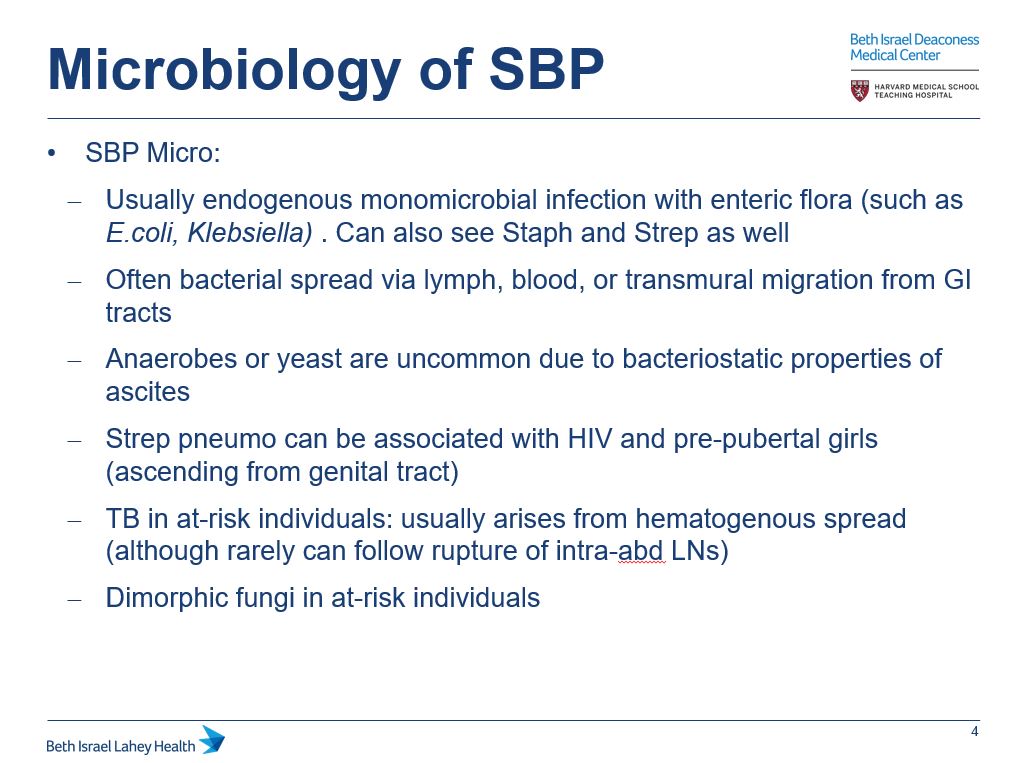
SBP is typically caused by enteric GNRs. Other orgs are less common without risk factors
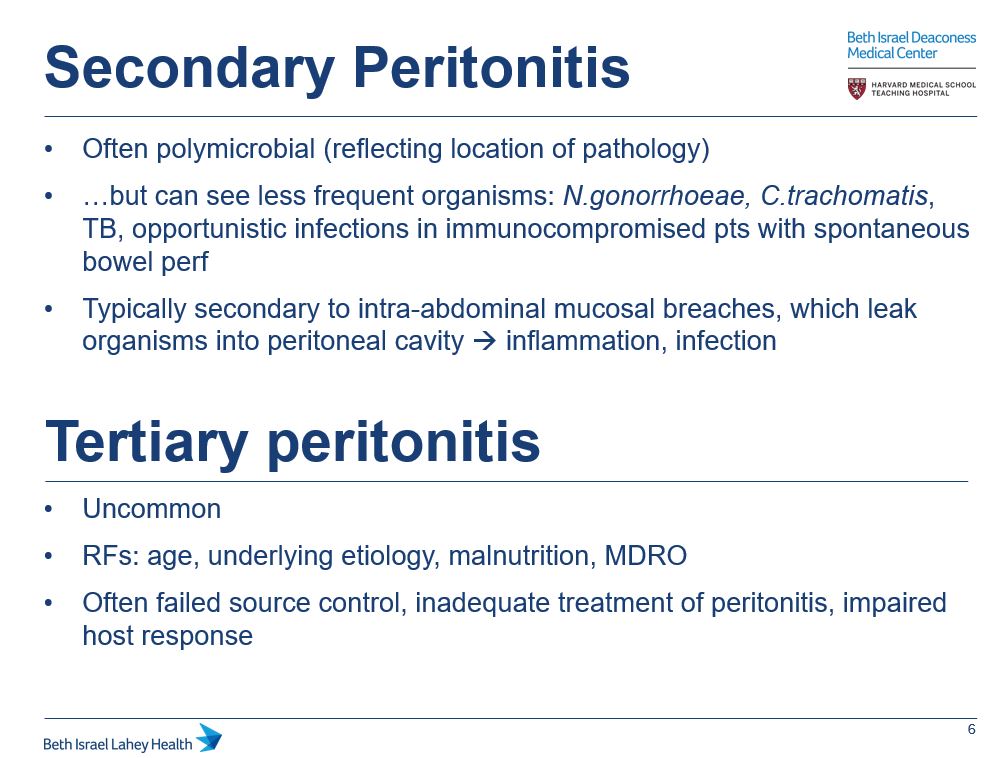
We won’t dive into secondary/tertiary peritonitis much here, but key https://abs.twimg.com/emoji/v2/... draggable="false" alt="📍" title="Runde Reißzwecke" aria-label="Emoji: Runde Reißzwecke">: these infections are typically polymicrobial, often due to break in intra-abd mucosa (abd abscess, perf viscus)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="📍" title="Runde Reißzwecke" aria-label="Emoji: Runde Reißzwecke">: these infections are typically polymicrobial, often due to break in intra-abd mucosa (abd abscess, perf viscus)
SBP is typically caused by enteric GNRs. Other orgs are less common without risk factors
We won’t dive into secondary/tertiary peritonitis much here, but key
5/
How dx peritonitis: https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧪" title="Test tube" aria-label="Emoji: Test tube">Paracentesis
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧪" title="Test tube" aria-label="Emoji: Test tube">Paracentesis
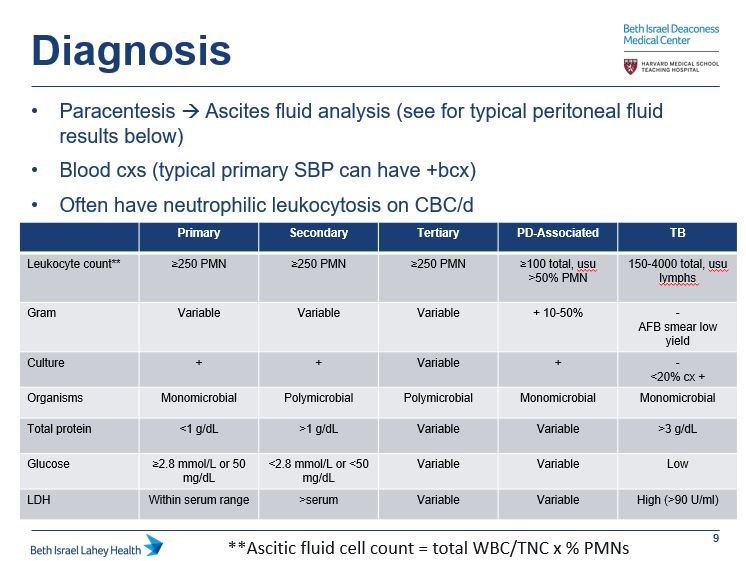
Interpreting ascites fluid is vital. See summary chart for results you would expect with diff types of peritonitis
SBP criteria and the 250 PMN cutoff is a common #TipsForNewDocs! #MedTwitter #GITwitter #medstudenttwitter
How dx peritonitis:
Interpreting ascites fluid is vital. See summary chart for results you would expect with diff types of peritonitis
SBP criteria and the 250 PMN cutoff is a common #TipsForNewDocs! #MedTwitter #GITwitter #medstudenttwitter
