So the #RECOVERYtrial RECOVERY dexamethasone study has been released as a preprint, although one should be careful of pre-prints, the team delivering this & the nature of the (non-commercial) study gives this strong preliminary validity. @PeterHorby https://www.medrxiv.org/content/10.1101/2020.06.22.20137273v1">https://www.medrxiv.org/content/1...
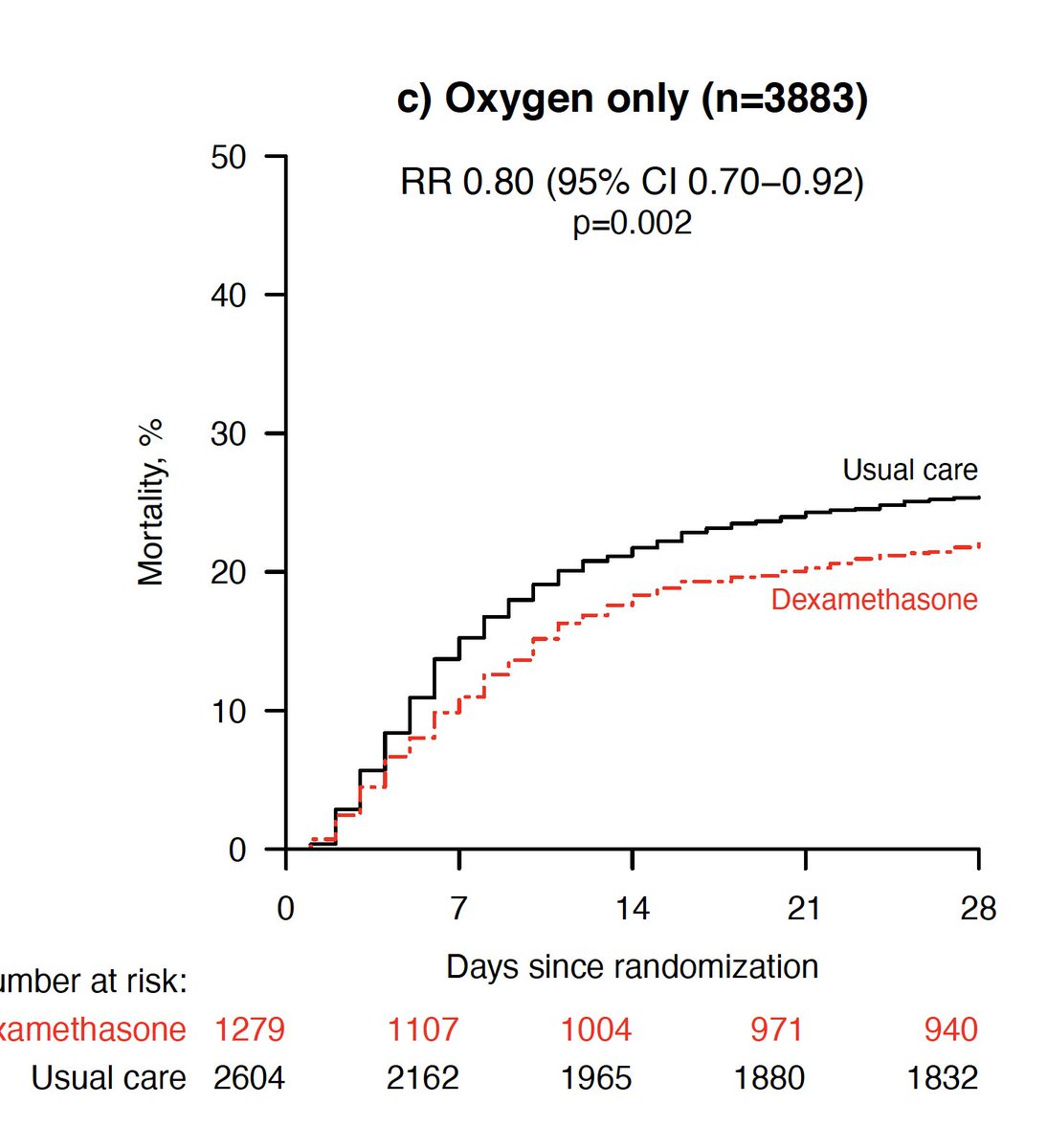
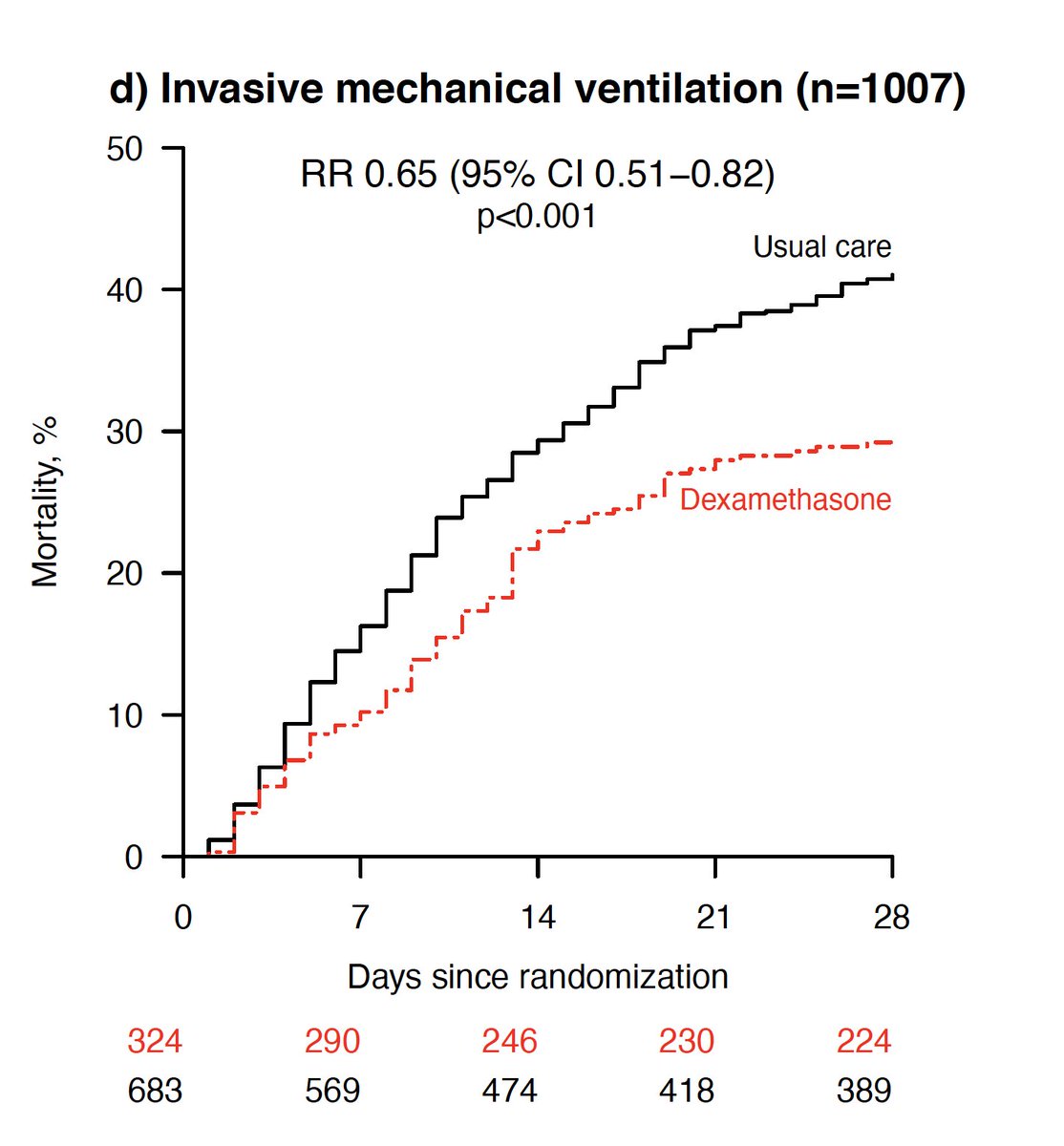
We’ve seen the headline result, dexamethasone reduces mortality in ventilated patients by 12% (relative risk reduction 30%) and 5% (relative risk reduction 20%) in patients needing oxygen.
A massive treatment effect, totally unbelievable? Whilst critical care is used to seeing relatively small treatment effects in-fact this is in keeping with the 15% ARR seen in heterogenous ARDS in Villar et al’s recent trial of steroids in ARDS https://pubmed.ncbi.nlm.nih.gov/32043986/ ">https://pubmed.ncbi.nlm.nih.gov/32043986/...
