(1/24)*De-mystifying Hepatic waveforms*
Welcome to Part 2. Now that we have gone through the basics:( https://twitter.com/msenussiMD/status/1278480975643709440).">https://twitter.com/msenussiM... Time for a deep dive where we can start to decipher the important clinical information we need to apply at the bedside #showmethewaveforms #shocksquad
Welcome to Part 2. Now that we have gone through the basics:( https://twitter.com/msenussiMD/status/1278480975643709440).">https://twitter.com/msenussiM... Time for a deep dive where we can start to decipher the important clinical information we need to apply at the bedside #showmethewaveforms #shocksquad
(2/24)We must acquaint ourselves with the different guises that HV waveforms may appear, they can be
- biphasic and tetrainflectional
- tetraphasic and tetrainflectional
- Increased antegrade flow (S and D magnitude)
- Increased retrograde flow (A-reversal, SR, DR)
See https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">
- biphasic and tetrainflectional
- tetraphasic and tetrainflectional
- Increased antegrade flow (S and D magnitude)
- Increased retrograde flow (A-reversal, SR, DR)
See
(3/24)The fun doesn& #39;t stop there! We all know how the atrium augments flow to the ventricle. With atrial relaxation (analogous to x-descent on JVP) that downward deflection helps increase forward flow during systole. With TV closure, you can see a notched S-wave (S1, S2).
(4/24)Now that we understand what falls under the confines of "normal" for these waveforms. Lets systematically look at different physiological and pathological states and their effects on
1. Atrial reversal wave
2. S-wave
3. D-wave
1. Atrial reversal wave
2. S-wave
3. D-wave
(5/24)** Atrial Reversal Wave (Ar)**: this is the first retrograde deflection that occurs after the p-wave.
1. Diminished or absent
2. Prominent all the time
3. Prominent some times
4. Biphasic Ar wave
1. Diminished or absent
2. Prominent all the time
3. Prominent some times
4. Biphasic Ar wave
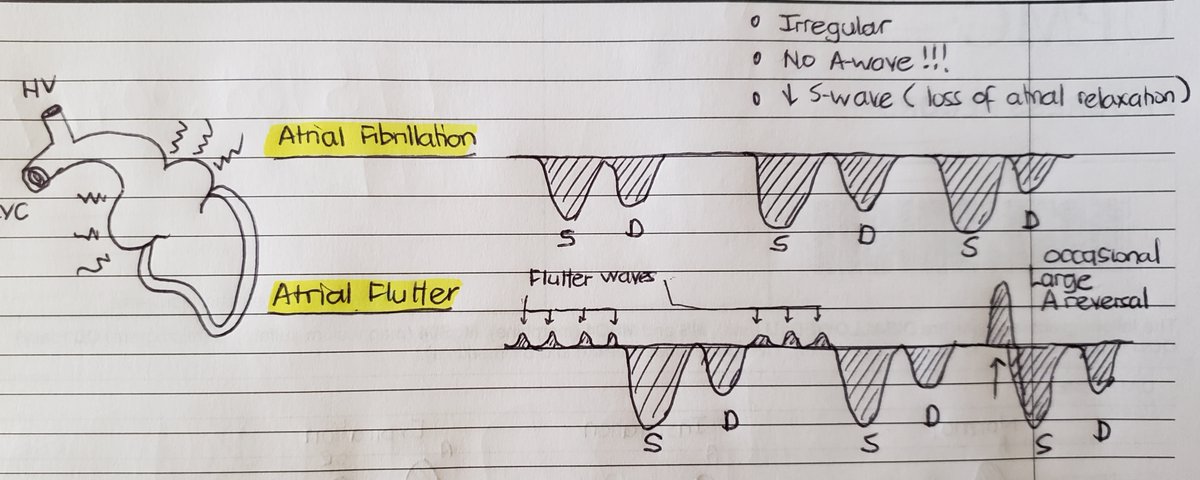
(6/24)Diminished/absent Ar wave
- Afib: no Ar wave, w/o atrial relaxation, S wave magnitude https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">
- Liver parenchymal disease ( low compliance thus appears as monophasic aninflectional flow)
- Aflutter: f-waves, if flutter wave occurs with TV closure https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">big Ar wave!
https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">big Ar wave!