6/
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="👆" title="Rückhand Zeigefinger nach oben" aria-label="Emoji: Rückhand Zeigefinger nach oben">Notice PD-associated peritonitis has diff dx criteria though: WBC >100 or >50% PMNs (if short dwell, may consider >50% PMNs abnormal even with WBC <100)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👆" title="Rückhand Zeigefinger nach oben" aria-label="Emoji: Rückhand Zeigefinger nach oben">Notice PD-associated peritonitis has diff dx criteria though: WBC >100 or >50% PMNs (if short dwell, may consider >50% PMNs abnormal even with WBC <100)
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="▶️" title="Nach rechts zeigendes Dreieck" aria-label="Emoji: Nach rechts zeigendes Dreieck">May also have different clinical features:
https://abs.twimg.com/emoji/v2/... draggable="false" alt="▶️" title="Nach rechts zeigendes Dreieck" aria-label="Emoji: Nach rechts zeigendes Dreieck">May also have different clinical features:
Abd pain
Cloudy effluent/dialysate
Bacteremia+fever less common than SBP
Abd pain
Cloudy effluent/dialysate
Bacteremia+fever less common than SBP
7/
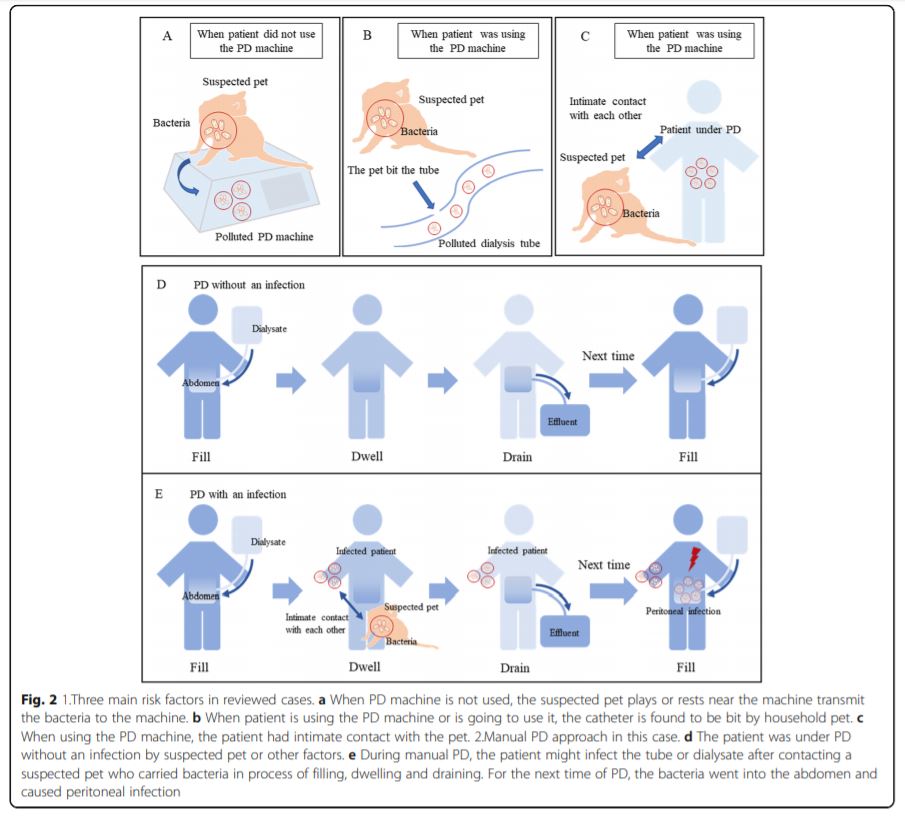
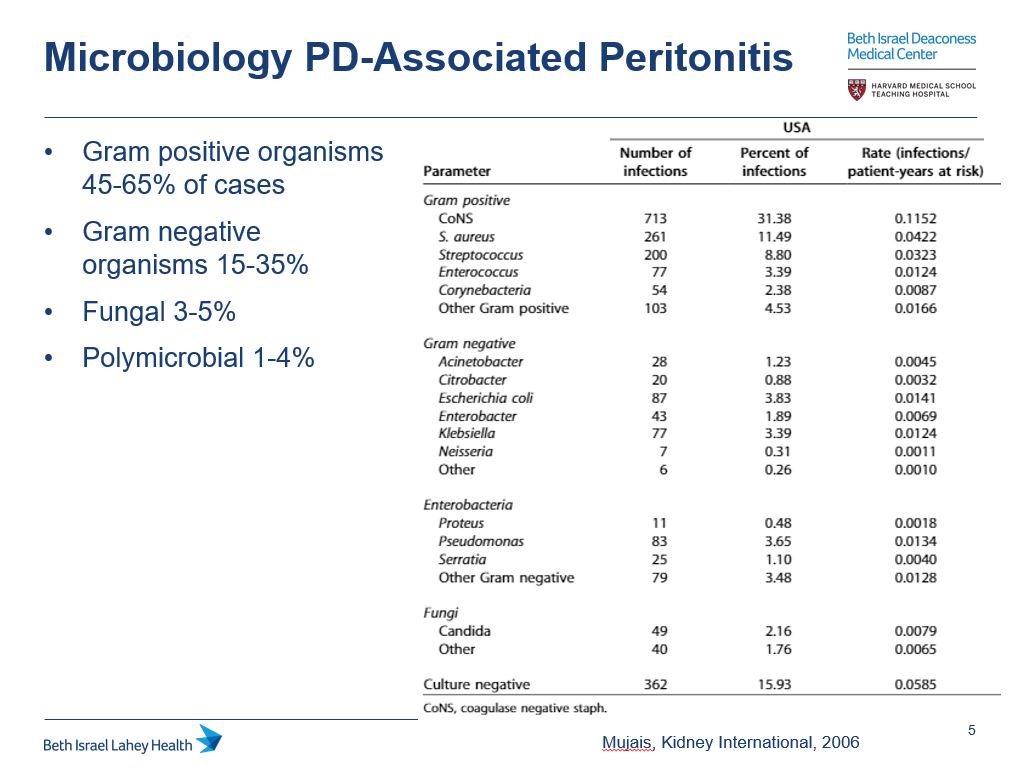
PD-associated inf can be: intraluminal contamination (connect/disconnect cath for exchange), exit site/tunnel infection, visceral (bowel bact)
Micro reflects this as pathogens often gram positive (bacterial skin contaminant). See chart/ref below
https://pubmed.ncbi.nlm.nih.gov/17080112/ ">https://pubmed.ncbi.nlm.nih.gov/17080112/...
