Following on from our #Tweetorial looking at silver trauma on this week’s #FractureFriday we’re taking a look at the (grand)mother of all fractures, so important they only take 3 letters to recognise – NOF!!
These patients are so important to manage appropriately as there is a 10% mortality in 30 days and 30% at a year post injury!! The Nottingham hip fracture score helps calculate the individuals risk based on various parameters.
Although these injuries can occur in younger patients as a result of high energy mechanisms the vast majority occur in older patients as a result of low energy injuries.
They may present with inability to weight bear, pain in the hip, pain on “pin-rolling” of the hip, or with a shortened and externally rotated hip. In general have a low threshold to x-ray any older person with difficulty weight-bearing or pain in the hip.
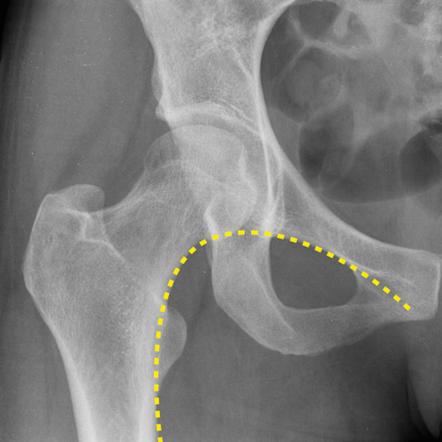
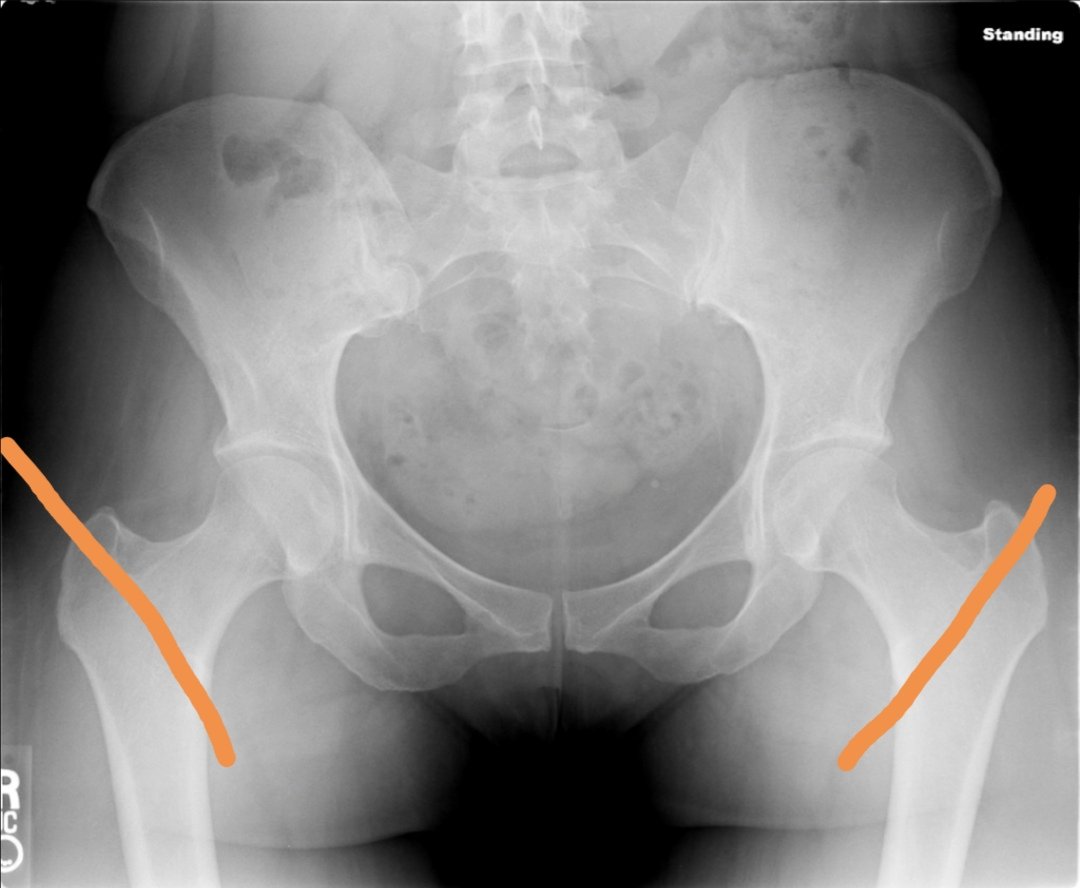
Any fracture of the femur within 5cm of the lesser trochanter is considered a NOF fracture. Some fractures may be obvious but others are not, looking at Shenton’s line can help! This should be a smooth line – if it’s not there may be a fracture!!
