It is no news that the Dexa trial is out in preprint.
Great work!
Many have been calling it practice changing and have suggested Dexa should be used in all patients admitted and in need of oxygen or mechanical ventilation.
I am way less comfortable with the interpretation.
Great work!
Many have been calling it practice changing and have suggested Dexa should be used in all patients admitted and in need of oxygen or mechanical ventilation.
I am way less comfortable with the interpretation.
Don´t get me wrong, the work is great. But I have some questions that challenge the criteria to use Dexa.
Short summary:
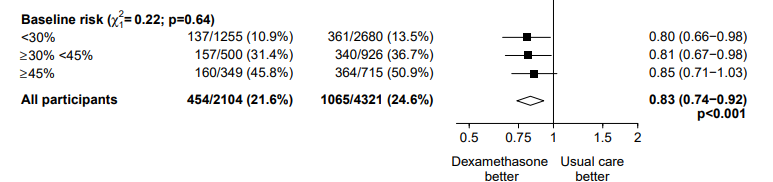
Dexa vs. usual care = 3% absolute risk reduction /14% relative risk reduction.
Subgroup analysis by respiratory support showing effect modification.
Short summary:
Dexa vs. usual care = 3% absolute risk reduction /14% relative risk reduction.
Subgroup analysis by respiratory support showing effect modification.
Those receiving no oxygen had no benefit and potential, yet non-significant harm from treatment (aHR 1.22)
Those on oxygen and those on a vent had benefit (aHR 0.80 and 0.65).
The conclusion suggests anyone on oxygen or on a ventilator would benefit and should be treated w/ Dexa
Those on oxygen and those on a vent had benefit (aHR 0.80 and 0.65).
The conclusion suggests anyone on oxygen or on a ventilator would benefit and should be treated w/ Dexa
Does the need for oxygen / vent interact with the way Dexa acts on the lungs / patient? If there is not rationale, does the stratification make sense? I am not sure it does.
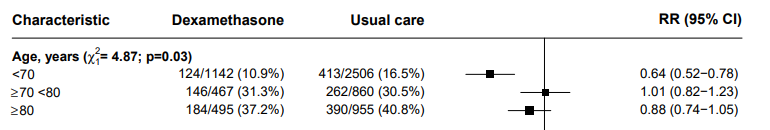
While they are a marker of severity, the study says there is no change in treatment effects based on the "Baseline risk" (figure).
Too bad I did not find the definition of this risk on the study protocol, manuscript or stats plan v1.0 or v.1.1, so I am not sure what this means.
Too bad I did not find the definition of this risk on the study protocol, manuscript or stats plan v1.0 or v.1.1, so I am not sure what this means.
If the difference in benefit between respiratory support group is not a direct effect of the effect modification, could it be related to something else (confounding)?
Although the study is balanced across treatments it is not balanced across subgroups.
Although the study is balanced across treatments it is not balanced across subgroups.
Can another effect modifier lead to the difference?
If yes, can this be the real factor leading to differences in benefit by treatment?
Is there a rationale for this?
I would say yes twice for all of those questions
If yes, can this be the real factor leading to differences in benefit by treatment?
Is there a rationale for this?
I would say yes twice for all of those questions
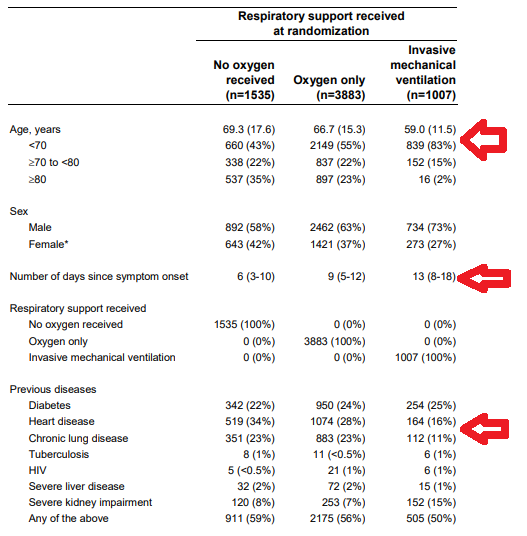
1. The subgroups are imbalanced by a lot of things, some rather unusual.
The more severe group is younger, has less comorbidities (heart and lung, mostly) and had longer disease duration.
Can this be effect modifier for the impact of dexamethasone on the outcomes?
The more severe group is younger, has less comorbidities (heart and lung, mostly) and had longer disease duration.
Can this be effect modifier for the impact of dexamethasone on the outcomes?
