THREAD!!  https://abs.twimg.com/emoji/v2/... draggable="false" alt="🥳" title="Partying face" aria-label="Emoji: Partying face">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🥳" title="Partying face" aria-label="Emoji: Partying face"> https://abs.twimg.com/emoji/v2/... draggable="false" alt="😁" title="Grinsendes Gesicht mit lächelnden Augen" aria-label="Emoji: Grinsendes Gesicht mit lächelnden Augen">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="😁" title="Grinsendes Gesicht mit lächelnden Augen" aria-label="Emoji: Grinsendes Gesicht mit lächelnden Augen">
Why @josimpson11’s paper on intubation barrier devices (that is, aerosol boxes AND plastic drapes) is, by a good margin, the most important thing that’s been published on these devices.
@Anaes_Journal https://onlinelibrary.wiley.com/doi/abs/10.1111/anae.15188">https://onlinelibrary.wiley.com/doi/abs/1...
Why @josimpson11’s paper on intubation barrier devices (that is, aerosol boxes AND plastic drapes) is, by a good margin, the most important thing that’s been published on these devices.
@Anaes_Journal https://onlinelibrary.wiley.com/doi/abs/10.1111/anae.15188">https://onlinelibrary.wiley.com/doi/abs/1...
Here& #39;s the first thing I LOVE about this paper: an engineer is an author!
Doctors are so frequently happy to step into other fields (law, stats, engineering, etc) without ever asking the experts for their input. Not these guys- they actually got an engineer involved!
Doctors are so frequently happy to step into other fields (law, stats, engineering, etc) without ever asking the experts for their input. Not these guys- they actually got an engineer involved!
They used a quantitative technique to measure the actual aerosol levels (in five different sizes, no less) at the intubator& #39;s head. No exploding fluorescent balloons in this study! They obtained actual aerosol numbers, measured objectively, which were generated with a neb.
They studied five different barriers, not just the box!
1. Conventional aerosol box (with suction),
2. Vertical plastic sheet,
3. Horizontal plastic sheet, and
4/5. A sealed box with an HME filter with, and without section.
All were compared to a control with no barrier device.