Some impacted fractures may not disrupt Shenton’s line but they may show a dense sclerotic line. And don’t forget to look out for other cause of the patients symptoms such as pubic rami or acetabular fracture!
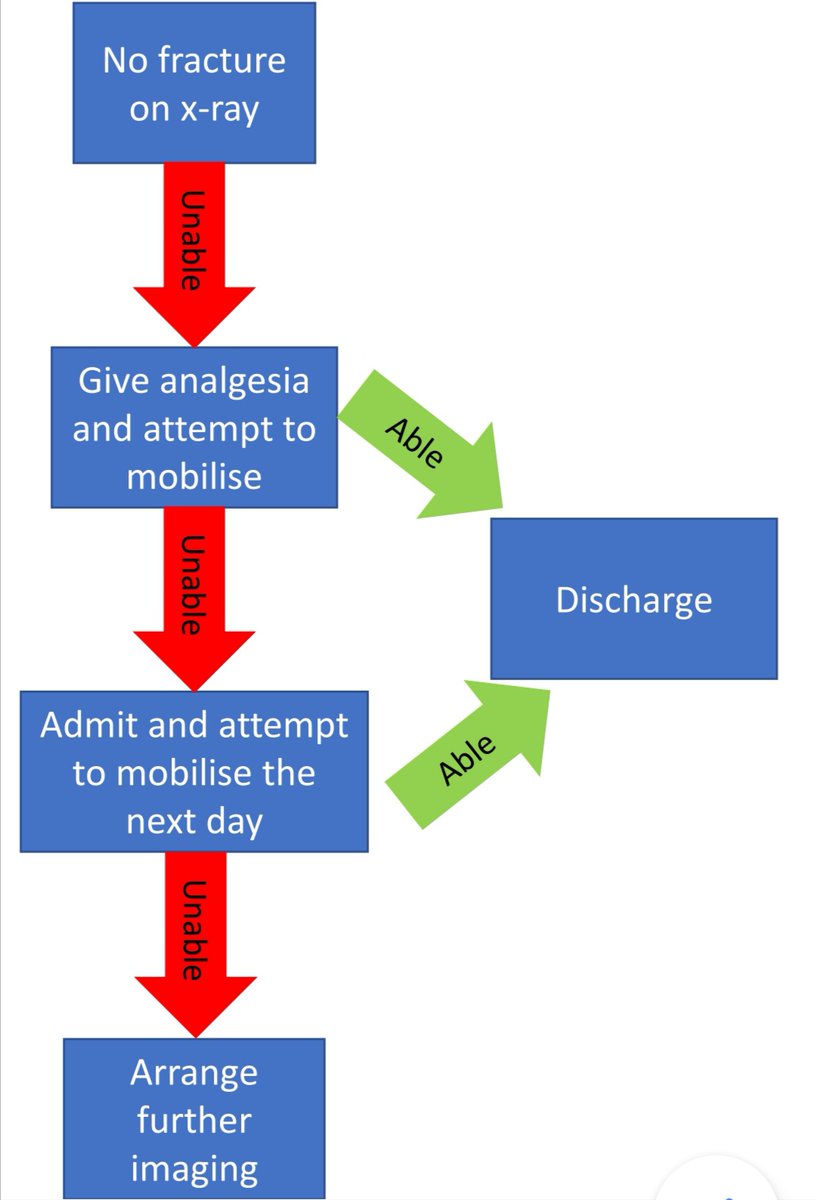
X-ray alone has a sensitivity of 93 – 98% so can miss some fractures. MRI or CT may offer better sensitivity and NICE recommend these if clinical suspicion of fracture still exists. @RCEM offers a pragmatic way to approach this situation.