PD-associated inf can be: intraluminal contamination (connect/disconnect cath for exchange), exit site/tunnel infection, visceral (bowel bact)
Micro reflects this as pathogens often gram positive (bacterial skin contaminant). See chart/ref below
https://pubmed.ncbi.nlm.nih.gov/17080112/ ">https://pubmed.ncbi.nlm.nih.gov/17080112/...
8/
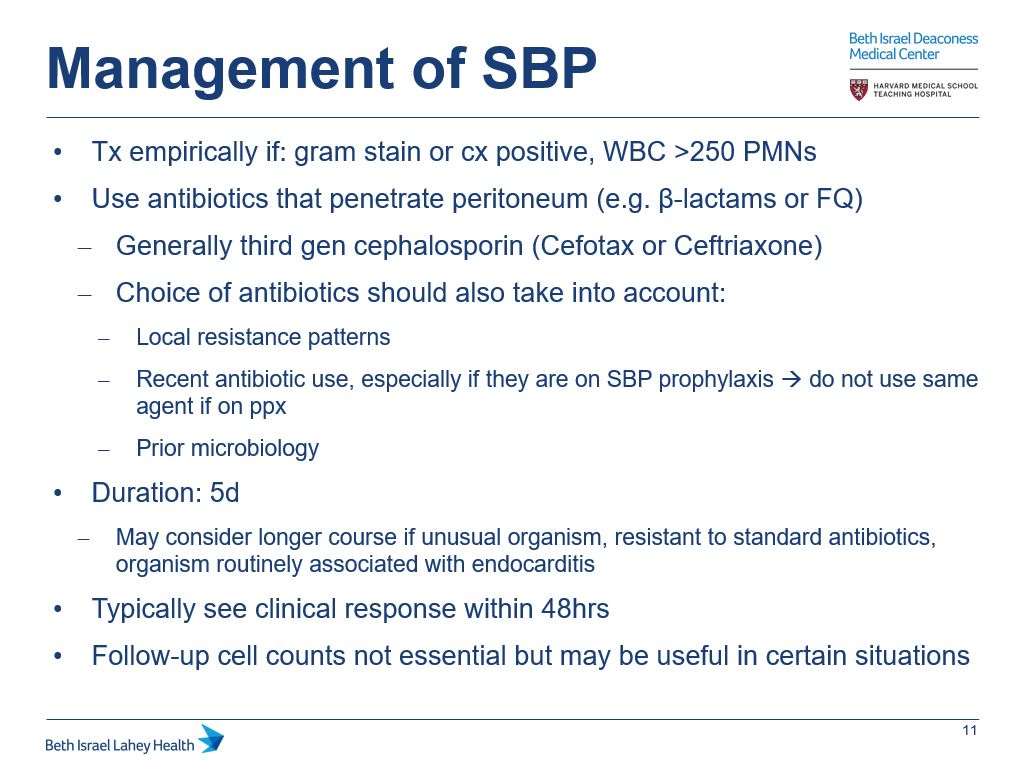
On to management, details https://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Rückhand Zeigefinger nach unten" aria-label="Emoji: Rückhand Zeigefinger nach unten">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Rückhand Zeigefinger nach unten" aria-label="Emoji: Rückhand Zeigefinger nach unten">
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔹" title="Kleine blaue Raute" aria-label="Emoji: Kleine blaue Raute">Why 5d? Here is RCT that comp& #39;d 5 v 10d of cefotax in SBP
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔹" title="Kleine blaue Raute" aria-label="Emoji: Kleine blaue Raute">Why 5d? Here is RCT that comp& #39;d 5 v 10d of cefotax in SBP https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">both grps similar cure, recurrent inf, mort https://pubmed.ncbi.nlm.nih.gov/2019378/
https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">both grps similar cure, recurrent inf, mort https://pubmed.ncbi.nlm.nih.gov/2019378/
