I am finishing residency with a very heavy heart. Yes, I& #39;m celebrating this joyful accomplishment. But just below the surface there is a lot of sorrow to wade through. I haven& #39;t metabolized it fully, but want to share where I am now...
A thread. 1/
A thread. 1/
I started residency just hoping I would make it through. I got so depressed in medical school, and couldn& #39;t imagine getting through internship. I knew there was a world of problems out there, but I had to focus on me. 2/
My internship was punctuated by 2 deaths by suicide at my institution—one resident, one medical student. I didn& #39;t know them, but their deaths deeply shaped me. I grieved. I took time off. I realized I had survived something they had not. It terrified me to my core. 3/
My recovery from depression include self-facing care. But it also included a critique of the medical education system I train in. Mainstream medical culture is hierarchical, abusive, and exploitative. No, not everyone in it. But the system. 4/
I found power in writing and telling my story. My undergrad degree in Women& #39;s and Gender Studies taught me how to interpret individual, lived experience through a lens of examining systems of power. I applied this to my own life. 5/
But even as I articulated this, I still struggled. In January of this year, right before the pandemic, I had a horrible, horrible experience on a 27 hour ICU call. Nightmarish. I can& #39;t even talk about it yet. I believe so deeply that these shifts are inhumane and exploitative. 6/
And then the pandemic happened. I will be honest: at first it was exciting. I had a clear purpose with incredible support. I was learning a lot. I felt like I was on a mission in the truest sense.
And then the horror set in. 7/
And then the horror set in. 7/
I will never forget the night I stood in an emergency dept wing converted into an ICU. I looked around at some 8 patients, all intubated, all Covid. My patient was on a stretcher. He had a vent I had never seen before. He had a transport monitor. 8/
He was dying and I had to tell his family. While I stood holding my phone so his family could say their goodbyes, I looked around that room. My thought was, "This is what Italy looked like." I realized I was standing in the middle of a nightmare. 9/
There were horribly difficult ethics of whether our patients with covid, in multiorgan failure, should get CPR. These decisions... what goes said and unsaid... who I felt I could trust... what I felt I could live with... it is difficult at a soul level. 10/
Very, very quickly it was obvious the pandemic would exacerbate injustice. One of my first Covid patients was from Riker& #39;s Island. I remembering thinking, "it will be carnage there." I felt sick imagining it. Knowing that stealing a backpack can get 3 years there. 11/
Then I began seeing the numbers of Black and Latinx patients dying at ~2x the rate of White patients. And I realized I wasn& #39;t surprised. I had to think about why that was. The answer seemed to be the biggest lesson of my residency. 12/
I have received my residency training in a "colorblind" segregated healthcare system in NYC. And before you dare think "oh thank goodness I& #39;m not there" hear me out. I think my experience reflects this entire country in a way. 13/
https://journals.sagepub.com/doi/pdf/10.1177/0020731416689549">https://journals.sagepub.com/doi/pdf/1...
https://journals.sagepub.com/doi/pdf/10.1177/0020731416689549">https://journals.sagepub.com/doi/pdf/1...
Leaving the VA out for second (that is a separate topic), I went back and forth between public and private NYC medicine. For 3 years I have been proud to be part of NYC public medicine. But the differences between these systems that so many of us accept are so stark. 14/
now let me be VERY clear. I am *not* here to critique my public hospital colleagues. No one is above critique, true. But we make do in an underfunded system. We provide care that other parts of the country flatly deny. For example: routine dialysis for undocumented patients. 15/
My fear of upsetting the powers at be have kept me from commenting on the obvious differences between private and public medicine in NYC. But that makes you wonder, if you wouldn& #39;t want people to know, maybe there is something there. 16/
In my public hospital, we struggle (I mean, pleading phone calls, do the labor ourselves) to get blood draws, transport, and physical therapy. There is a constant scarcity mentality. A constant sense that you have to fight the system to get anything done for your patients. 17/
At the private hospital, patients have private rooms the size of Manhattan studios. They have flat screen TVs as wide as my bed. You put an order in, and it happens without a phone call, without a struggle. It& #39;s so confusing going back and forth between these worlds. 18/
Learning about racism & other forms of oppression is a long process and I have lots of work to do. These last few weeks, I& #39;ve been so grateful for Black scholars, activists, and HCWs who& #39;ve helped me expand my frameworks to interpret what I& #39;ve witnessed in residency. 19/
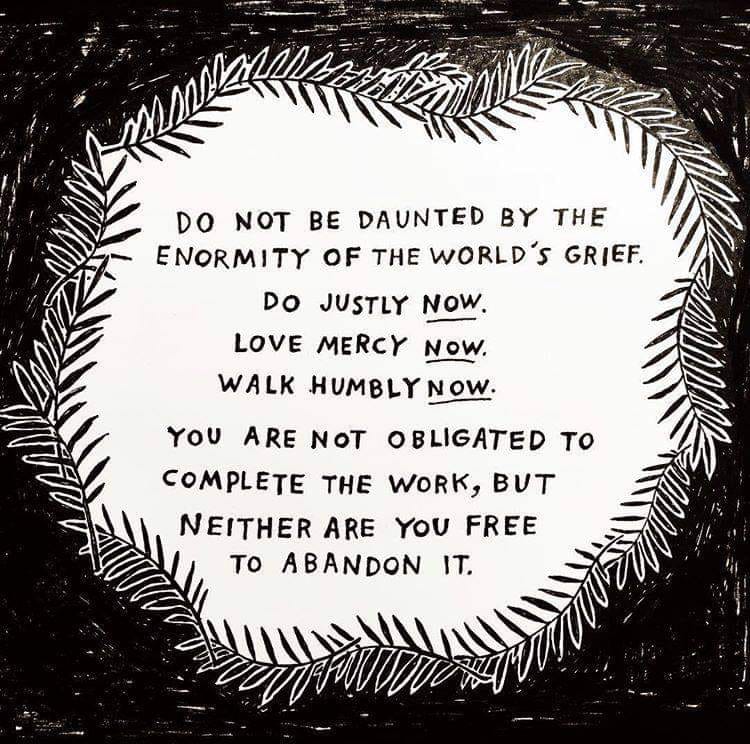
I started residency thinking a lot about how I would survive it. And I did. I learned I am much stronger than I know. I learned that many of my suspicions about the problems of medical hierarchies were just as true as I thought as a student. 20/

 Read on Twitter
Read on Twitter