#FDA recently approved #pembrolizumab- a tissue agnostic indication in metastatic tumors with high #TMB (>10 mut/MB) using Foundation One Dx companion diagnostic test. I want to share a tweetorial on why this indication could be problematic and hope to share some nuances on #TMB
I hope to cover the following
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">What is TMB ?
https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">What is TMB ?
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">Why is it important?
https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">Why is it important?
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> Controversy regarding appropriate cut-offs for TMB
https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> Controversy regarding appropriate cut-offs for TMB
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">Finally KN-158-study based on which the approval was gained
https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">Finally KN-158-study based on which the approval was gained
https://bit.ly/2BgbYSt ">https://bit.ly/2BgbYSt&q... (Lawrence et al)
https://bit.ly/2YfWRS5 ">https://bit.ly/2YfWRS5&q... (Alexandrov et al)
Lawrence et al had  https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts">3,083 tumor/normal pairs across 27 tumors, 2,957 whole-exome and 126 whole-genome
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts">3,083 tumor/normal pairs across 27 tumors, 2,957 whole-exome and 126 whole-genome
Alexandrov et al had  https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts">7,042 samples of 30 tumor types (507 whole genome and 6,535 exomes)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts">7,042 samples of 30 tumor types (507 whole genome and 6,535 exomes)
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts">Both showed tumors towards the right not only had higher mutation burden-but also had the most success with immunotherapy initially
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts">Both showed tumors towards the right not only had higher mutation burden-but also had the most success with immunotherapy initially
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts">BTW both papers are one of the most highly cited
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts">BTW both papers are one of the most highly cited
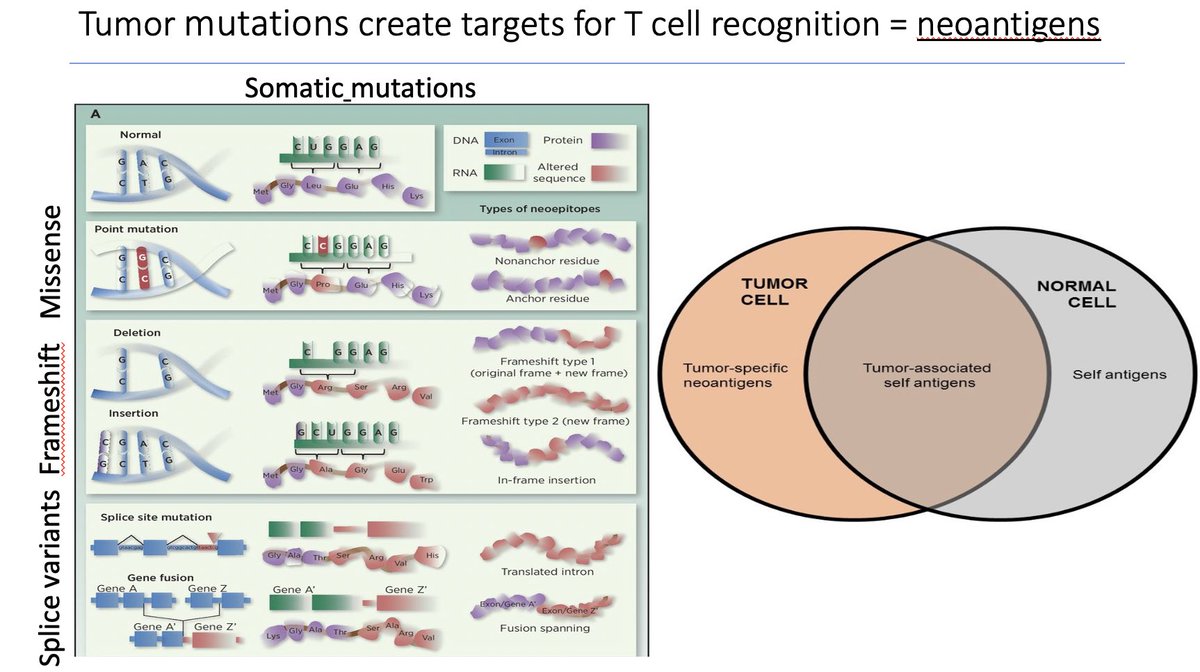
Tumor mutations creates targets for T-cell recognition=  https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌟" title="Leuchtender Stern" aria-label="Emoji: Leuchtender Stern">neoantigens
