Going live with the @bartspom #covid19pocus meeting
Join an excellent international faculty discussing all things #pocus and #COVID19!
Join an excellent international faculty discussing all things #pocus and #COVID19!
First up are lung ultrasound royalty -
@LunaGargani and @giovolpicelli
Discussing their extensive experience of lung ultrasound in #COVID19 #covid19pocus
@LunaGargani and @giovolpicelli
Discussing their extensive experience of lung ultrasound in #COVID19 #covid19pocus
Reviewing the initial data on lung ultrasound in #covid19
https://www.escardio.org/Education/E-Learning/Webinars/COVID-19-how-to-use-and-interpret-lung-ultrasound
https://www.escardio.org/Education... href=" https://theultrasoundjournal.springeropen.com/articles/10.1186/s13089-020-00171-w
https://theultrasoundjournal.springeropen.com/articles/... href="https://twtext.com//hashtag/covid19pocus"> #covid19pocus
https://www.escardio.org/Education/E-Learning/Webinars/COVID-19-how-to-use-and-interpret-lung-ultrasound
Latest paper from Luna and Gio here https://link.springer.com/article/10.1007/s00134-020-06048-9
And">https://link.springer.com/article/1... a lovely review from @cianmcdermott and @EMManchester here https://www.medrxiv.org/content/10.1101/2020.06.15.20130344v1">https://www.medrxiv.org/content/1...
And">https://link.springer.com/article/1... a lovely review from @cianmcdermott and @EMManchester here https://www.medrxiv.org/content/10.1101/2020.06.15.20130344v1">https://www.medrxiv.org/content/1...
Little reminder on technique for lung ultrasound
I love this video from @kyliebaker888
https://www.youtube.com/watch?v=Yvc83U74Z3s
https://www.youtube.com/watch... href="https://twtext.com//hashtag/covid19pocus"> #covid19pocus
I love this video from @kyliebaker888
https://www.youtube.com/watch?v=Yvc83U74Z3s
Check out the excellent resource https://www.openlus.com/en/
Which">https://www.openlus.com/en/"... contains tutorials, videos and literature- direct from Gio and Luna
#covid19pocus
Which">https://www.openlus.com/en/"... contains tutorials, videos and literature- direct from Gio and Luna
#covid19pocus
Now @giovolpicelli discussing his experience
in ED, their LUS use was mainly for triage
LUS is very sensitive (more so than CXR and CT in some studies) but not specific https://www.stemlynsblog.org/combatting-covid19-is-lung-ultrasound-an-option/
However">https://www.stemlynsblog.org/combattin... it is “typical”- which means if PTP is high it’s suggestive.
#covid19pocus
in ED, their LUS use was mainly for triage
LUS is very sensitive (more so than CXR and CT in some studies) but not specific https://www.stemlynsblog.org/combatting-covid19-is-lung-ultrasound-an-option/
However">https://www.stemlynsblog.org/combattin... it is “typical”- which means if PTP is high it’s suggestive.
#covid19pocus
The proper terminology for ultrasound (and arguably all imaging) is to speak in terms of probabilities, and not in terms of diagnosis
Gio is giving us a Bayesian lesson here
(Discuss twitter!)
Gio is giving us a Bayesian lesson here
(Discuss twitter!)
Probabilities of #COVID19 based on imaging findings
From https://link.springer.com/content/pdf/10.1007/s00134-020-06048-9.pdf
https://link.springer.com/content/p... href="https://twtext.com//hashtag/covid19pocus"> #covid19pocus
From https://link.springer.com/content/pdf/10.1007/s00134-020-06048-9.pdf
@giovolpicelli takes this one step further
Combining the imaging with the patient’s presenting “phenotype” as seen below #covid19pocus
This is called “clinical integration” and I think it’s something we sometimes forget to do. It can also be quite hard.
Combining the imaging with the patient’s presenting “phenotype” as seen below #covid19pocus
This is called “clinical integration” and I think it’s something we sometimes forget to do. It can also be quite hard.
A key point here, which you might here repeated later today...
Lung ultrasound does not predict outcomes in #covid19 patients.
#covid19pocus
Lung ultrasound does not predict outcomes in #covid19 patients.
#covid19pocus
Interesting question on subpleural consolidations on lung ultrasound- seeing that they may be small infarcts https://link.springer.com/article/10.1007/s00134-020-06085-4
More">https://link.springer.com/article/1... data is needed… #covid19pocus
More">https://link.springer.com/article/1... data is needed… #covid19pocus
Does lung ultrasound still have a role now the pandemic is slowing?