Indeed
PROSEVA, a trial of proning in ARDS, demonstrated a 16.8% ARR
https://pubmed.ncbi.nlm.nih.gov/23688302/
Low">https://pubmed.ncbi.nlm.nih.gov/23688302/... tidal volumes -the most robustly reproduced effect in ARDS – had an 8.8% ARR
https://pubmed.ncbi.nlm.nih.gov/10793162/ ">https://pubmed.ncbi.nlm.nih.gov/10793162/...
PROSEVA, a trial of proning in ARDS, demonstrated a 16.8% ARR
https://pubmed.ncbi.nlm.nih.gov/23688302/
Low">https://pubmed.ncbi.nlm.nih.gov/23688302/... tidal volumes -the most robustly reproduced effect in ARDS – had an 8.8% ARR
https://pubmed.ncbi.nlm.nih.gov/10793162/ ">https://pubmed.ncbi.nlm.nih.gov/10793162/...
And, this is one of the largest studies ever conducted in ARDS – (and yes, almost all the ventilated C19 patients meet criteria for ARDS and would have been eligible for almost every ARDS trial over the past two decades, so lets not start that one again).
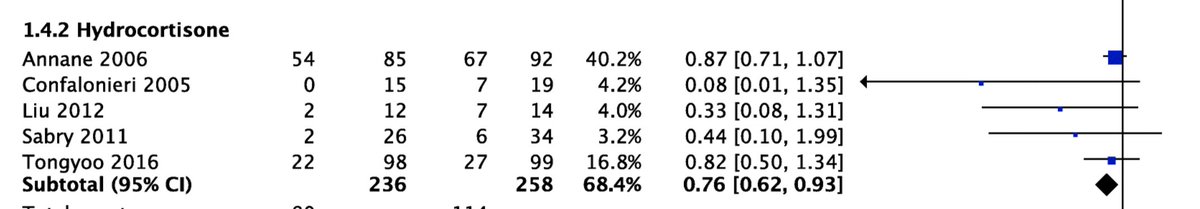
So the effect size is not implausible. What about mechanism? Steroids in ARDS have a mixed picture, variations in dose, timing and patient selection probably affect this.
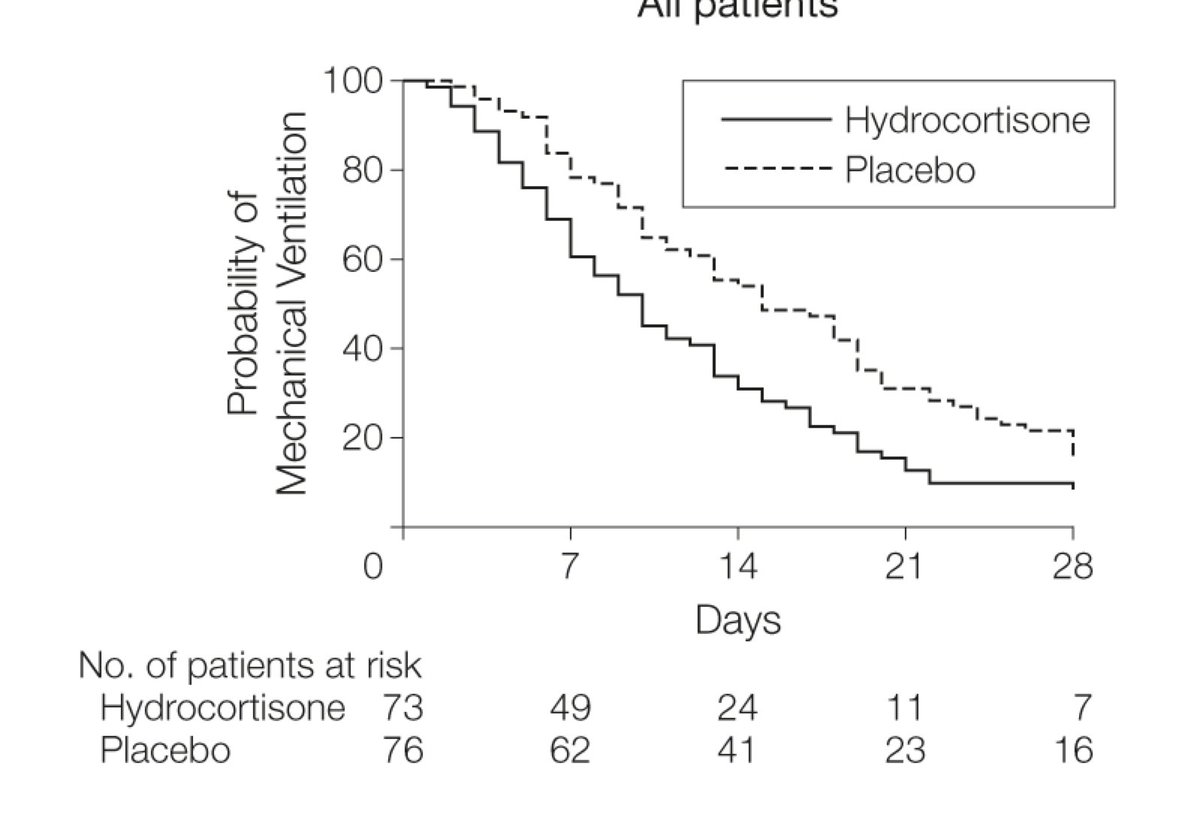
Meduri and colleagues suggested steroids reduced duration of ventilation https://pubmed.ncbi.nlm.nih.gov/17426195/ ">https://pubmed.ncbi.nlm.nih.gov/17426195/...