Looking after patients with NOF fractures is a great example of how excellent MDT work can lead to the best outcome for patients!! Many different teams have an important part to play in the patient’s journey!!
In the ED after making the diagnosis one of the first steps should be ensuring proper analgesia, this may be achieved with either a fascia iliaca or femoral nerve block. Although often done with USS guidance it can be done with landmarks alone!
https://www.rcem.ac.uk/docs/QI%20+%20Clinical%20Audit/FIB%20guideline%20document%20for%20the%20ED.pdf">https://www.rcem.ac.uk/docs/QI%2...
https://www.rcem.ac.uk/docs/QI%20+%20Clinical%20Audit/FIB%20guideline%20document%20for%20the%20ED.pdf">https://www.rcem.ac.uk/docs/QI%2...
Sensible baseline investigations should be arranged, such as bloods, CXR, and ECG. It’s also important to consider why the patient fell. Was it a mechanical fall or was it a caused by another pathology such as a stroke or cardiac problem?
This investigation may be continued by the inpatient geriatric team with a review of the patient’s medications – are they taking sedating medicates? Are they at risk of postural hypotension? They will also optimise the patient for surgery which may include anticoagulant reversal!
The aim is to operate either on the day of injury or the day after – the faster it’s fixed the faster the patient can mobilise!! The choice of how to fix the fracture is made by the orthopaedic team and is based on the type of fracture.
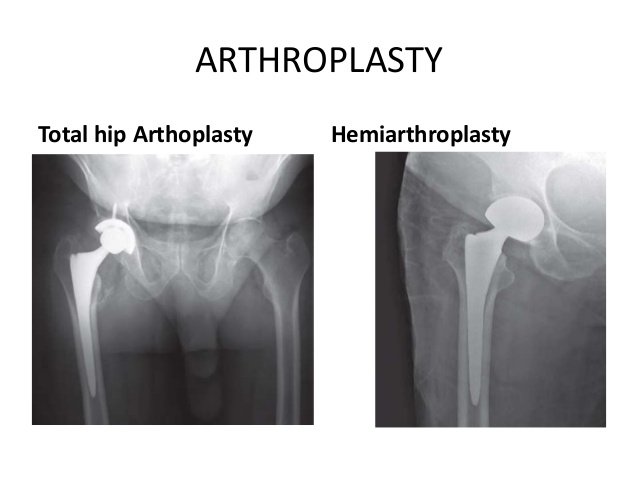
Broadly these can be split into intra and extracapsular fractures, this is relative to the hip joint capsule and can roughly be divided by an imaginary line between the 2 trochanters. This is important as the area proximal to this has a retrograde blood supply.
You may remember from our scaphoid fracture #Tweetorial that this can put the proximal segment at risk of avascular necrosis if there is a displaced intracpsular fracture. They may be managed with a hemiarthroplasty or a total if the patient was very active before injury.
If it is undisplaced then cannulated screws can be used preserving the femoral head. Extracapsular fractures are normally managed with a dynamic hip screw but this requires strong bone to affix to, if this isn’t available then an IM nail with a sliding screw can be used.
The work isn’t over after the surgery though!! Next is a long period of rehabilitation. The physiotherapy team will help the patient mobilise, working on developing muscle strength (with sarcopenia being a cause of falls) and how to mobilise safely.
The occupational therapy team may look at how the patients home circumstances can be adapted to reduce the risk of further falls. Of course the work is not just limited to these groups – as we said it’s a massive team effort!!
A bit of a long one this week but there are lots of things to make sure we think about!! Hope to see you next time for more #FOAMed #MedicalTwitter

 Read on Twitter
Read on Twitter