@giovolpicelli reckons it has a role both in the pandemic and in the quiet phase to improve diagnostic accuracy
#covid19pocus
@giovolpicelli reckons it has a role both in the pandemic and in the quiet phase to improve diagnostic accuracy
#covid19pocus
Further discussion on semiotics
We should stop using the term “subpleural consolidation” as all consolidations are subpleural
Gio prefers “peripheral consolidations"
We should stop using the term “subpleural consolidation” as all consolidations are subpleural
Gio prefers “peripheral consolidations"
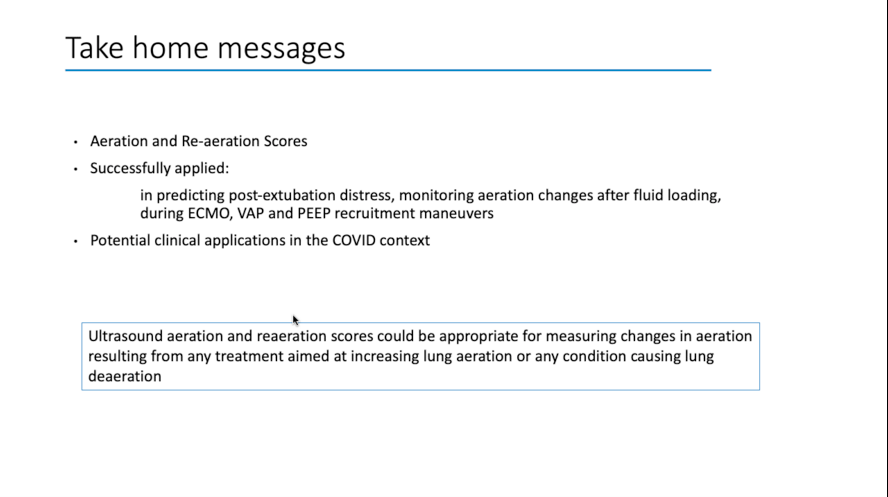
Now Annia Schreiber from Toronto is discussing lung ultrasound scoring in intensive care
Useful papers:
Bouhemad https://anesthesiology.pubs.asahq.org/article.aspx?articleid=2091559
Soldati">https://anesthesiology.pubs.asahq.org/article.a... (COVID19 specific) https://onlinelibrary.wiley.com/doi/full/10.1002/jum.15285
https://onlinelibrary.wiley.com/doi/full/... href="https://twtext.com//hashtag/covid19pocus"> #covid19pocus
Useful papers:
Bouhemad https://anesthesiology.pubs.asahq.org/article.aspx?articleid=2091559
Soldati">https://anesthesiology.pubs.asahq.org/article.a... (COVID19 specific) https://onlinelibrary.wiley.com/doi/full/10.1002/jum.15285
There’s also a lung ultrasound reaeration score https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4069489/">https://www.ncbi.nlm.nih.gov/pmc/artic...
Evidence for lung ultrasound scoring:
Septic shock https://bmcpulmmed.biomedcentral.com/articles/10.1186/s12890-018-0755-9
ECMO:
https://bmcpulmmed.biomedcentral.com/articles/... href=" https://pubmed.ncbi.nlm.nih.gov/28936711/
Recruitment:
https://pubmed.ncbi.nlm.nih.gov/28936711/... href=" https://pubmed.ncbi.nlm.nih.gov/20851923/
(More">https://pubmed.ncbi.nlm.nih.gov/20851923/... on ECMO later) #covid19pocus
Septic shock https://bmcpulmmed.biomedcentral.com/articles/10.1186/s12890-018-0755-9
ECMO:
Recruitment:
(More">https://pubmed.ncbi.nlm.nih.gov/20851923/... on ECMO later) #covid19pocus
How can we integrate this into our ICU patients?
Useful study from @cardiacACCP et al here https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7228719/
https://www.ncbi.nlm.nih.gov/pmc/artic... href="https://twtext.com//hashtag/covid19pocus"> #covid19pocus
Useful study from @cardiacACCP et al here https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7228719/
Annia is suggesting LUS has a role in:
1. Initial diagnosis
2. Selection of therapies
3. EVLW
4. Proning/ECMO
5. Weaning
These are empirical suggestions based on experience, with no data to support this
#covid19pocus
1. Initial diagnosis
2. Selection of therapies
3. EVLW
4. Proning/ECMO
5. Weaning
These are empirical suggestions based on experience, with no data to support this
#covid19pocus
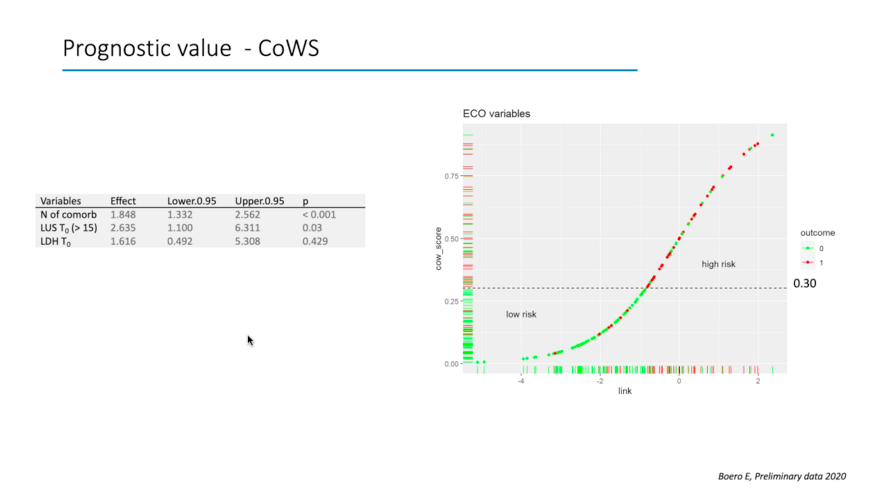
A proposed Lung ultrasound score at presentation to the ED- the CLUE score https://onlinelibrary.wiley.com/doi/10.1111/1742-6723.13546
https://onlinelibrary.wiley.com/doi/10.11... href="https://twtext.com//hashtag/covid19pocus"> #covid19pocus
Using a previous score https://pubmed.ncbi.nlm.nih.gov/32396163/
And">https://pubmed.ncbi.nlm.nih.gov/32396163/... modifying it by adding lung ultrasound, AUROC improved from 0.73 to 0.78
So lung ultrasound by itself does not predict, but it may be another useful data point
And">https://pubmed.ncbi.nlm.nih.gov/32396163/... modifying it by adding lung ultrasound, AUROC improved from 0.73 to 0.78
So lung ultrasound by itself does not predict, but it may be another useful data point
