#idtips #idmeded day 4. Staph aureus bacteremia. You will deal with this in inpatient medicine / surgical / critical care / emergency specialty.
Want to know the secret why ID consults save lives? Approach
1) Treat appropriately
2) Find the source
3) Find the complications
Want to know the secret why ID consults save lives? Approach
1) Treat appropriately
2) Find the source
3) Find the complications
Why do we care - in the post antibiotic era mortality of 20% (13% infection related) - not changed despite advances in past 15 years. in those over 70 - up to 35%.
Contrast to
3.5% NSTEMI, 4.5% STEMI
2% COVID (depending)
23% AML induction in elderly
THIS IS A SERIOUS DISEASE
Contrast to
3.5% NSTEMI, 4.5% STEMI
2% COVID (depending)
23% AML induction in elderly
THIS IS A SERIOUS DISEASE
ID Consultations save lives. Many different studies - but the approach follows the 3 steps - right treatment, source, complications. No other magic recipe.
Great work by @tonybai16 @ASPphysician
https://academic.oup.com/cid/article/60/10/1451/338895
In">https://academic.oup.com/cid/artic... this study an 8% difference in mortality for consult
Great work by @tonybai16 @ASPphysician
https://academic.oup.com/cid/article/60/10/1451/338895
In">https://academic.oup.com/cid/artic... this study an 8% difference in mortality for consult
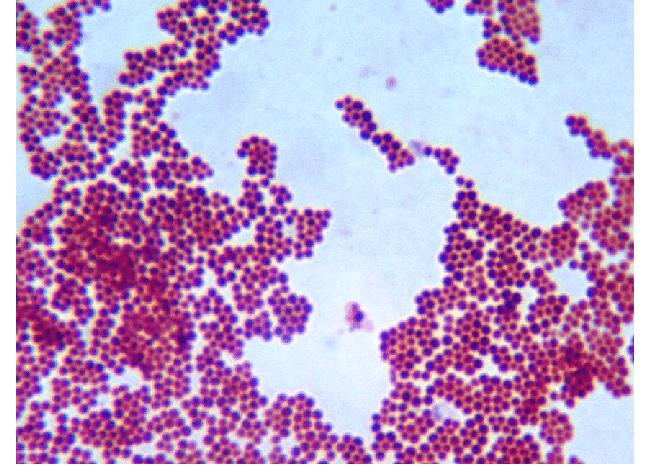
First - blood culture shows GPC in clusters. Evaluate patient first in terms of syndrome - single or multiple cultures, early or late. What was the reason for blood cultures. If stable, not unstable, and unclear if syndrome infectious wait to treat. Repeat cultures.
If suspicion, febrile, unwell then treat.
Use both an MRSA drug and an MSSA drug up front. Ideal is Vanco/Cefazolin for dosing (and cost). Why both?
1) Cover MRSA in the time to get a sensitivity
2) Vanco is a poor MSSA drug - while sick want to optimize with betalactam
Use both an MRSA drug and an MSSA drug up front. Ideal is Vanco/Cefazolin for dosing (and cost). Why both?
1) Cover MRSA in the time to get a sensitivity
2) Vanco is a poor MSSA drug - while sick want to optimize with betalactam
Second - source
Head to toe exam. Examine all lines, mouth, recent IV sites, phlebotomy sites, wounds, injection sites. Look on skin surface for abscesses. Listen to heart for murmur, lungs for consolidation/effusion.
Staph aureus bacteremia is a symptom not a disease
Head to toe exam. Examine all lines, mouth, recent IV sites, phlebotomy sites, wounds, injection sites. Look on skin surface for abscesses. Listen to heart for murmur, lungs for consolidation/effusion.