Meduri and colleagues suggested steroids reduced duration of ventilation https://pubmed.ncbi.nlm.nih.gov/17426195/ ">https://pubmed.ncbi.nlm.nih.gov/17426195/...
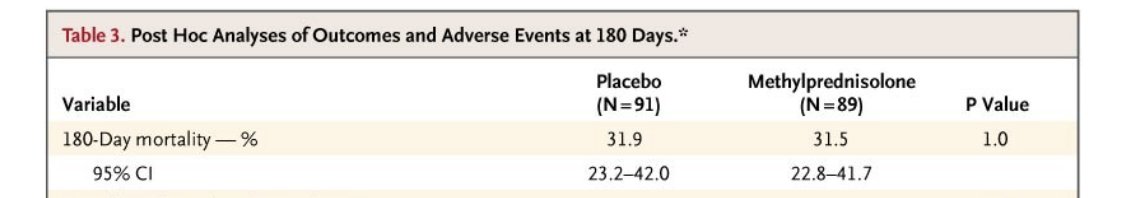
whilst the ARDSnet trialists suggested that short-term outcomes might be better but longer term complications might be higher, leading to no overall benefit (so we do need to see long-term outcomes in RECOVERY)
https://pubmed.ncbi.nlm.nih.gov/16625008/ ">https://pubmed.ncbi.nlm.nih.gov/16625008/...
https://pubmed.ncbi.nlm.nih.gov/16625008/ ">https://pubmed.ncbi.nlm.nih.gov/16625008/...
However, a recent meta analysis suggested that steroids did improve mortality and shorten ventilation in patients with ARDS
https://pubmed.ncbi.nlm.nih.gov/30155260/ ">https://pubmed.ncbi.nlm.nih.gov/30155260/...
https://pubmed.ncbi.nlm.nih.gov/30155260/ ">https://pubmed.ncbi.nlm.nih.gov/30155260/...