- Afib: no Ar wave, w/o atrial relaxation, S wave magnitude
- Liver parenchymal disease ( low compliance thus appears as monophasic aninflectional flow)
- Aflutter: f-waves, if flutter wave occurs with TV closure
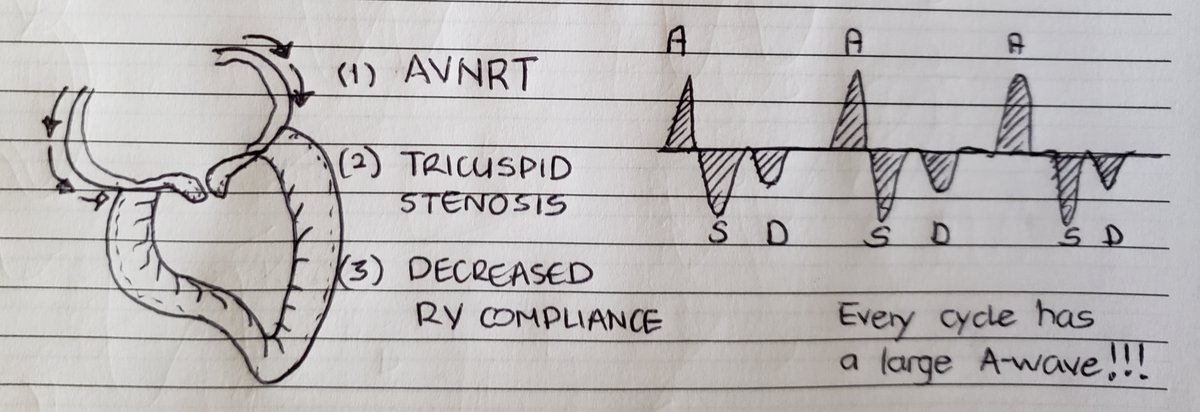
(7/24) Prominent Ar wave all the time: think fixed obstruction! or conduction abnormality that leads to atrial contraction against a closed TV all the time.
(8/24)Prominent Ar wave sometimes:
- expiration can always increase reversal waves
- PVCs and 3rd AV Block w occasional atrial contraction against closed TV
- insp https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">venous return
https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">venous return https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> more reversal waves in pt with
https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> more reversal waves in pt with  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">RV compliance
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">RV compliance
- expiration can always increase reversal waves
- PVCs and 3rd AV Block w occasional atrial contraction against closed TV
- insp
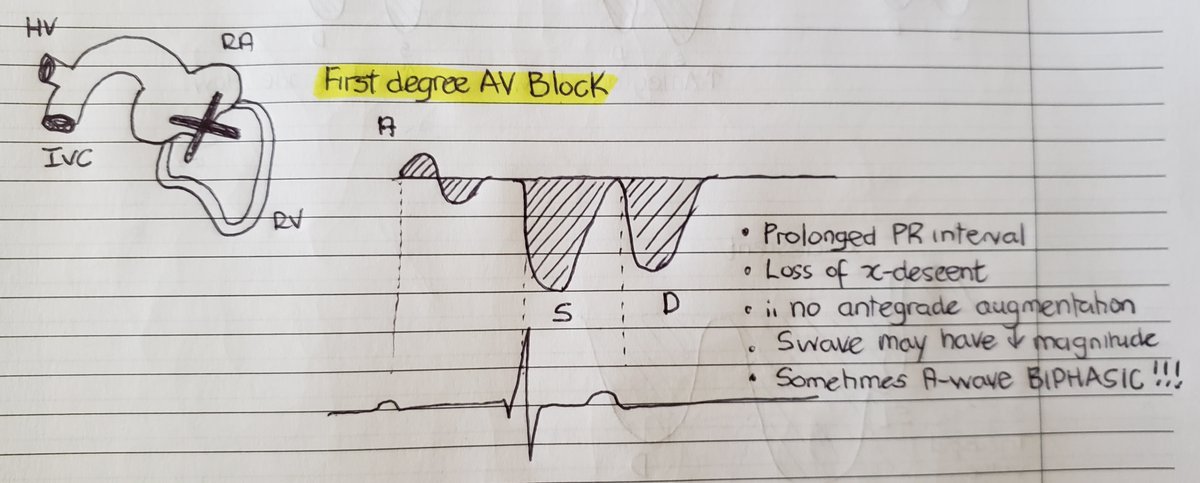
(9/24)Biphasic Ar wave: this is a rarity but can be seen. due to prolonged PR interval. The Ar wave may become biphasic. Another downstream effect is loss of x descent which translates to smaller S-waves.