https://pubmed.ncbi.nlm.nih.gov/2019378/&... class="Emoji" style="height:16px;" src=" https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔹" title="Kleine blaue Raute" aria-label="Emoji: Kleine blaue Raute">Many ctrs have diff approach to f/u paras, good topic to discuss with your GI colleagues @BIDMC_GI @javiervg0902
On to management, details
9/
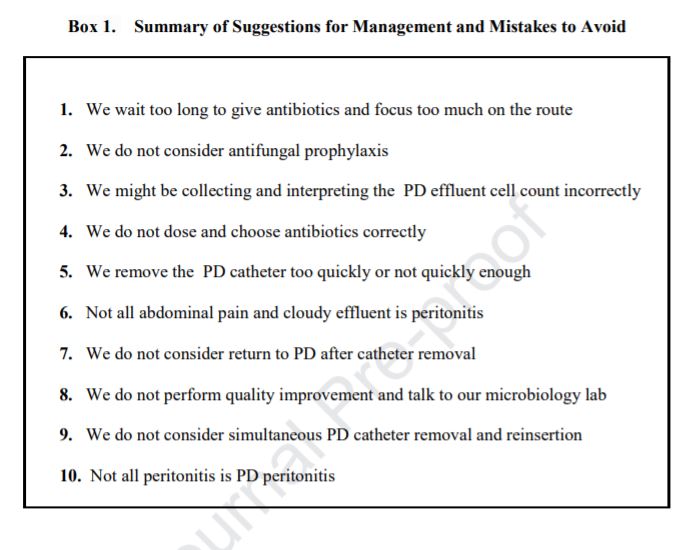
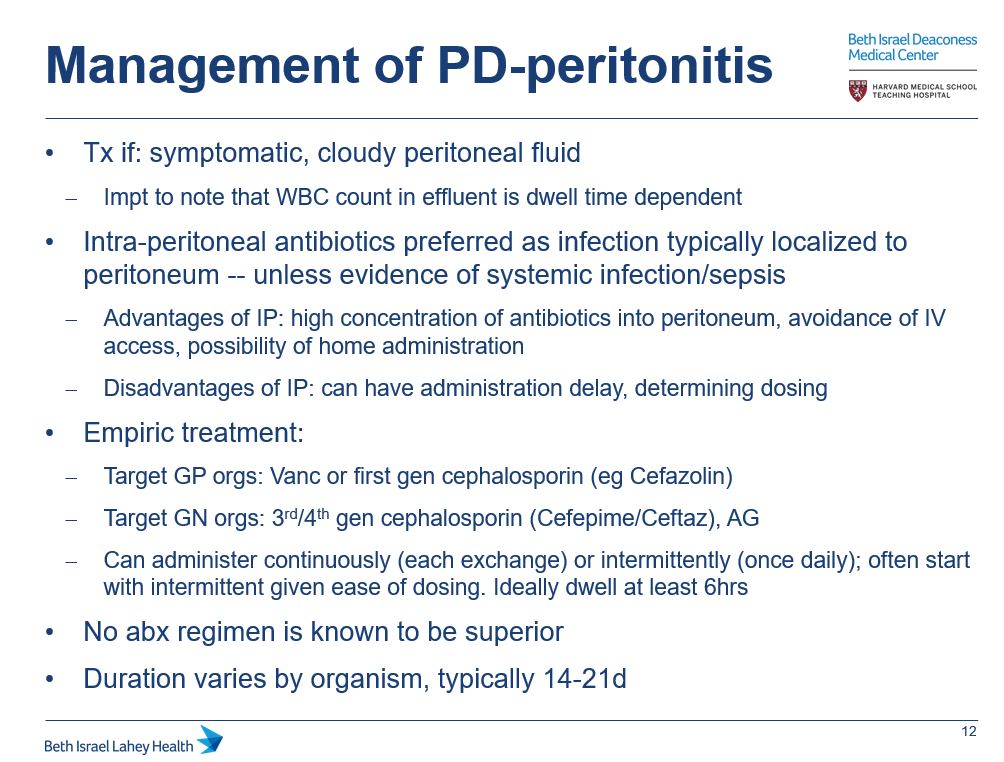
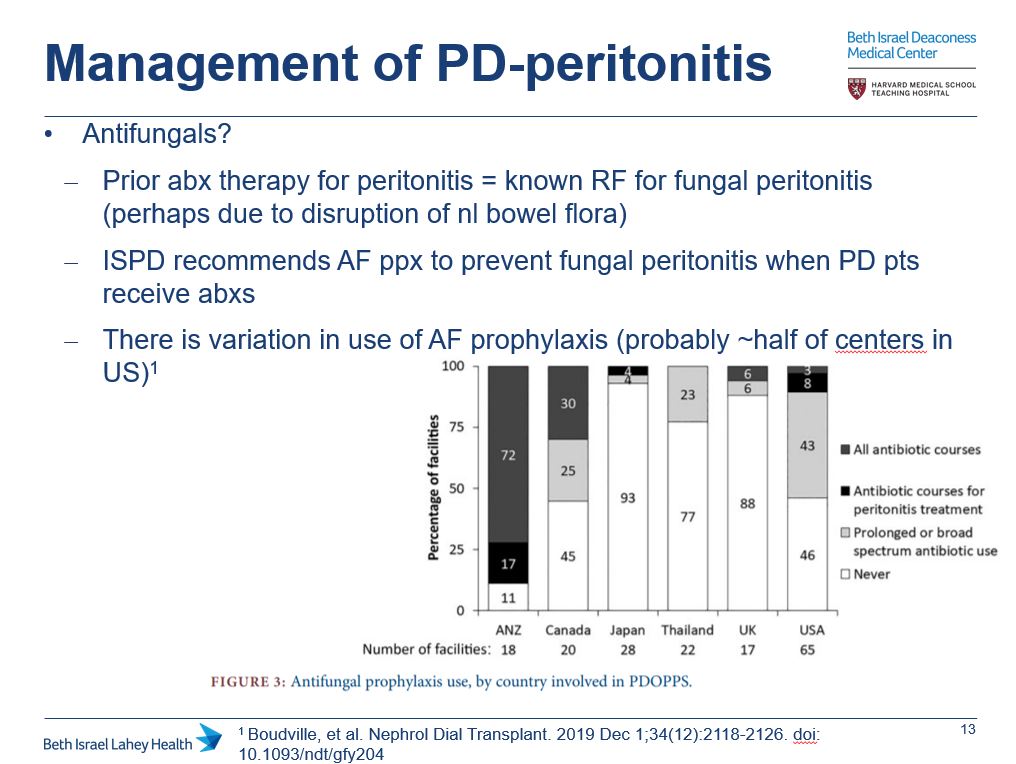
Management of PD-assoc& #39;d peritonitis is different.
Did you know that there are ISPD guidelines?
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🥔" title="Kartoffel" aria-label="Emoji: Kartoffel">For catheter inf: https://journals.sagepub.com/doi/pdf/10.3747/pdi.2016.00120
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🥔" title="Kartoffel" aria-label="Emoji: Kartoffel">For catheter inf: https://journals.sagepub.com/doi/pdf/10.3747/pdi.2016.00120
https://journals.sagepub.com/doi/pdf/1... class="Emoji" style="height:16px;" src=" https://abs.twimg.com/emoji/v2/... draggable="false" alt="🥔" title="Kartoffel" aria-label="Emoji: Kartoffel">For peritonitis:
https://journals.sagepub.com/doi/pdf/10.3747/pdi.2016.00078">https://journals.sagepub.com/doi/pdf/1...
Management of PD-assoc& #39;d peritonitis is different.
Did you know that there are ISPD guidelines?
https://journals.sagepub.com/doi/pdf/10.3747/pdi.2016.00078">https://journals.sagepub.com/doi/pdf/1...