Surely giving immunosuppressive steroids to patients with an infection is a bad idea? (And remember most ARDS is actually severe pneumonia, usually bacterial but also viral)
This is where it gets interesting. In RECOVERY, benefit in patients was in those with >7 days of symptoms -and not in those who did not need oxygen (who may be earlier in disease, when viral replication is prominent)- in the unadjusted analysis mortality was HIGHER in this group
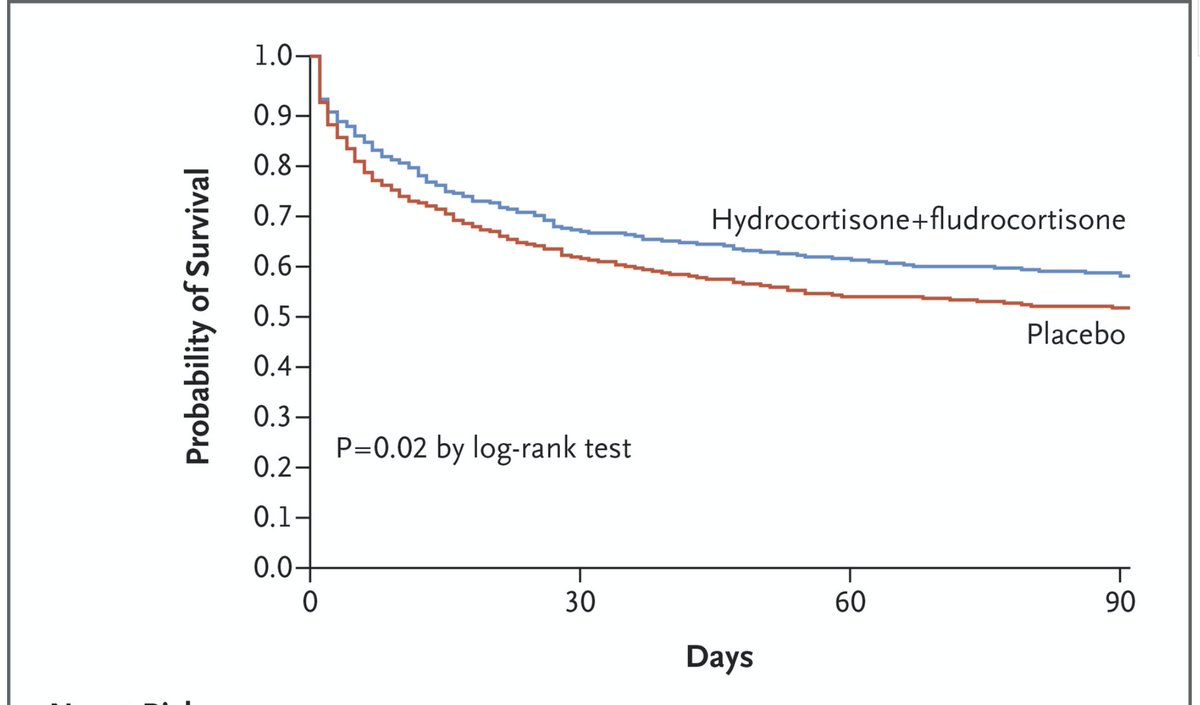
But steroids are probably beneficial, or at least not harmful, in patients with severe infections leading to septic shock -this was mostly thought to be due to effects on vasoplegia but may in-fact be immunomodulatory.
https://pubmed.ncbi.nlm.nih.gov/29490185/ ">https://pubmed.ncbi.nlm.nih.gov/29490185/...
https://pubmed.ncbi.nlm.nih.gov/29490185/ ">https://pubmed.ncbi.nlm.nih.gov/29490185/...
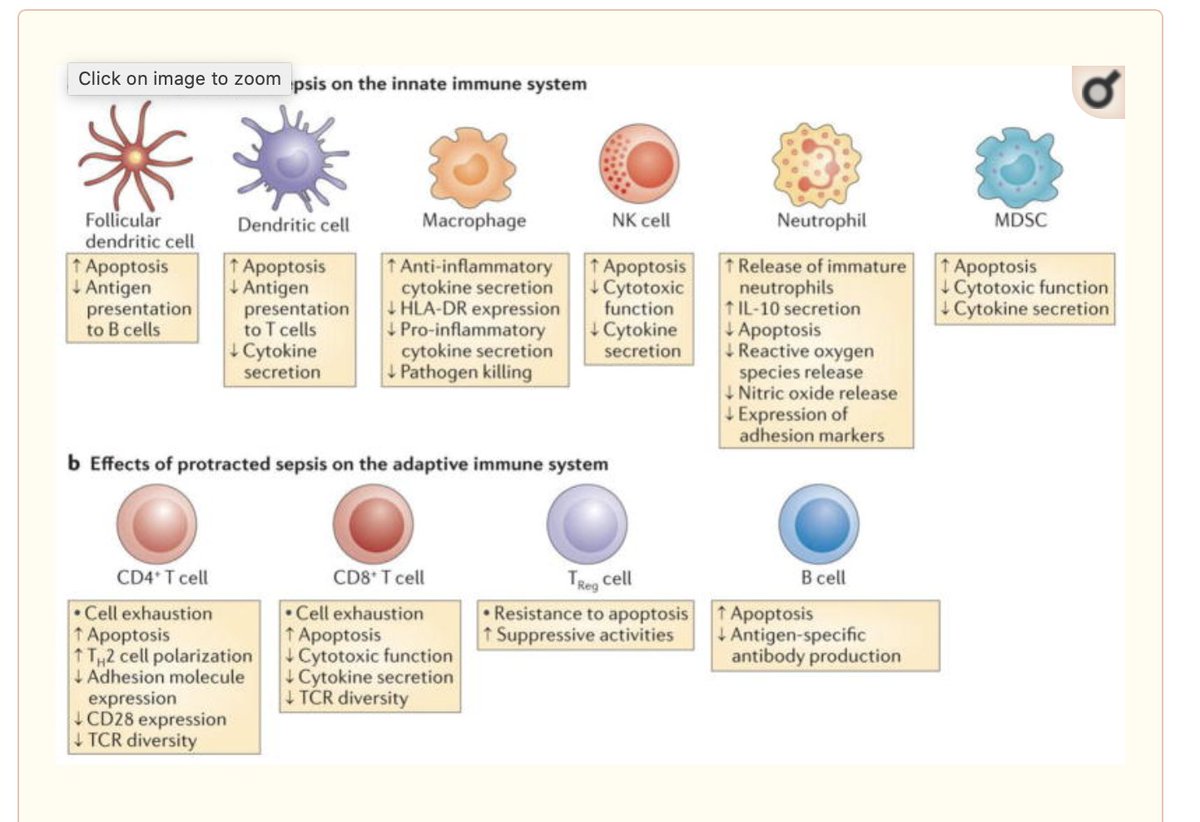
For someone who has spent the last 13 odd years researching the immunoparetic effects of critical illness, and showing the impact of this on secondary infections, this is a little hard to square with my work and that of others in the field -review linked
https://pubmed.ncbi.nlm.nih.gov/24232462/ ">https://pubmed.ncbi.nlm.nih.gov/24232462/...
https://pubmed.ncbi.nlm.nih.gov/24232462/ ">https://pubmed.ncbi.nlm.nih.gov/24232462/...
However, several studies suggest that steroids may REDUCE the risk of secondary infection in ARDS. Weird, huh https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤔" title="Denkendes Gesicht" aria-label="Emoji: Denkendes Gesicht">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤔" title="Denkendes Gesicht" aria-label="Emoji: Denkendes Gesicht">
https://pubmed.ncbi.nlm.nih.gov/17426195/ ">https://pubmed.ncbi.nlm.nih.gov/17426195/... https://pubmed.ncbi.nlm.nih.gov/21427372/ ">https://pubmed.ncbi.nlm.nih.gov/21427372/...