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌟" title="Leuchtender Stern" aria-label="Emoji: Leuchtender Stern">neoantigens https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌟" title="Leuchtender Stern" aria-label="Emoji: Leuchtender Stern">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌟" title="Leuchtender Stern" aria-label="Emoji: Leuchtender Stern">
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts">TMB was thought to be a surrogate marker for neoantigen burden
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts">TMB was thought to be a surrogate marker for neoantigen burden https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">immunogenecity
https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">immunogenecity https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">susceptibility to checkpoint blockade
https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">susceptibility to checkpoint blockade
Random slide on tumor mutations
Random slide on tumor mutations
First two papers to validate this:
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts">Snyder et al in melanoma with CTLA-4 blockade https://bit.ly/3fPDup5
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts">Snyder et al in melanoma with CTLA-4 blockade https://bit.ly/3fPDup5
https://bit.ly/3fPDup5&q... class="Emoji" style="height:16px;" src=" https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts">Rizvi et al in NSCLC with PD-L1 blockade https://bit.ly/2AOYPzW
https://bit.ly/2AOYPzW&q... class="Emoji" style="height:16px;" src=" https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts"> #TMB determined by whole exome sequencing (protein coding regions of 20,000 genes or~1% whole genome)
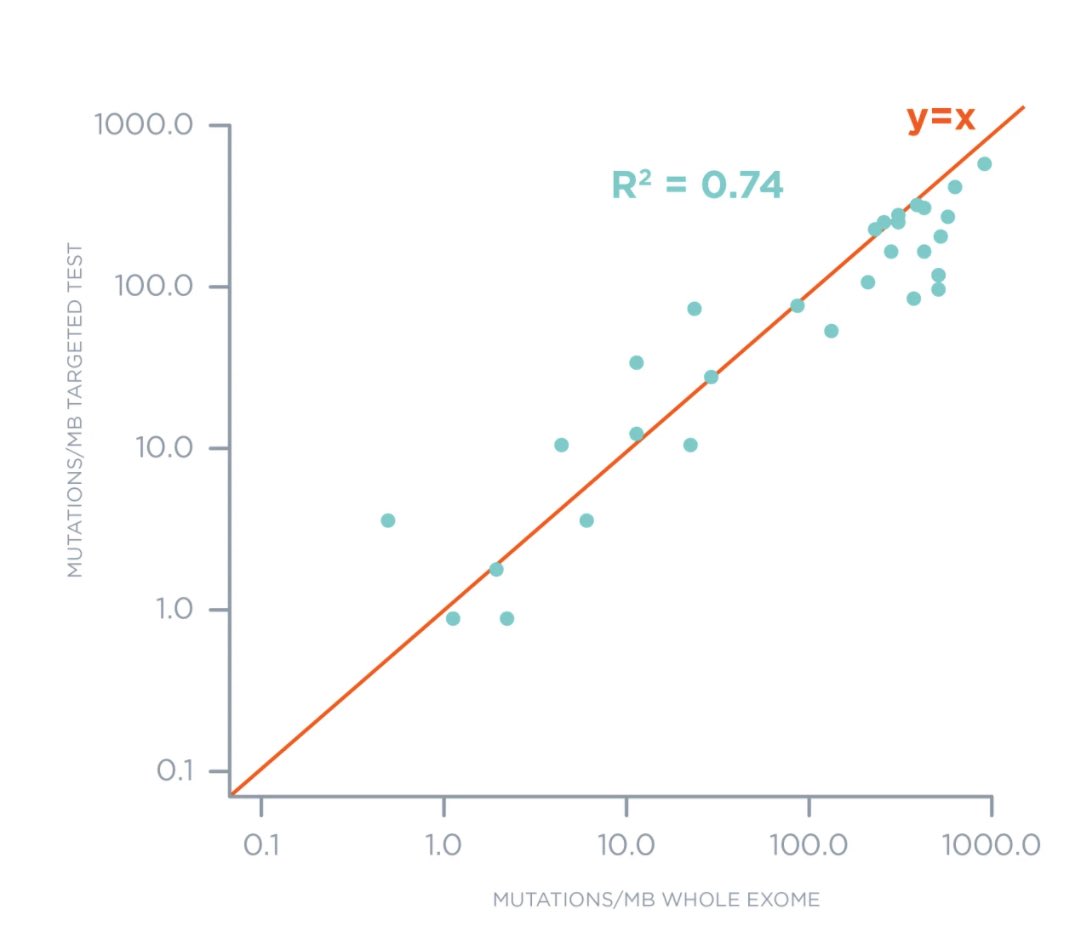
Next comes our friendly assay #FoundationOne
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">~300+ gene panel (only a subset of entire exome/20,000 genes)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">~300+ gene panel (only a subset of entire exome/20,000 genes)
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> Only mutations in tumor specimens (no germline comparison)-bioinformatically filter out potential germline variants (not perfect)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> Only mutations in tumor specimens (no germline comparison)-bioinformatically filter out potential germline variants (not perfect)
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> Both synonymous & non-synonymous
https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> Both synonymous & non-synonymous
First they showed a good concordance between #TMB determined by whole-exome approach and the #FoundationOne panel ( https://bit.ly/3eiJHcs )">https://bit.ly/3eiJHcs&q...