(10/24) **S-wave**: represents antegrade flow spanning from the R-wave to end of the T-wave. This has been the major focus of many and I feel most misunderstood ...but lets unwrap!
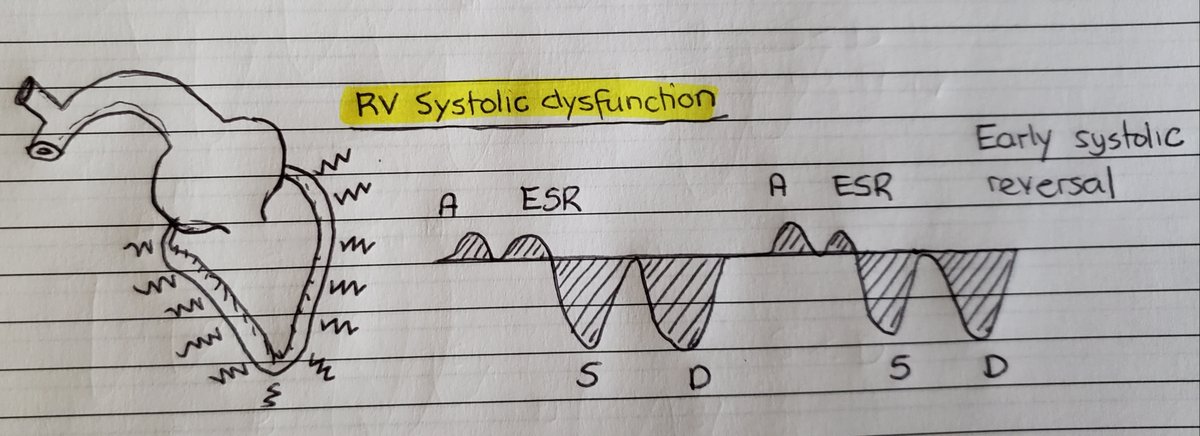
(11/24) Normally S>D, with progressive volume and RV dysfunction its clear that the S-wave diminishes and ultimately reverses. This is the spectrum that we are accustomed to but is an over-simplification nonetheless.
(12/24) The S-wave can be reduced due to any of the following or a combination thereof:
1. Lack of atrial participation
2. Excess volume in RA (think TR)
3. RV systolic dysfunction
Therefore it is not always a congestive parameter! This is where I see many falter.
1. Lack of atrial participation
2. Excess volume in RA (think TR)
3. RV systolic dysfunction
Therefore it is not always a congestive parameter! This is where I see many falter.
(13/24) For ex., In atrial flutter or atrial fibrillation, the lack of an atrial relaxation phase which normally creates an x descent and amplifies antegrade systolic flow is no longer present. Therefore, s-waves are diminished! This is not a volume issue even though S<D.
(14/24) In pts with RV systolic dysfunction, this is manifested as an early systolic flow reversal (ESR) with a late small S-wave. Its early because lack of downward RV movement.
