Performance status in cancer isn’t broken, but is it time for an upgrade? Check out our commentary with @ElisabethEdvar2 Guro Stene and Lee Jones in @ASCO_pubs on different tools to assess PS https://ascopubs.org/doi/full/10.1200/JCO.20.00721#.XvUWQFppeI8.twitter">https://ascopubs.org/doi/full/... THREAD
1948: Karnofsky et al used 3 criteria to evaluate nitrogen mustard efficacy: objective (decrease in lesion size), subjective (patient reported symptoms), and PS (i.e., patients’ ability to participate in activities of daily life) /2
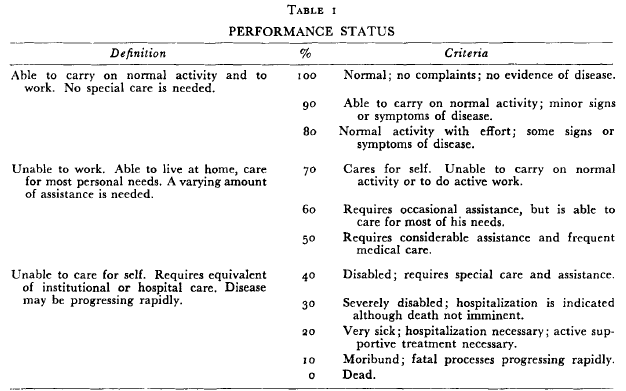
Evaluation of PS was standardized using a physician rated scale, now known as Karnofsky Performance Status (KPS), ranging from 0 (dead) to 100 (well-functioning) with 10-point increments /3
1960: Zubrod et al. introduced simpler 6-point Eastern Cooperative Oncology Group (ECOG) PS scale [0 (fully active) to 5 (dead)] as one of 15 standardized assessments for all ECOG multicenter clinical trials /4
1973: ECOG and KPS were used to evaluate therapeutic efficacy, until, in what appears to be a fantastic keynote, Zelen stated that PS should and must be considered in clinical trial eligibility /5
1973-80s: PS scales in clinical trials transitioned from assessment of therapeutic efficacy to eligibility and stratification (i.e., more homogenous subgroups) /6
1980s-present: KPS and ECOG scores are strong independent predictors of clinical outcomes, are inexpensive, and used in virtually every clinical across the entire cancer care continuum. So why advocate for an upgrade? /7
KPS and ECOG have poor reliability, limited prognostic value in patients with good PS, restricted ability to detect longitudinal ‘real-time’ changes. More objective, discriminatory, and dynamic tools are needed! /8
Great alternative tools are available like HCT-CI or #geriatric assessment However, these tools are population specific https://jamanetwork.com/journals/jamaoncology/fullarticle/2754746">https://jamanetwork.com/journals/... /9
In non-oncology settings, numerous standardized tests are used like sit-to-stand test, timed up and go test, 6 min walk test. But, these tools have ‘low ceilings’, so may not help discriminate between pts with good PS /10
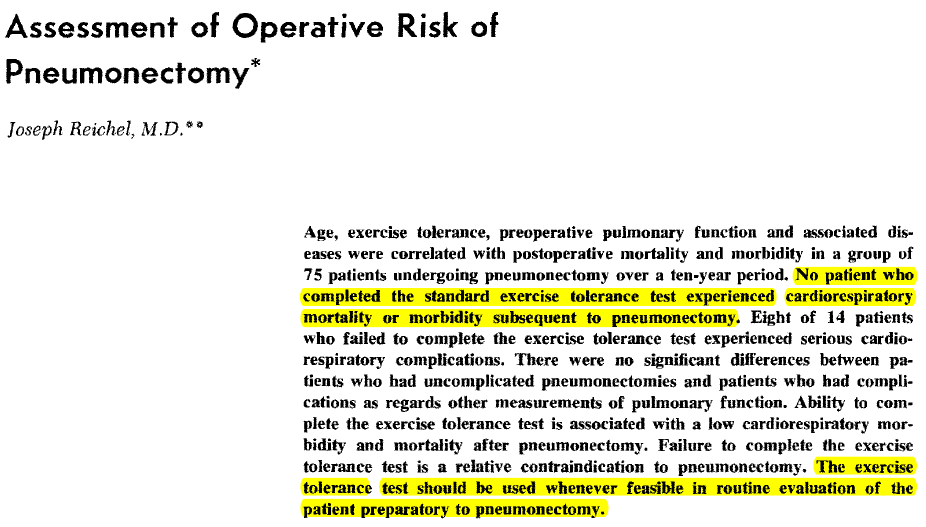
#exercise tests (e.g., CPET) are the gold standard for many reasons and VO2peak is considered a ‘clinical vital sign’ in chronic cardiac and lung conditions, could they be used in oncology? Back in 1972 Reichel thought so /11
Despite major advantages, CPET requires specialized equipment and trained personnel – widespread clinical application may be limited /12
What’s next? Perhaps a #digital phenotyping frontier. Many challenges for implementation, but integration of physiological, mobility, PRO, EHR data may be help treatment selection, clinical trial eligibility, and toxicity monitoring /end

 Read on Twitter
Read on Twitter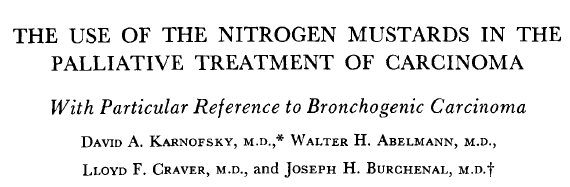
![1960: Zubrod et al. introduced simpler 6-point Eastern Cooperative Oncology Group (ECOG) PS scale [0 (fully active) to 5 (dead)] as one of 15 standardized assessments for all ECOG multicenter clinical trials /4 1960: Zubrod et al. introduced simpler 6-point Eastern Cooperative Oncology Group (ECOG) PS scale [0 (fully active) to 5 (dead)] as one of 15 standardized assessments for all ECOG multicenter clinical trials /4](https://pbs.twimg.com/media/EbY2iRfWsAk52OE.png)