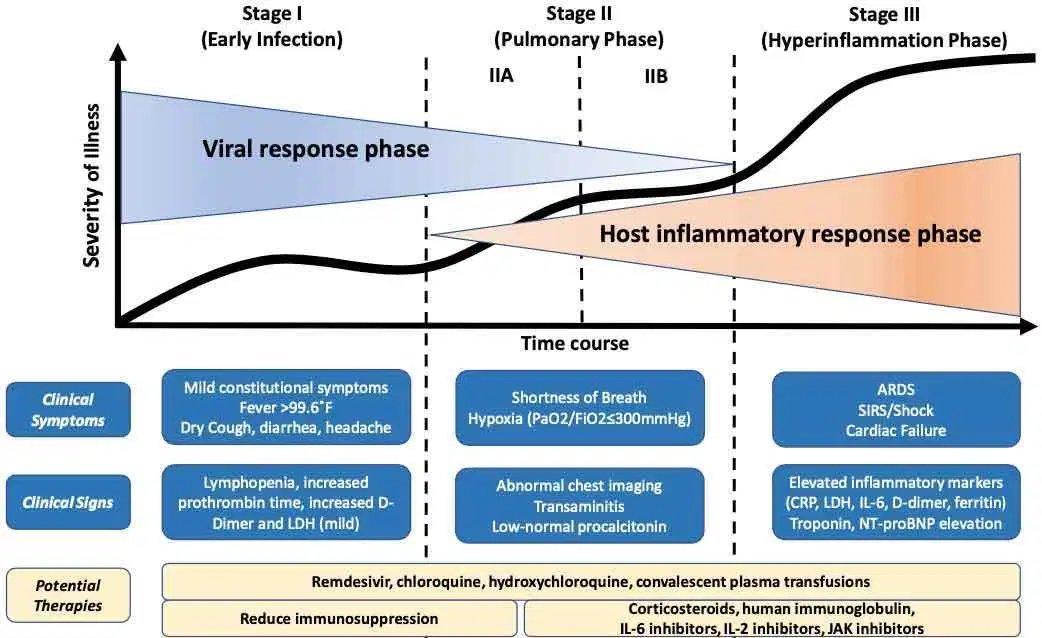
A. Could "days since symptom onset" be the effect modifier?
This classic figure suggest a pathophysiological reason.
The difference in the table 1 is not small (6 vs. 13 days).
This classic figure suggest a pathophysiological reason.
The difference in the table 1 is not small (6 vs. 13 days).
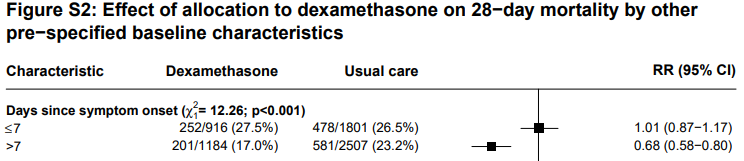
And the effect is clearly documents in table S2.
Difference in magnitude comparable to the ventilatory support stratification, significant (p<0.001) and chi-sq 12.
So yes, The benefit could be related to timing, not support.
Difference in magnitude comparable to the ventilatory support stratification, significant (p<0.001) and chi-sq 12.
So yes, The benefit could be related to timing, not support.
Moreover, giving it early could have negative effects, as the immunosuppression / modulation could facilitate viral replication.
So, interpretation 1: The effect of dexa could likely be dependent on time (better late) rather than ventilatory support.
So, interpretation 1: The effect of dexa could likely be dependent on time (better late) rather than ventilatory support.
Still, there is at least one alternative explanation to consider.
The more severe group is 10y younger (69 vs. 59) and has lower prevalence of heart (16% vs. 34%) and lung disease (11% vs. 34%).
This means the more severe group is less frail. Can this be the effect modifier?
The more severe group is 10y younger (69 vs. 59) and has lower prevalence of heart (16% vs. 34%) and lung disease (11% vs. 34%).
This means the more severe group is less frail. Can this be the effect modifier?
Once again yes. Pathophysiology rationales:
A. more frail, older individuals are less likely to develop immune over response, thus less likely to benefit from immunomodulation.
B. Those individuals also more likely to develop secondary infections, critical care neuropathy, etc.
A. more frail, older individuals are less likely to develop immune over response, thus less likely to benefit from immunomodulation.
B. Those individuals also more likely to develop secondary infections, critical care neuropathy, etc.
From rationale to evidence, table S2 also demonstrates that the benefit is restricted to those <70y.
Unfortunately no data on comorbidities.
So, interpretation 2, risk benefit might only be favorable to dexa in younger or those with less comorbidities.
Unfortunately no data on comorbidities.
So, interpretation 2, risk benefit might only be favorable to dexa in younger or those with less comorbidities.
Although these or not final conclusions, they show that the subgroup analysis is not definite. In fact, I think these two options have even more pathophysiological rationale than what authors propose.
It is important to note that this is not just a picky twitter reviewer comment, this has important practical implication on who are the real candidates for this important treatment.
Again, congratulations to the authors for the great work.
I´ll end with a question based on the study and my comments. Who do you think is probably the key factor to decide when to use Dexa based on RECOVERY?
I´ll end with a question based on the study and my comments. Who do you think is probably the key factor to decide when to use Dexa based on RECOVERY?

 Read on Twitter
Read on Twitter