10/
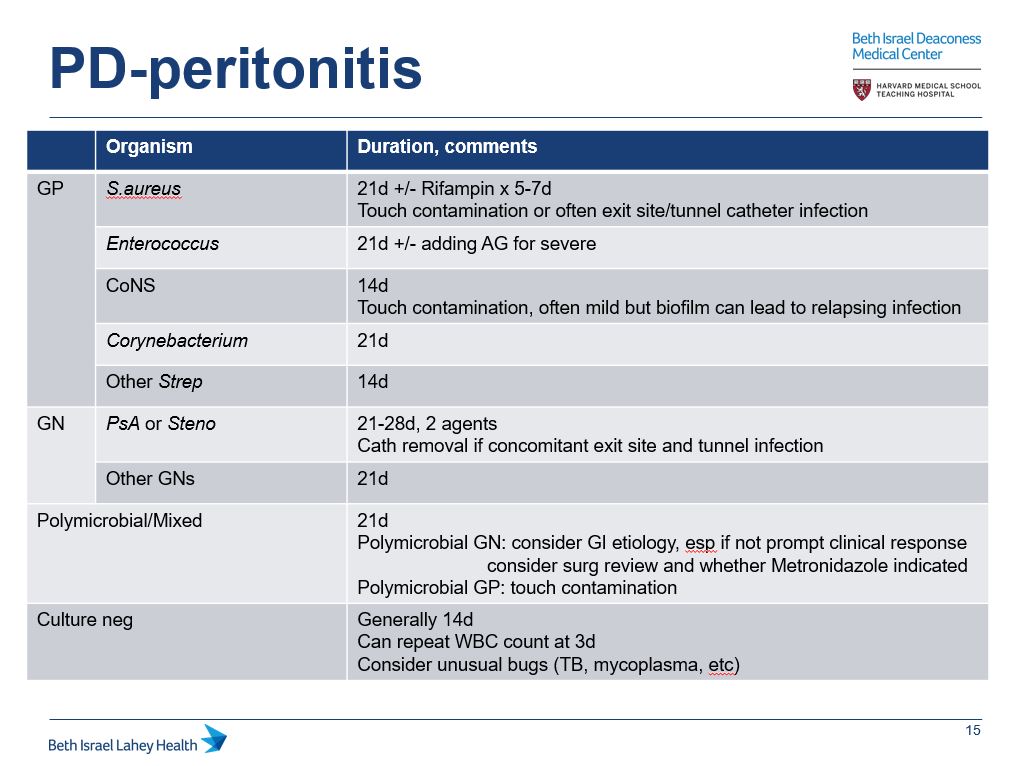
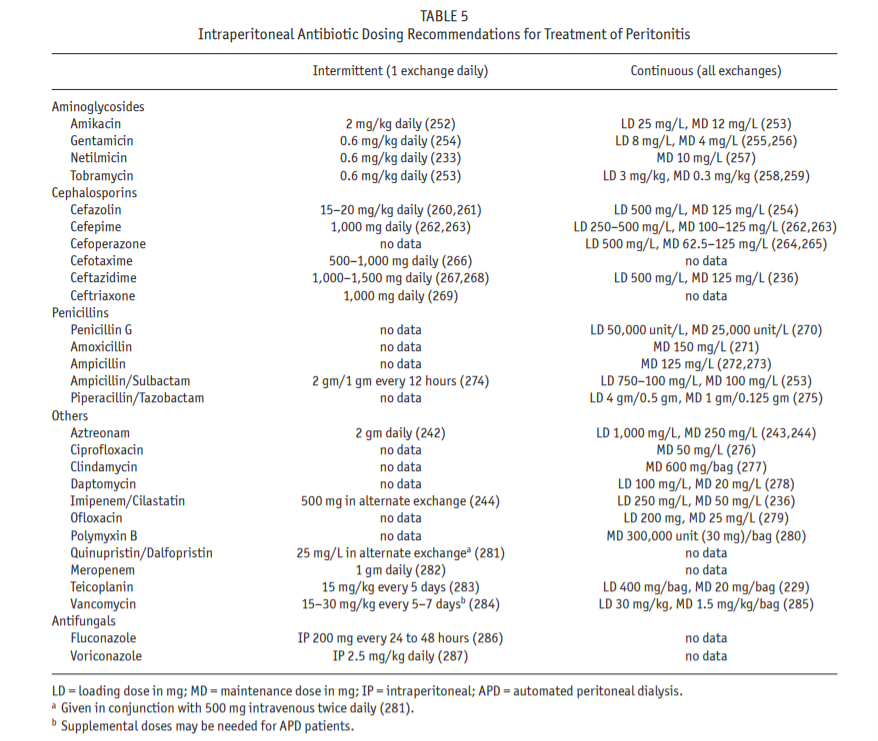
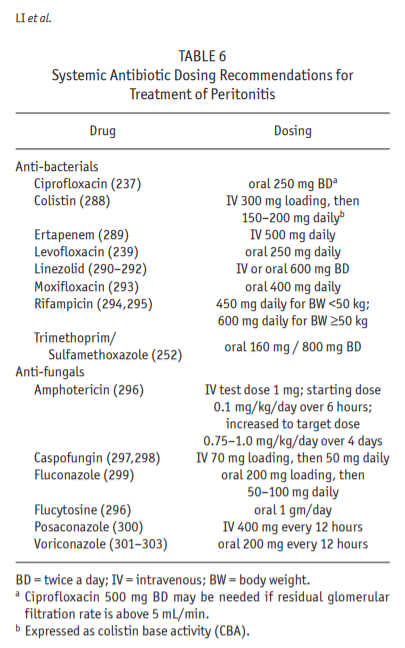
Despite https://abs.twimg.com/emoji/v2/... draggable="false" alt="👆" title="Rückhand Zeigefinger nach oben" aria-label="Emoji: Rückhand Zeigefinger nach oben">guidelines, theres variability. Here is a chart w/recs for tx by org + dosing charts
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👆" title="Rückhand Zeigefinger nach oben" aria-label="Emoji: Rückhand Zeigefinger nach oben">guidelines, theres variability. Here is a chart w/recs for tx by org + dosing charts
This is just part of the management though, #NephTwitter likely has other tips. Shout-out to @BID_NephFellows for their expertise + #PharmTwitter friends to help w/IP abx dosing!
Despite
This is just part of the management though, #NephTwitter likely has other tips. Shout-out to @BID_NephFellows for their expertise + #PharmTwitter friends to help w/IP abx dosing!
11/
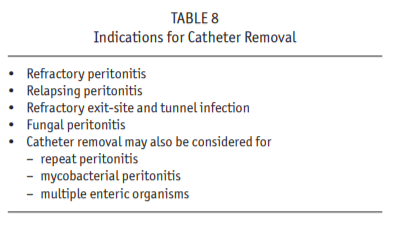
Lastly, what are indications for PD catheter removal?