1. Conventional aerosol box (with suction),
2. Vertical plastic sheet,
3. Horizontal plastic sheet, and
4/5. A sealed box with an HME filter with, and without section.
All were compared to a control with no barrier device.
7 intubations per device; 42 intubations.
Aerosols were generated with a nebuliser and dispersed by the "patient" coughing. A nebuliser would generate large droplets as well, but unlike some experiments, in this study the quantitative analyser selectively detected only aerosols.
Aerosols were generated with a nebuliser and dispersed by the "patient" coughing. A nebuliser would generate large droplets as well, but unlike some experiments, in this study the quantitative analyser selectively detected only aerosols.
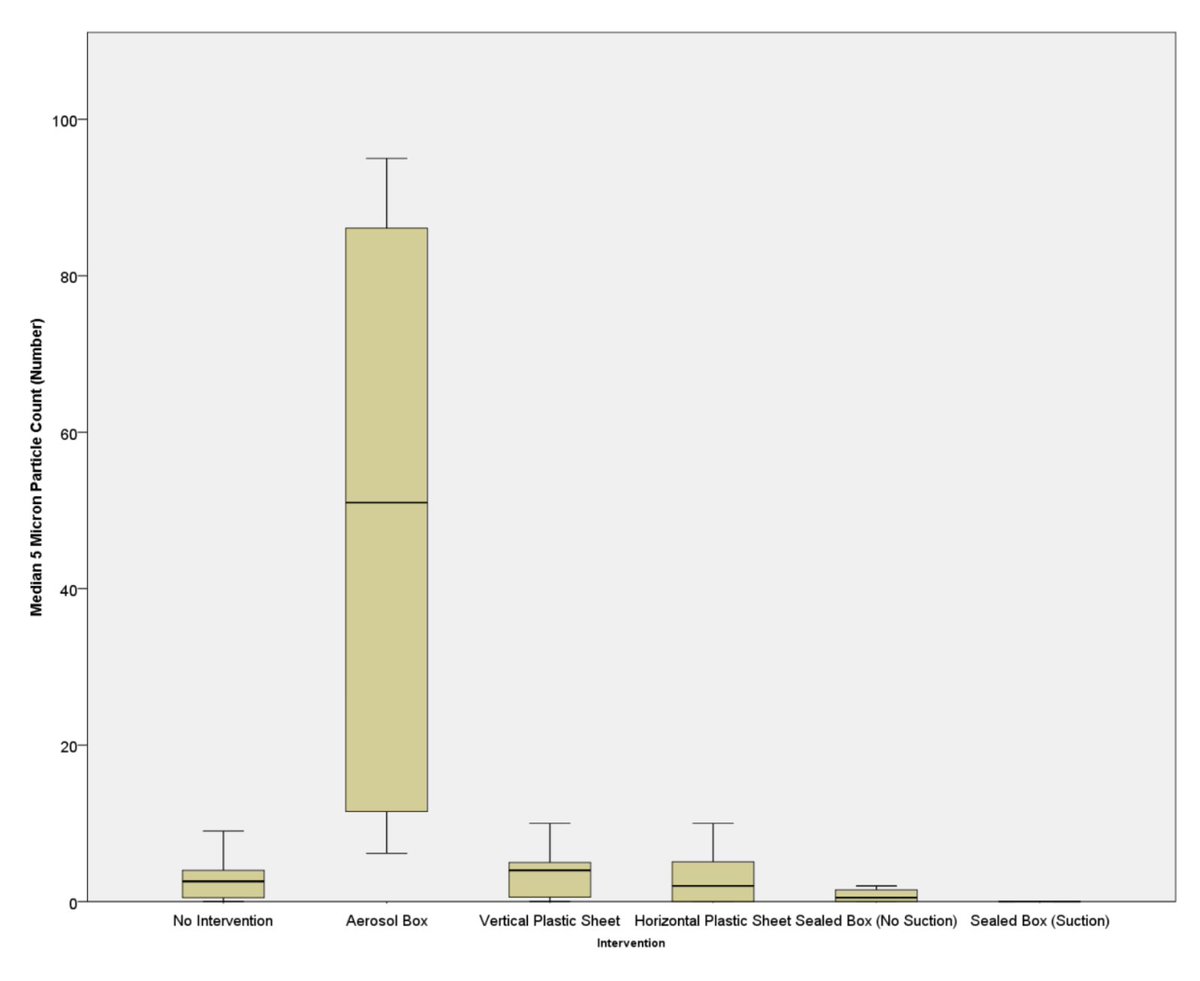
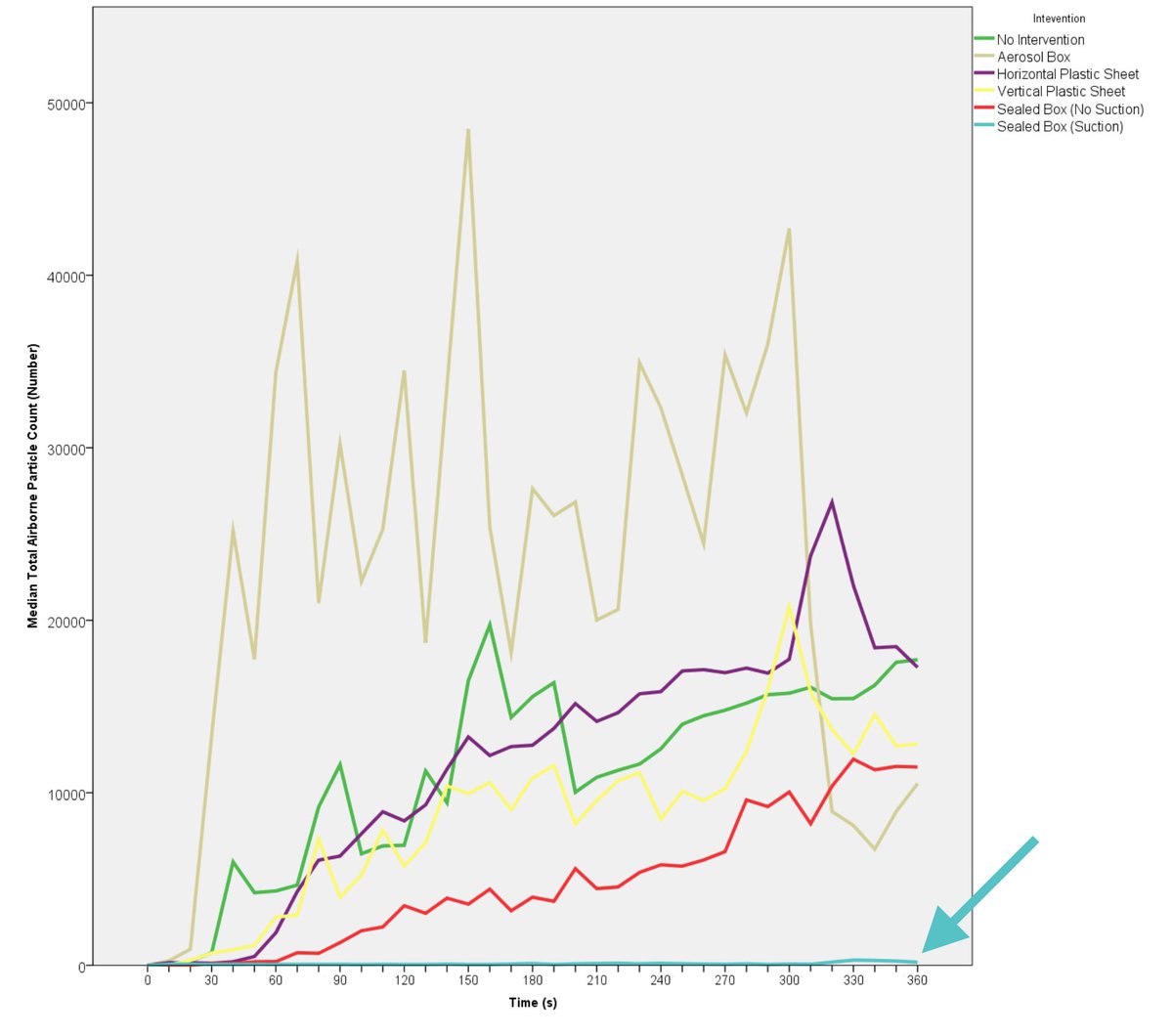
Now for results: There& #39;s heaps of data in this study if you want to look at all the tables and figures. I& #39;m just going to give a summary here, but the full paper is open-access (thanks @Anaes_Journal!) so have a look in detail if you& #39;re keen.