Next up- Enrico Boero on diaphragm monitoring in #COVID19 using ultrasound
Ping @sonophysio
#covid19pocus
Ping @sonophysio
#covid19pocus
Diaphgramatic dysfunction is twice as common as limb weakness following ICU admission
https://www.atsjournals.org/doi/full/10.1164/rccm.201602-0367OC
https://www.atsjournals.org/doi/full/... href="https://twtext.com//hashtag/covid19pocus"> #covid19pocus
https://www.atsjournals.org/doi/full/10.1164/rccm.201602-0367OC
Causes of Ventilator induced diaphragmatic dysfunction (VIDD)
https://link.springer.com/article/10.1186/s40635-019-0259-9
https://link.springer.com/article/1... href="https://twtext.com//hashtag/covid19pocus"> #covid19pocus
(I do wonder about using ultrasound to assess P-SILI…?)
https://link.springer.com/article/10.1186/s40635-019-0259-9
(I do wonder about using ultrasound to assess P-SILI…?)
Diaphgragm ultrasound - uses and how to
https://link.springer.com/article/10.1007/s00134-013-2823-1?utm_content=buffercbc97&utm_medium=social&utm_source=twitter.com&utm_campaign=buffer
https://link.springer.com/article/1... href=" https://pubmed.ncbi.nlm.nih.gov/31938825/
https://pubmed.ncbi.nlm.nih.gov/31938825/... href="https://twtext.com//hashtag/covid19pocus"> #covid19pocus
https://link.springer.com/article/10.1007/s00134-013-2823-1?utm_content=buffercbc97&utm_medium=social&utm_source=twitter.com&utm_campaign=buffer
https://link.springer.com/article/10.1007/s00134-013-2823-1?utm_content=buffercbc97&utm_medium=social&utm_source=twitter.com&utm_campaign=buffer
Does it predict weaning outcomes?
Maybe https://journal.chestnet.org/article/S0012-3692(17)31482-4/pdf
Maybe">https://journal.chestnet.org/article/S... not:
https://pubmed.ncbi.nlm.nih.gov/30910636/
https://pubmed.ncbi.nlm.nih.gov/30910636/... href="https://twtext.com//hashtag/covid19pocus"> #covid19pocus
Maybe https://journal.chestnet.org/article/S0012-3692(17)31482-4/pdf
Maybe">https://journal.chestnet.org/article/S... not:
https://pubmed.ncbi.nlm.nih.gov/30910636/
Beautiful work from my friend @aron_jonny
Describing the role of advanced echocardiography in managing the #COVID19 patient
Including a huge focus on the right ventricle ping @concernecus
Describing the role of advanced echocardiography in managing the #COVID19 patient
Including a huge focus on the right ventricle ping @concernecus

 Read on Twitter
Read on Twitter

 #covid19pocus" title="Probabilities of #COVID19 based on imaging findingsFrom https://link.springer.com/content/p... href="https://twtext.com//hashtag/covid19pocus"> #covid19pocus" class="img-responsive" style="max-width:100%;"/>
#covid19pocus" title="Probabilities of #COVID19 based on imaging findingsFrom https://link.springer.com/content/p... href="https://twtext.com//hashtag/covid19pocus"> #covid19pocus" class="img-responsive" style="max-width:100%;"/>

 #covid19pocus(I do wonder about using ultrasound to assess P-SILI…?)" title="Causes of Ventilator induced diaphragmatic dysfunction (VIDD) https://link.springer.com/article/1... href="https://twtext.com//hashtag/covid19pocus"> #covid19pocus(I do wonder about using ultrasound to assess P-SILI…?)" class="img-responsive" style="max-width:100%;"/>
#covid19pocus(I do wonder about using ultrasound to assess P-SILI…?)" title="Causes of Ventilator induced diaphragmatic dysfunction (VIDD) https://link.springer.com/article/1... href="https://twtext.com//hashtag/covid19pocus"> #covid19pocus(I do wonder about using ultrasound to assess P-SILI…?)" class="img-responsive" style="max-width:100%;"/>