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Stern mit 8 Strahlen" aria-label="Emoji: Stern mit 8 Strahlen">Refractory perit
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Stern mit 8 Strahlen" aria-label="Emoji: Stern mit 8 Strahlen">Refractory perit
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Stern mit 8 Strahlen" aria-label="Emoji: Stern mit 8 Strahlen">Relapsing perit
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Stern mit 8 Strahlen" aria-label="Emoji: Stern mit 8 Strahlen">Relapsing perit
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Stern mit 8 Strahlen" aria-label="Emoji: Stern mit 8 Strahlen">Refractory catheter inf
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Stern mit 8 Strahlen" aria-label="Emoji: Stern mit 8 Strahlen">Refractory catheter inf
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Stern mit 8 Strahlen" aria-label="Emoji: Stern mit 8 Strahlen">Fungal peritonitis
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Stern mit 8 Strahlen" aria-label="Emoji: Stern mit 8 Strahlen">Fungal peritonitis
Strongly consider with:
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Stern mit 8 Strahlen" aria-label="Emoji: Stern mit 8 Strahlen">Mycobact or polymicrobial inf
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Stern mit 8 Strahlen" aria-label="Emoji: Stern mit 8 Strahlen">Mycobact or polymicrobial inf
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Stern mit 8 Strahlen" aria-label="Emoji: Stern mit 8 Strahlen">Association with intra-abd pathology
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Stern mit 8 Strahlen" aria-label="Emoji: Stern mit 8 Strahlen">Association with intra-abd pathology
Lastly, what are indications for PD catheter removal?
Strongly consider with:
12/
PD-assoc& #39;d peritonitis is more complex than fits in this thread, a recent publ thinking about management: https://www.sciencedirect.com/science/article/pii/S2590059520301321
Here& #39;s">https://www.sciencedirect.com/science/a... case/review fr initial poll. Don& #39;t forget pet-associated PD-peritonitis if you have an unusual bug! https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7081570/">https://www.ncbi.nlm.nih.gov/pmc/artic...
PD-assoc& #39;d peritonitis is more complex than fits in this thread, a recent publ thinking about management: https://www.sciencedirect.com/science/article/pii/S2590059520301321
Here& #39;s">https://www.sciencedirect.com/science/a... case/review fr initial poll. Don& #39;t forget pet-associated PD-peritonitis if you have an unusual bug! https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7081570/">https://www.ncbi.nlm.nih.gov/pmc/artic...

 Read on Twitter
Read on Twitter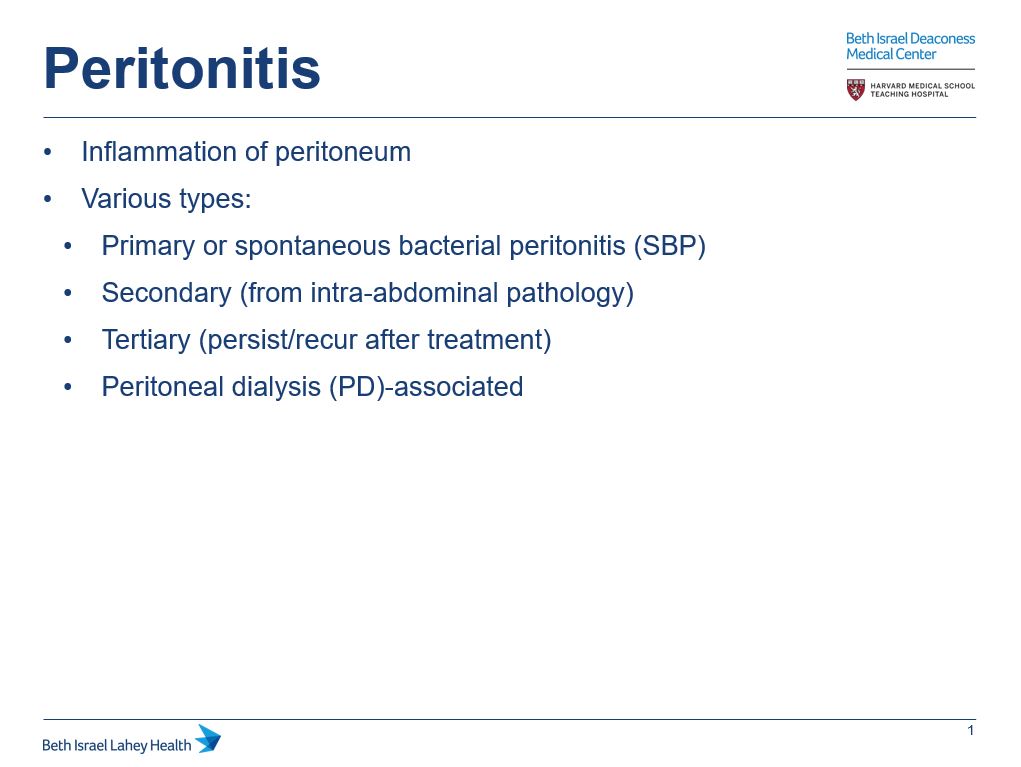
 : these infections are typically polymicrobial, often due to break in intra-abd mucosa (abd abscess, perf viscus)" title="4/SBP is typically caused by enteric GNRs. Other orgs are less common without risk factorsWe won’t dive into secondary/tertiary peritonitis much here, but key https://abs.twimg.com/emoji/v2/... draggable="false" alt="📍" title="Runde Reißzwecke" aria-label="Emoji: Runde Reißzwecke">: these infections are typically polymicrobial, often due to break in intra-abd mucosa (abd abscess, perf viscus)">
: these infections are typically polymicrobial, often due to break in intra-abd mucosa (abd abscess, perf viscus)" title="4/SBP is typically caused by enteric GNRs. Other orgs are less common without risk factorsWe won’t dive into secondary/tertiary peritonitis much here, but key https://abs.twimg.com/emoji/v2/... draggable="false" alt="📍" title="Runde Reißzwecke" aria-label="Emoji: Runde Reißzwecke">: these infections are typically polymicrobial, often due to break in intra-abd mucosa (abd abscess, perf viscus)">
 : these infections are typically polymicrobial, often due to break in intra-abd mucosa (abd abscess, perf viscus)" title="4/SBP is typically caused by enteric GNRs. Other orgs are less common without risk factorsWe won’t dive into secondary/tertiary peritonitis much here, but key https://abs.twimg.com/emoji/v2/... draggable="false" alt="📍" title="Runde Reißzwecke" aria-label="Emoji: Runde Reißzwecke">: these infections are typically polymicrobial, often due to break in intra-abd mucosa (abd abscess, perf viscus)">
: these infections are typically polymicrobial, often due to break in intra-abd mucosa (abd abscess, perf viscus)" title="4/SBP is typically caused by enteric GNRs. Other orgs are less common without risk factorsWe won’t dive into secondary/tertiary peritonitis much here, but key https://abs.twimg.com/emoji/v2/... draggable="false" alt="📍" title="Runde Reißzwecke" aria-label="Emoji: Runde Reißzwecke">: these infections are typically polymicrobial, often due to break in intra-abd mucosa (abd abscess, perf viscus)">
 ParacentesisInterpreting ascites fluid is vital. See summary chart for results you would expect with diff types of peritonitisSBP criteria and the 250 PMN cutoff is a common #TipsForNewDocs! #MedTwitter #GITwitter #medstudenttwitter" title="5/How dx peritonitis: https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧪" title="Test tube" aria-label="Emoji: Test tube">ParacentesisInterpreting ascites fluid is vital. See summary chart for results you would expect with diff types of peritonitisSBP criteria and the 250 PMN cutoff is a common #TipsForNewDocs! #MedTwitter #GITwitter #medstudenttwitter" class="img-responsive" style="max-width:100%;"/>
ParacentesisInterpreting ascites fluid is vital. See summary chart for results you would expect with diff types of peritonitisSBP criteria and the 250 PMN cutoff is a common #TipsForNewDocs! #MedTwitter #GITwitter #medstudenttwitter" title="5/How dx peritonitis: https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧪" title="Test tube" aria-label="Emoji: Test tube">ParacentesisInterpreting ascites fluid is vital. See summary chart for results you would expect with diff types of peritonitisSBP criteria and the 250 PMN cutoff is a common #TipsForNewDocs! #MedTwitter #GITwitter #medstudenttwitter" class="img-responsive" style="max-width:100%;"/>