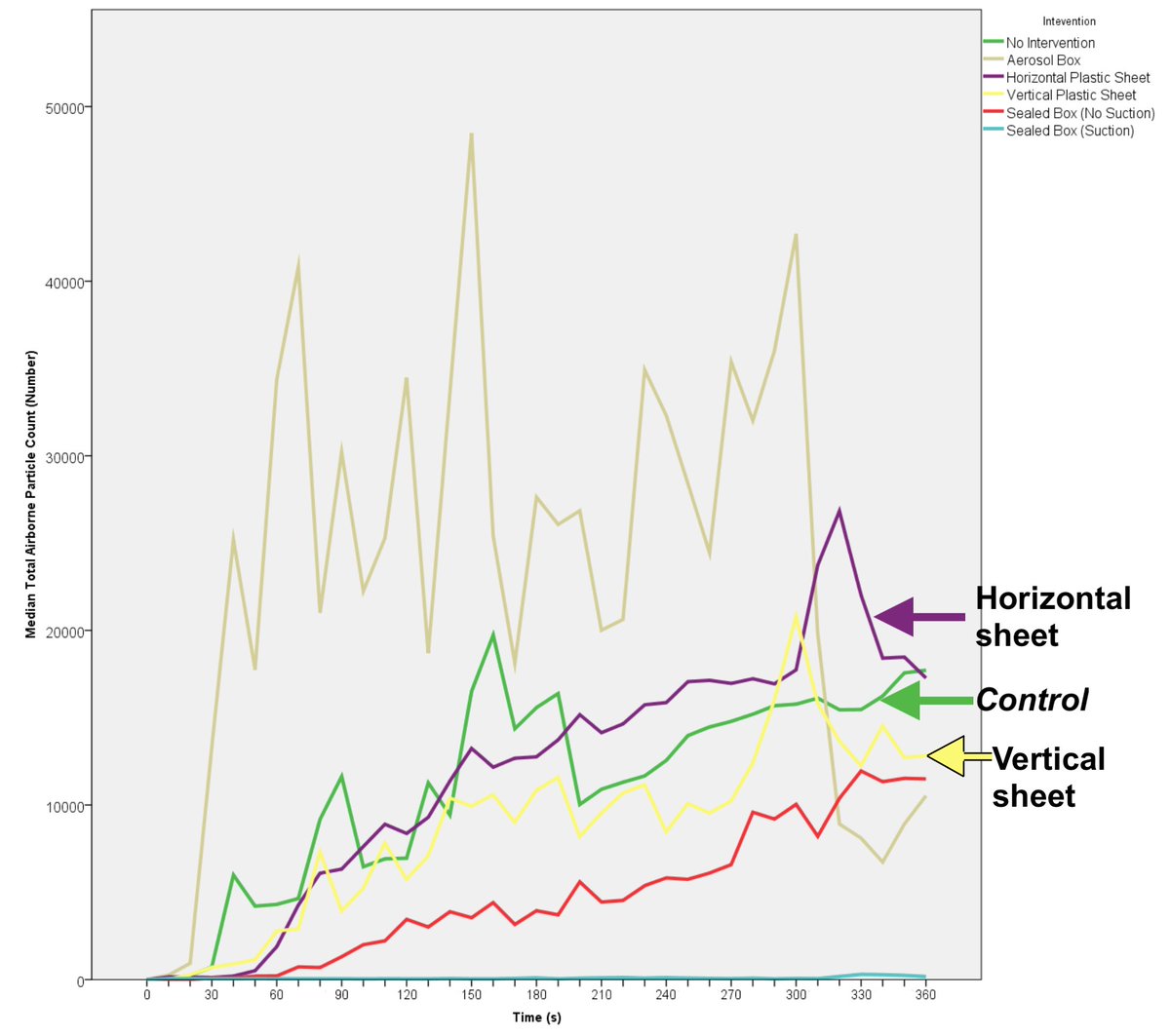
Intubating under plastic drapes: neither the vertical (yellow line) nor horizontal drape (purple line) arrangement reduced the clinician’s exposure to aerosol. Plastic drapes don’t help, according to this study.
Results for the box were more interesting. Exposure to aerosols were actually _increased_ by using the box! (statistically significant).
They suggested this may be due to the Bernoulli principle causing aerosol to & #39;jet& #39; [my word, not theirs] out the armholes onto the clinician!
They suggested this may be due to the Bernoulli principle causing aerosol to & #39;jet& #39; [my word, not theirs] out the armholes onto the clinician!
The difference is even more impressive when you look at the 5um aerosol droplet size. Just look how much additional aerosol the clinician is exposed to when using the aerosol box!
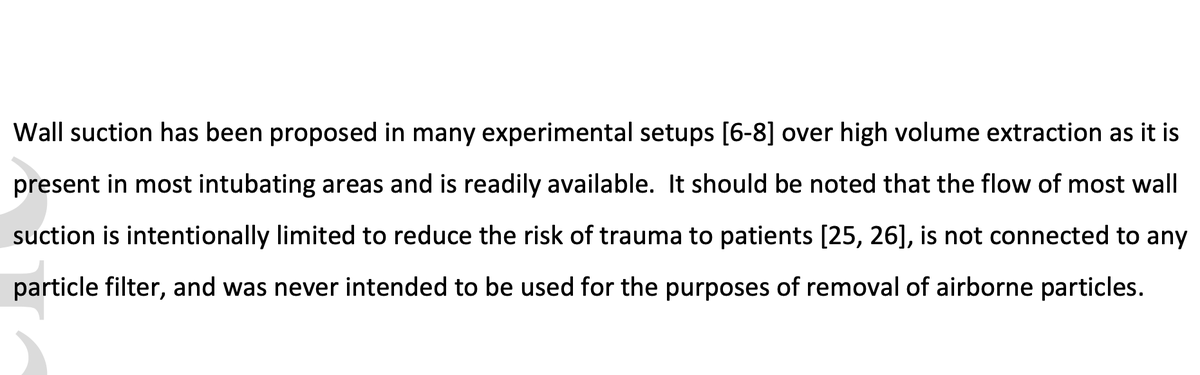
OK, there was two more barriers studied: a fully-contained box with and without suction. The fully-contained box with suction was the only device that offered some protection.