https://pubmed.ncbi.nlm.nih.gov/17426195/ ">https://pubmed.ncbi.nlm.nih.gov/17426195/... https://pubmed.ncbi.nlm.nih.gov/21427372/ ">https://pubmed.ncbi.nlm.nih.gov/21427372/...
This may be because steroids help get people off ventilators faster, and being ventilated is the strongest risk factor for developing pneumonia in ICU
https://pubmed.ncbi.nlm.nih.gov/21666444/ ">https://pubmed.ncbi.nlm.nih.gov/21666444/...
https://pubmed.ncbi.nlm.nih.gov/21666444/ ">https://pubmed.ncbi.nlm.nih.gov/21666444/...
But is may also be that steroids help turn off the systemic inflammatory response that drives the secondary immunosuppression
https://pubmed.ncbi.nlm.nih.gov/25289930/
https://pubmed.ncbi.nlm.nih.gov/25289930/... href=" https://pubmed.ncbi.nlm.nih.gov/7067052/ ">https://pubmed.ncbi.nlm.nih.gov/7067052/&... https://link.springer.com/chapter/10.1007/978-3-642-35109-9_11">https://link.springer.com/chapter/1...
https://pubmed.ncbi.nlm.nih.gov/25289930/
There remain a whole pile of unanswered questions, are there subgroups who benefit, should we use steroids for all ARDS, should we use steroids in ventilated bacterial pneumonia, how do they interact with the patients’ endogenous steroid secretion?
But TL:DR, will I be using dexamethasone at 6mg/day for ventilated or severe non-ventilated COVID19?
Yes -indeed have already prescribed it.
Yes -indeed have already prescribed it.
PS -this study is an amazing achievement, during a pandemic -just look at the list of those involved from across the UK. Its a tribute to the NHS and UK medicine& #39;s comittment to evidence-based medicine https://www.medrxiv.org/content/medrxiv/suppl/2020/06/22/2020.06.22.20137273.DC1/2020.06.22.20137273-1.pdf">https://www.medrxiv.org/content/m...

 Read on Twitter
Read on Twitter