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔹" title="Kleine blaue Raute" aria-label="Emoji: Kleine blaue Raute">Why 5d? Here is RCT that comp& #39;d 5 v 10d of cefotax in SBPhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">both grps similar cure, recurrent inf, mort https://pubmed.ncbi.nlm.nih.gov/2019378/&... class="Emoji" style="height:16px;" src=" " title="8/On to management, detailshttps://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Rückhand Zeigefinger nach unten" aria-label="Emoji: Rückhand Zeigefinger nach unten">https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔹" title="Kleine blaue Raute" aria-label="Emoji: Kleine blaue Raute">Why 5d? Here is RCT that comp& #39;d 5 v 10d of cefotax in SBPhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">both grps similar cure, recurrent inf, mort https://pubmed.ncbi.nlm.nih.gov/2019378/&... class="Emoji" style="height:16px;" src=" " class="img-responsive" style="max-width:100%;"/>
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔹" title="Kleine blaue Raute" aria-label="Emoji: Kleine blaue Raute">Why 5d? Here is RCT that comp& #39;d 5 v 10d of cefotax in SBPhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">both grps similar cure, recurrent inf, mort https://pubmed.ncbi.nlm.nih.gov/2019378/&... class="Emoji" style="height:16px;" src=" " title="8/On to management, detailshttps://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Rückhand Zeigefinger nach unten" aria-label="Emoji: Rückhand Zeigefinger nach unten">https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔹" title="Kleine blaue Raute" aria-label="Emoji: Kleine blaue Raute">Why 5d? Here is RCT that comp& #39;d 5 v 10d of cefotax in SBPhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">both grps similar cure, recurrent inf, mort https://pubmed.ncbi.nlm.nih.gov/2019378/&... class="Emoji" style="height:16px;" src=" " class="img-responsive" style="max-width:100%;"/>
 For catheter inf: https://journals.sagepub.com/doi/pdf/1... class="Emoji" style="height:16px;" src=" " title="9/Management of PD-assoc& #39;d peritonitis is different. Did you know that there are ISPD guidelines?https://abs.twimg.com/emoji/v2/... draggable="false" alt="🥔" title="Kartoffel" aria-label="Emoji: Kartoffel">For catheter inf: https://journals.sagepub.com/doi/pdf/1... class="Emoji" style="height:16px;" src=" ">
For catheter inf: https://journals.sagepub.com/doi/pdf/1... class="Emoji" style="height:16px;" src=" " title="9/Management of PD-assoc& #39;d peritonitis is different. Did you know that there are ISPD guidelines?https://abs.twimg.com/emoji/v2/... draggable="false" alt="🥔" title="Kartoffel" aria-label="Emoji: Kartoffel">For catheter inf: https://journals.sagepub.com/doi/pdf/1... class="Emoji" style="height:16px;" src=" ">
 For catheter inf: https://journals.sagepub.com/doi/pdf/1... class="Emoji" style="height:16px;" src=" " title="9/Management of PD-assoc& #39;d peritonitis is different. Did you know that there are ISPD guidelines?https://abs.twimg.com/emoji/v2/... draggable="false" alt="🥔" title="Kartoffel" aria-label="Emoji: Kartoffel">For catheter inf: https://journals.sagepub.com/doi/pdf/1... class="Emoji" style="height:16px;" src=" ">
For catheter inf: https://journals.sagepub.com/doi/pdf/1... class="Emoji" style="height:16px;" src=" " title="9/Management of PD-assoc& #39;d peritonitis is different. Did you know that there are ISPD guidelines?https://abs.twimg.com/emoji/v2/... draggable="false" alt="🥔" title="Kartoffel" aria-label="Emoji: Kartoffel">For catheter inf: https://journals.sagepub.com/doi/pdf/1... class="Emoji" style="height:16px;" src=" ">
 For catheter inf: https://journals.sagepub.com/doi/pdf/1... class="Emoji" style="height:16px;" src=" " title="9/Management of PD-assoc& #39;d peritonitis is different. Did you know that there are ISPD guidelines?https://abs.twimg.com/emoji/v2/... draggable="false" alt="🥔" title="Kartoffel" aria-label="Emoji: Kartoffel">For catheter inf: https://journals.sagepub.com/doi/pdf/1... class="Emoji" style="height:16px;" src=" ">
For catheter inf: https://journals.sagepub.com/doi/pdf/1... class="Emoji" style="height:16px;" src=" " title="9/Management of PD-assoc& #39;d peritonitis is different. Did you know that there are ISPD guidelines?https://abs.twimg.com/emoji/v2/... draggable="false" alt="🥔" title="Kartoffel" aria-label="Emoji: Kartoffel">For catheter inf: https://journals.sagepub.com/doi/pdf/1... class="Emoji" style="height:16px;" src=" ">
 guidelines, theres variability. Here is a chart w/recs for tx by org + dosing chartsThis is just part of the management though, #NephTwitter likely has other tips. Shout-out to @BID_NephFellows for their expertise + #PharmTwitter friends to help w/IP abx dosing!" title="10/Despite https://abs.twimg.com/emoji/v2/... draggable="false" alt="👆" title="Rückhand Zeigefinger nach oben" aria-label="Emoji: Rückhand Zeigefinger nach oben">guidelines, theres variability. Here is a chart w/recs for tx by org + dosing chartsThis is just part of the management though, #NephTwitter likely has other tips. Shout-out to @BID_NephFellows for their expertise + #PharmTwitter friends to help w/IP abx dosing!">
guidelines, theres variability. Here is a chart w/recs for tx by org + dosing chartsThis is just part of the management though, #NephTwitter likely has other tips. Shout-out to @BID_NephFellows for their expertise + #PharmTwitter friends to help w/IP abx dosing!" title="10/Despite https://abs.twimg.com/emoji/v2/... draggable="false" alt="👆" title="Rückhand Zeigefinger nach oben" aria-label="Emoji: Rückhand Zeigefinger nach oben">guidelines, theres variability. Here is a chart w/recs for tx by org + dosing chartsThis is just part of the management though, #NephTwitter likely has other tips. Shout-out to @BID_NephFellows for their expertise + #PharmTwitter friends to help w/IP abx dosing!">