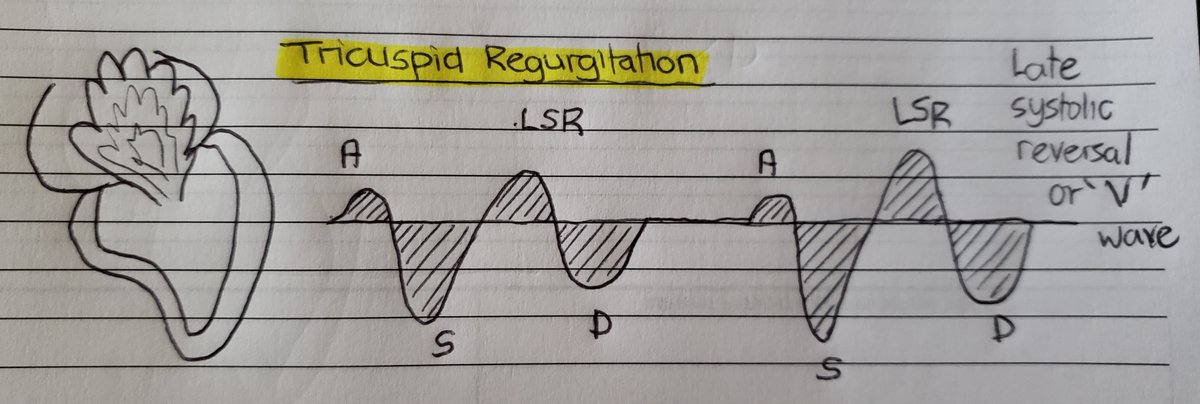
(15/24) However in TR, as systole progresses more volume builds up in the RA and therefore flow reversal is expected to be late! Known as S-reversal wave or V-wave.
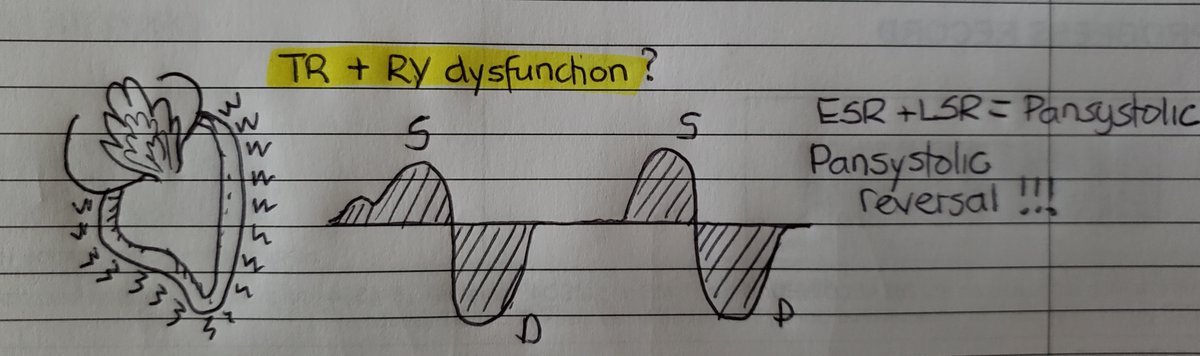
(16/24) But wait one darn minute! Don& #39;t these pathological states often coexist? Yes, indeed and when they overlap it becomes pansystolic (early and late combined). Spells bad news for the patient!
(17/24)In fact , it is important to realize that 1. loss of atrial kick 2. TR 3. RV systolic dysfunction in combination can all reduce the S-wave to some extent but you need significant TR and RV dysfunction for systolic flow reversal!
(18/24)By the time patients have systolic flow reversal its quite obvious clinically and this doesn& #39;t add much. However, this is important and hepful as a de-resuscitative tool. In other words, volume removal to achieve better waveforms.
(19/24) **D-wave** Antegrade flow that occurs during diastole (end of T-wave to R-wave).
1. Decreased with https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">RV relaxation (ex. RVH)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">RV relaxation (ex. RVH)
2. Changes in constriction
3. Changes in restriction
1. Decreased with
2. Changes in constriction
3. Changes in restriction
(20/24)Pericardial constriction is like a Rube Goldberg machine...so many things that come into play.
