1/ A Tweetorial on ventilator waveforms and vent dysynchrony. Share any videos of vent dysynchrony if you have them!
@cardionerds @Sam_Brusca @CPSolvers @DxRxEdu @WApplefeld @AnnaPodolanczuk @OslerResidency @sanjayvdesai @ATSCritCare @ColumbiaCCM @iwashyna @DrDaleNeedham
@cardionerds @Sam_Brusca @CPSolvers @DxRxEdu @WApplefeld @AnnaPodolanczuk @OslerResidency @sanjayvdesai @ATSCritCare @ColumbiaCCM @iwashyna @DrDaleNeedham
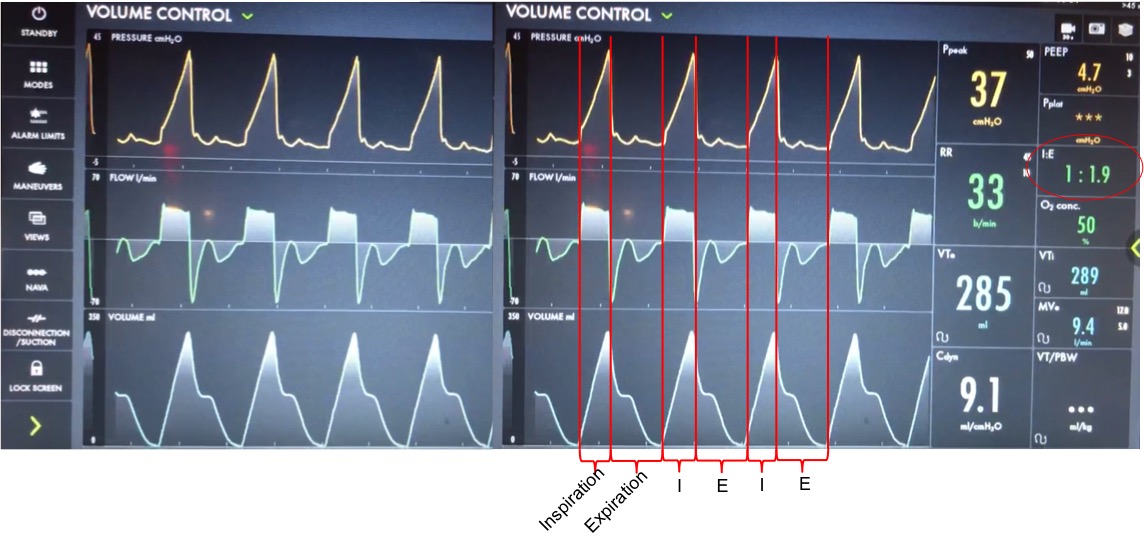
2/ A 40s M is intubated for #Covid-19 ARDS. He has been dysynchronous with the vent so to maintain lung protective ventilation he was on propofol, fentanyl and midazolam. His sedation is being weaned (still RASS -5) and the RN calls for vent dysynchrony. Here is his vent:
3/ Before delving into the type of dysynynchrony and management, based on these waveforms what is actually happening?
4/ Let’s take a look at the waveforms and identify the phase of breathing. This is VC with a square flow waveform, so as the volume is delivered, the flow is at a constant rate, and the pressure is measured. You can see that E is about 2x I (determined by I time or flow rate)
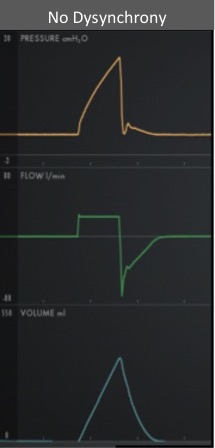
5/ With a passive patient (no dysynchrony) after inspiration, the volume curve should show a smooth decrease with exhalation, the pressure curve should flatten to the set PEEP, and the flow will be negative and gradually return to 0 as the patient exhales
6/ In our case you see simultaneous dysynchrony in all 3 waveforms during exhalation (red arrows). In the pressure waveform there is a negative deflection, the flow quickly rises to 0 before returning to negative, and the volume curve plateaus as exhalation pauses.
7/ Putting this together, it means that during expiration there is an inspiratory effort. The patient is trying to inhale, which causes a negative pressure deflection, and a pause in air flowing out of the lungs. If this effort triggered a breath, there could be breath stacking.
8/ The same pattern occurs after every breath, and the patient was still heavily sedated
This combination of findings is a type of dysynchrony called REVERSE TRIGGERING or ENTRAINMENT
Note: ineffective triggering can be considered, but overall more consistent w/ entrainment
This combination of findings is a type of dysynchrony called REVERSE TRIGGERING or ENTRAINMENT
Note: ineffective triggering can be considered, but overall more consistent w/ entrainment
9/ The change in pressure and flow of a ventilator-initiated breath stimulates an inspiratory effort from the patient. This may be mediated by the diaphragm or the central respiratory center. The stimulated effort can start during inspiration, or after, in exhalation
10/ Reverse triggering often occurs in heavily sedated pts, and is defined by a stable, repetitive pattern (i.e. it is not voluntary, but reflex mediated). It can also occur in anoxic brain injury. It can be induced in awake patients but is seen less clinically in this context.
11 / Treating reverse triggering:
-- Increasing sedation does not work
-- Paralysis is needed if synchrony is mandatory
-- Changing the respiratory rate and tidal volume can break the pattern. Overdistention often plays a role. I like trying a lower RR, and smaller Vts.
-- Increasing sedation does not work
-- Paralysis is needed if synchrony is mandatory
-- Changing the respiratory rate and tidal volume can break the pattern. Overdistention often plays a role. I like trying a lower RR, and smaller Vts.
12/ One last management note.
DO NOT just increase the trigger sensitivity of the vent. This can stop breath stacking, but does not prevent dysynchrony and harmful changes in transpulmonary pressure.
DO NOT just increase the trigger sensitivity of the vent. This can stop breath stacking, but does not prevent dysynchrony and harmful changes in transpulmonary pressure.
13/ For this patient, sedation was lightened further, and the respiratory rate decreased and the pattern of reverse triggering ultimately broke without the need for paralysis.
I hope you enjoyed, and please share any cases of vent dysynchrony that you’ve seen!
I hope you enjoyed, and please share any cases of vent dysynchrony that you’ve seen!

 Read on Twitter
Read on Twitter