 guidelines, theres variability. Here is a chart w/recs for tx by org + dosing chartsThis is just part of the management though, #NephTwitter likely has other tips. Shout-out to @BID_NephFellows for their expertise + #PharmTwitter friends to help w/IP abx dosing!" title="10/Despite https://abs.twimg.com/emoji/v2/... draggable="false" alt="👆" title="Rückhand Zeigefinger nach oben" aria-label="Emoji: Rückhand Zeigefinger nach oben">guidelines, theres variability. Here is a chart w/recs for tx by org + dosing chartsThis is just part of the management though, #NephTwitter likely has other tips. Shout-out to @BID_NephFellows for their expertise + #PharmTwitter friends to help w/IP abx dosing!">
guidelines, theres variability. Here is a chart w/recs for tx by org + dosing chartsThis is just part of the management though, #NephTwitter likely has other tips. Shout-out to @BID_NephFellows for their expertise + #PharmTwitter friends to help w/IP abx dosing!" title="10/Despite https://abs.twimg.com/emoji/v2/... draggable="false" alt="👆" title="Rückhand Zeigefinger nach oben" aria-label="Emoji: Rückhand Zeigefinger nach oben">guidelines, theres variability. Here is a chart w/recs for tx by org + dosing chartsThis is just part of the management though, #NephTwitter likely has other tips. Shout-out to @BID_NephFellows for their expertise + #PharmTwitter friends to help w/IP abx dosing!">
 guidelines, theres variability. Here is a chart w/recs for tx by org + dosing chartsThis is just part of the management though, #NephTwitter likely has other tips. Shout-out to @BID_NephFellows for their expertise + #PharmTwitter friends to help w/IP abx dosing!" title="10/Despite https://abs.twimg.com/emoji/v2/... draggable="false" alt="👆" title="Rückhand Zeigefinger nach oben" aria-label="Emoji: Rückhand Zeigefinger nach oben">guidelines, theres variability. Here is a chart w/recs for tx by org + dosing chartsThis is just part of the management though, #NephTwitter likely has other tips. Shout-out to @BID_NephFellows for their expertise + #PharmTwitter friends to help w/IP abx dosing!">
guidelines, theres variability. Here is a chart w/recs for tx by org + dosing chartsThis is just part of the management though, #NephTwitter likely has other tips. Shout-out to @BID_NephFellows for their expertise + #PharmTwitter friends to help w/IP abx dosing!" title="10/Despite https://abs.twimg.com/emoji/v2/... draggable="false" alt="👆" title="Rückhand Zeigefinger nach oben" aria-label="Emoji: Rückhand Zeigefinger nach oben">guidelines, theres variability. Here is a chart w/recs for tx by org + dosing chartsThis is just part of the management though, #NephTwitter likely has other tips. Shout-out to @BID_NephFellows for their expertise + #PharmTwitter friends to help w/IP abx dosing!">
 Refractory perithttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Stern mit 8 Strahlen" aria-label="Emoji: Stern mit 8 Strahlen">Relapsing perithttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Stern mit 8 Strahlen" aria-label="Emoji: Stern mit 8 Strahlen">Refractory catheter infhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Stern mit 8 Strahlen" aria-label="Emoji: Stern mit 8 Strahlen">Fungal peritonitisStrongly consider with: https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Stern mit 8 Strahlen" aria-label="Emoji: Stern mit 8 Strahlen">Mycobact or polymicrobial infhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Stern mit 8 Strahlen" aria-label="Emoji: Stern mit 8 Strahlen">Association with intra-abd pathology" title="11/Lastly, what are indications for PD catheter removal?https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Stern mit 8 Strahlen" aria-label="Emoji: Stern mit 8 Strahlen">Refractory perithttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Stern mit 8 Strahlen" aria-label="Emoji: Stern mit 8 Strahlen">Relapsing perithttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Stern mit 8 Strahlen" aria-label="Emoji: Stern mit 8 Strahlen">Refractory catheter infhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Stern mit 8 Strahlen" aria-label="Emoji: Stern mit 8 Strahlen">Fungal peritonitisStrongly consider with: https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Stern mit 8 Strahlen" aria-label="Emoji: Stern mit 8 Strahlen">Mycobact or polymicrobial infhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Stern mit 8 Strahlen" aria-label="Emoji: Stern mit 8 Strahlen">Association with intra-abd pathology" class="img-responsive" style="max-width:100%;"/>
Refractory perithttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Stern mit 8 Strahlen" aria-label="Emoji: Stern mit 8 Strahlen">Relapsing perithttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Stern mit 8 Strahlen" aria-label="Emoji: Stern mit 8 Strahlen">Refractory catheter infhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Stern mit 8 Strahlen" aria-label="Emoji: Stern mit 8 Strahlen">Fungal peritonitisStrongly consider with: https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Stern mit 8 Strahlen" aria-label="Emoji: Stern mit 8 Strahlen">Mycobact or polymicrobial infhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Stern mit 8 Strahlen" aria-label="Emoji: Stern mit 8 Strahlen">Association with intra-abd pathology" title="11/Lastly, what are indications for PD catheter removal?https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Stern mit 8 Strahlen" aria-label="Emoji: Stern mit 8 Strahlen">Refractory perithttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Stern mit 8 Strahlen" aria-label="Emoji: Stern mit 8 Strahlen">Relapsing perithttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Stern mit 8 Strahlen" aria-label="Emoji: Stern mit 8 Strahlen">Refractory catheter infhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Stern mit 8 Strahlen" aria-label="Emoji: Stern mit 8 Strahlen">Fungal peritonitisStrongly consider with: https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Stern mit 8 Strahlen" aria-label="Emoji: Stern mit 8 Strahlen">Mycobact or polymicrobial infhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Stern mit 8 Strahlen" aria-label="Emoji: Stern mit 8 Strahlen">Association with intra-abd pathology" class="img-responsive" style="max-width:100%;"/>