So we should use these, right?! We have a solution!? Well, unfortunately not...
So we should use these, right?! We have a solution!? Well, unfortunately not...
This final box was truely contained: instead of arm-holes it had fixed rubber gloves, and a neoprene synthetic-rubber sheet around the patient and "its design renders tracheal intubation mechanically impossible." I gather that it basically served as a negative control.
Summary:
This is an excellent study where doctors actually engaged an engineer to answer an engineering question!
This is an excellent study where doctors actually engaged an engineer to answer an engineering question!
The aerosol box _increased_ the exposure of the clinician! So not only do they delay intubation, but the best study that we have (this one) suggests these may increase your risk of COVID19!
Even if only for selfish reasons, any use of these should be discontinued immediately.
Even if only for selfish reasons, any use of these should be discontinued immediately.
Plastic drapes, studied in two different orientations, offered no protection. Therefore I cannot see any reason why someone would use them now -- they only pose risk of interfering with patient care for no benefit.
Could it have been predicated that aerosol boxes increase risk to staff? Yes; many did in fact. The mechanism might not have been predicted, but the potential for cobra effect was foreseeable.
We need to investigate any "good ideas" before implementation. https://twitter.com/SpontVentGA/status/1244577555320942593?s=20">https://twitter.com/SpontVent...
We need to investigate any "good ideas" before implementation. https://twitter.com/SpontVentGA/status/1244577555320942593?s=20">https://twitter.com/SpontVent...

 Read on Twitter
Read on Twitter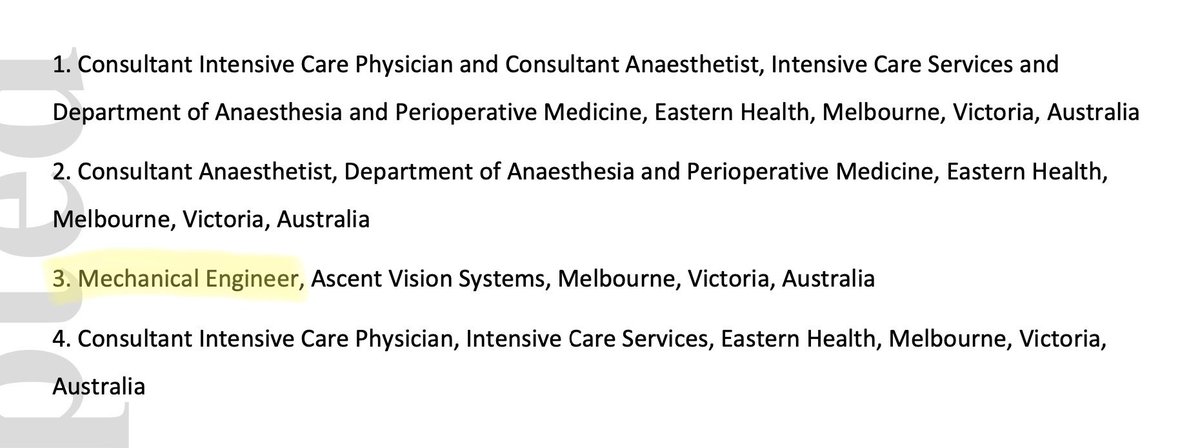





![Results for the box were more interesting. Exposure to aerosols were actually _increased_ by using the box! (statistically significant).They suggested this may be due to the Bernoulli principle causing aerosol to & #39;jet& #39; [my word, not theirs] out the armholes onto the clinician! Results for the box were more interesting. Exposure to aerosols were actually _increased_ by using the box! (statistically significant).They suggested this may be due to the Bernoulli principle causing aerosol to & #39;jet& #39; [my word, not theirs] out the armholes onto the clinician!](https://pbs.twimg.com/media/EbI-Da1UMAAe0rX.jpg)