1. Pericardial constraint prevents IT pressure changes to be transmitted to the cardiac chambers
2. Respiratory variation in ventricular filling
3. Ventricular interdependence
1. Pericardial constraint prevents IT pressure changes to be transmitted to the cardiac chambers
2. Respiratory variation in ventricular filling
3. Ventricular interdependence
(21/24)In constriction, with expiration, IT pressure is not transmitted, thus mitral inflow increases, LV bulges to the right, along with less venous return-> exp diastolic flow reversal.
(22/24) In restriction, with inspiration there is increased venous return and given the poor RV compliance  https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> inspiratory diastolic flow reversal!
https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> inspiratory diastolic flow reversal!
(23/24)So in summary, these waveforms provide an incredible amount of information! I use it like a barometer which gives me accurate info on hemodynamic conditions. A JVP of 8 (just a number) has little meaning if not interpreted in the context of the waveforms.
(24/24) Good movies are always in trilogies so stay tuned for the final installment. We will go over real cases, step by step and see how you can seamlessly incorporate this into practice. I will also go over unique and special circumstances and future implications.

 Read on Twitter
Read on Twitter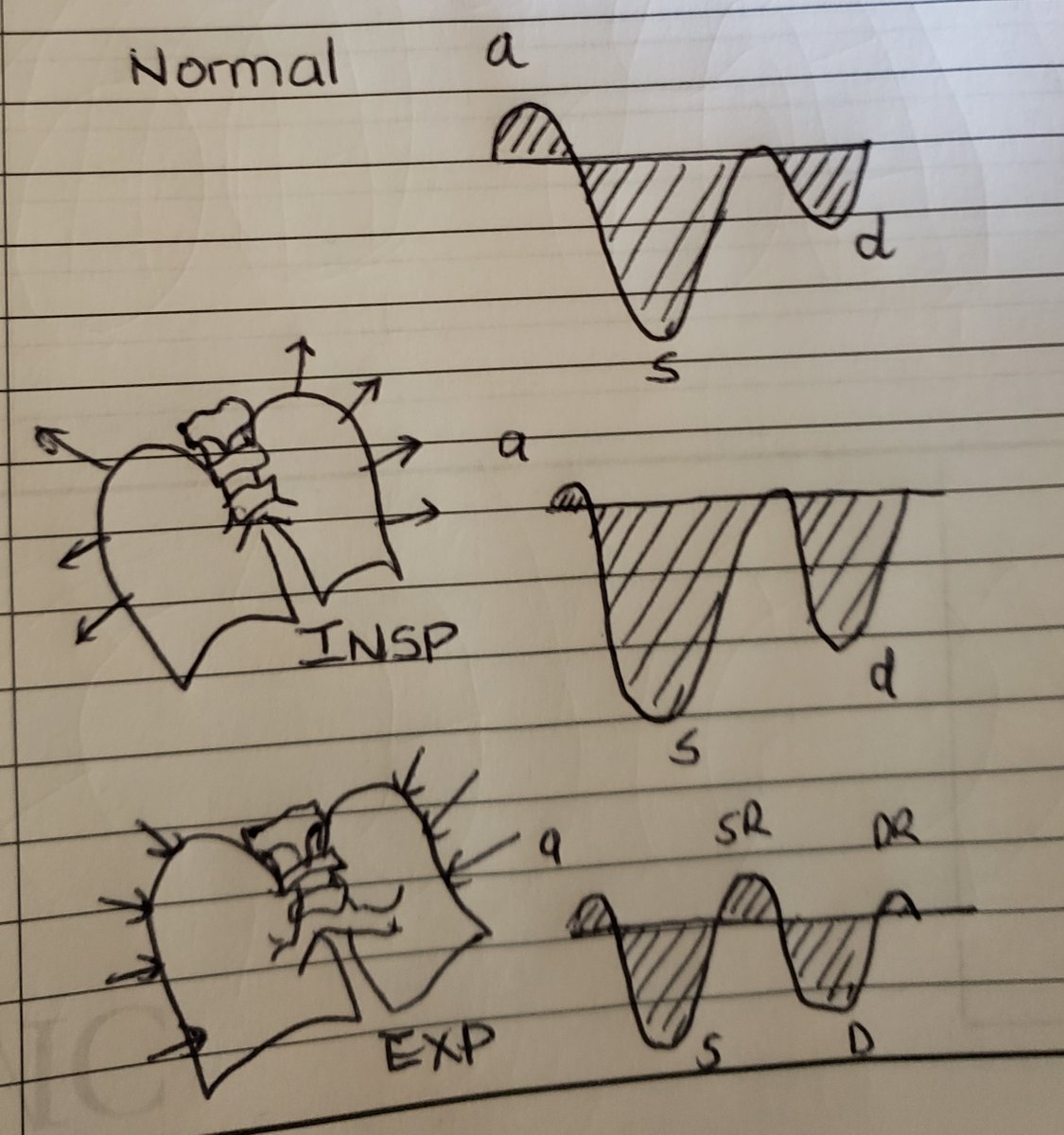 " title="(2/24)We must acquaint ourselves with the different guises that HV waveforms may appear, they can be- biphasic and tetrainflectional- tetraphasic and tetrainflectional - Increased antegrade flow (S and D magnitude)- Increased retrograde flow (A-reversal, SR, DR)Seehttps://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">" class="img-responsive" style="max-width:100%;"/>
" title="(2/24)We must acquaint ourselves with the different guises that HV waveforms may appear, they can be- biphasic and tetrainflectional- tetraphasic and tetrainflectional - Increased antegrade flow (S and D magnitude)- Increased retrograde flow (A-reversal, SR, DR)Seehttps://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">" class="img-responsive" style="max-width:100%;"/>

 - Liver parenchymal disease ( low compliance thus appears as monophasic aninflectional flow)- Aflutter: f-waves, if flutter wave occurs with TV closurehttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">big Ar wave!" title="(6/24)Diminished/absent Ar wave- Afib: no Ar wave, w/o atrial relaxation, S wave magnitude https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten"> - Liver parenchymal disease ( low compliance thus appears as monophasic aninflectional flow)- Aflutter: f-waves, if flutter wave occurs with TV closurehttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">big Ar wave!" class="img-responsive" style="max-width:100%;"/>