Staph aureus bacteremia is a symptom not a disease
Third complications
1) Physical exam as above - pay attention to seeding points
-neuro exam for CNS/spinal lesions
-spinal exam top to bottom for disciitis/abscess
-all large and small joints
-liver/spleen exam
-ANYWHERE there is hardware - as these are sticking points
1) Physical exam as above - pay attention to seeding points
-neuro exam for CNS/spinal lesions
-spinal exam top to bottom for disciitis/abscess
-all large and small joints
-liver/spleen exam
-ANYWHERE there is hardware - as these are sticking points
Echo - everyone needs at a minimum - a TTE with reasonable views of valve. Next step - as with everything in medicine, is pre-test probability of how likely. Really this ties to
a) Duration of bacteremia
b) Places where bacteria can stick
c) Multiple sites of infxn
a) Duration of bacteremia
b) Places where bacteria can stick
c) Multiple sites of infxn
Why TEE - in the classic era (1997)
https://pubmed.ncbi.nlm.nih.gov/9316542/
TTE">https://pubmed.ncbi.nlm.nih.gov/9316542/&... was positive in 7 / 26 as compared to TEE. Meaning 19/26 missed.
Imaging resolution diff then and now? even modern studies showing same issue - https://bit.ly/38uP0Dw ">https://bit.ly/38uP0Dw&q...
https://pubmed.ncbi.nlm.nih.gov/9316542/
TTE">https://pubmed.ncbi.nlm.nih.gov/9316542/&... was positive in 7 / 26 as compared to TEE. Meaning 19/26 missed.
Imaging resolution diff then and now? even modern studies showing same issue - https://bit.ly/38uP0Dw ">https://bit.ly/38uP0Dw&q...
So who needs a TTE vs. TEE. Clinical prediction rules help (see: https://bit.ly/2Z0Eelk )
1)">https://bit.ly/2Z0Eelk&q... Duration of bacteremia - community acquired! PWID, long sx duration or long clearance
2) Sticking places - prior IE, pacemakers, valves
3) Multiple sites or multiple embolic events
1)">https://bit.ly/2Z0Eelk&q... Duration of bacteremia - community acquired! PWID, long sx duration or long clearance
2) Sticking places - prior IE, pacemakers, valves
3) Multiple sites or multiple embolic events
If you have a short clearance with a clear source and no risk factors - can argue a totally clean TTE is enough with rapid clearance (i.e. the ICU patient with a line infection that is rapidly dealt with). But think through three steps for each case, and if concerns TEE.
3) Treatment
-make sure all sources that need draining are drained - no treatment will necessarily fix this.
-narrow therapy based on sensitivity
-aim for a minimum of 2 weeks of INTRAVENOUS treatment in patients who are low pretest for IE.
-for all else - aim higher and/or TEE
-make sure all sources that need draining are drained - no treatment will necessarily fix this.
-narrow therapy based on sensitivity
-aim for a minimum of 2 weeks of INTRAVENOUS treatment in patients who are low pretest for IE.
-for all else - aim higher and/or TEE
Oral stepdown - not generally warranted. This is a serious disease and needs to be treated as such. Cohort in Spain of low risk and propensity matching to linezolid which showed reasonable results. Not randomized by any means. But default should be IV https://bit.ly/3dZFlpW ">https://bit.ly/3dZFlpW&q...
Only other big data is POET trial - but remember many were not staph, and zero MRSA in that trial. Regimen was either Linezolid (high dose) + Rifampin or Amoxicillin + Rifampin if PCN susceptible (routinely not done in some centers). +++ Pill burden and close monitoring
Bottom line
1) This is not a disease to mess around with - 1 in 8 of your patients will die, and 1 in 3 if older
2) Treat right early
3) Look for complications and source. TEE in right patients
4) Aim for treatment course as IV. Oral only in certain careful situations.
1) This is not a disease to mess around with - 1 in 8 of your patients will die, and 1 in 3 if older
2) Treat right early
3) Look for complications and source. TEE in right patients
4) Aim for treatment course as IV. Oral only in certain careful situations.

 Read on Twitter
Read on Twitter