- Liver parenchymal disease ( low compliance thus appears as monophasic aninflectional flow)- Aflutter: f-waves, if flutter wave occurs with TV closurehttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">big Ar wave!" title="(6/24)Diminished/absent Ar wave- Afib: no Ar wave, w/o atrial relaxation, S wave magnitude https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten"> - Liver parenchymal disease ( low compliance thus appears as monophasic aninflectional flow)- Aflutter: f-waves, if flutter wave occurs with TV closurehttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">big Ar wave!" class="img-responsive" style="max-width:100%;"/>
 venous returnhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> more reversal waves in pt with https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">RV compliance" title="(8/24)Prominent Ar wave sometimes: - expiration can always increase reversal waves- PVCs and 3rd AV Block w occasional atrial contraction against closed TV- insphttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">venous returnhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> more reversal waves in pt with https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">RV compliance" class="img-responsive" style="max-width:100%;"/>
venous returnhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> more reversal waves in pt with https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">RV compliance" title="(8/24)Prominent Ar wave sometimes: - expiration can always increase reversal waves- PVCs and 3rd AV Block w occasional atrial contraction against closed TV- insphttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">venous returnhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> more reversal waves in pt with https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">RV compliance" class="img-responsive" style="max-width:100%;"/>


 inspiratory diastolic flow reversal!" title="(22/24) In restriction, with inspiration there is increased venous return and given the poor RV compliance https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> inspiratory diastolic flow reversal!" class="img-responsive" style="max-width:100%;"/>
inspiratory diastolic flow reversal!" title="(22/24) In restriction, with inspiration there is increased venous return and given the poor RV compliance https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> inspiratory diastolic flow reversal!" class="img-responsive" style="max-width:100%;"/>