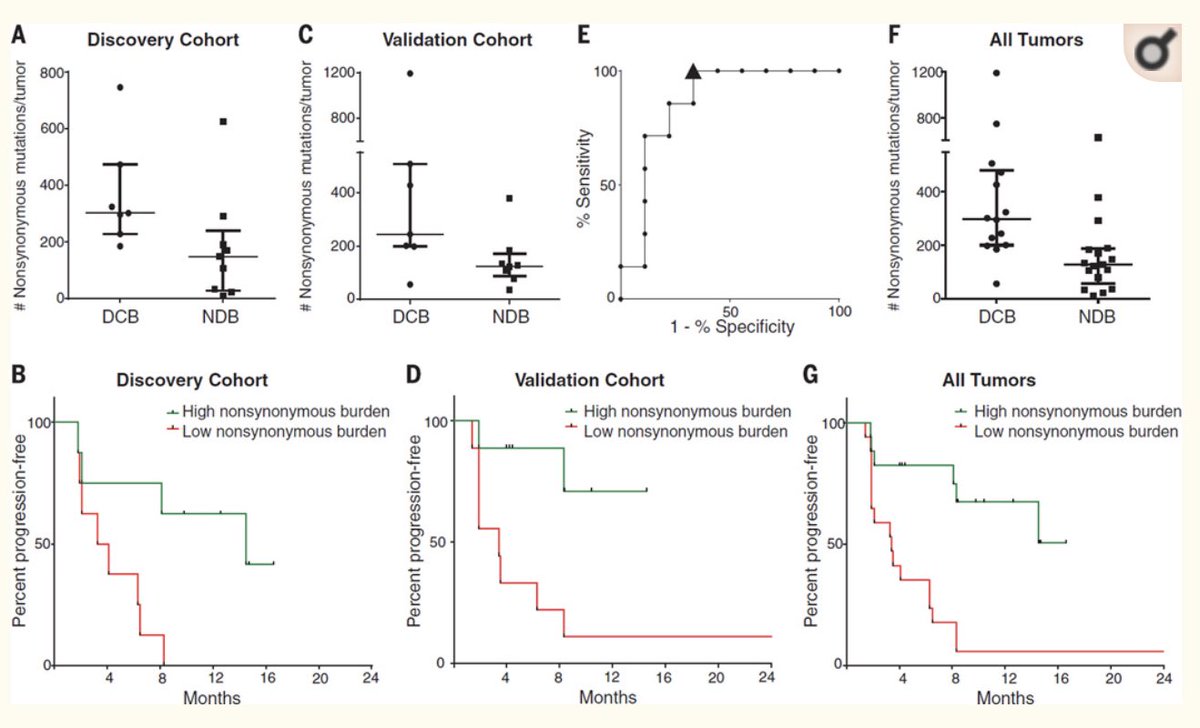
Next they showed that Higher #TMB by #FoundationOne was a/w betters outcome with single agent anti-PD1 (RR, PFS and OS) compared to low or intermediate #TMB by @PatelOncology @Dr_R_Kurzrock
https://bit.ly/2AS7nG9
https://bit.ly/2AS7nG9&q... class="Emoji" style="height:16px;" src=" https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts">Interestingly, this finding was not true with nivo+ipi combo
https://bit.ly/2AS7nG9
High #TMB >20 mut/MB (roughly 270 mut/exome)
Intermediate #TMB 6-19 mut/MB
Low #TMB 1-5 mut/MB
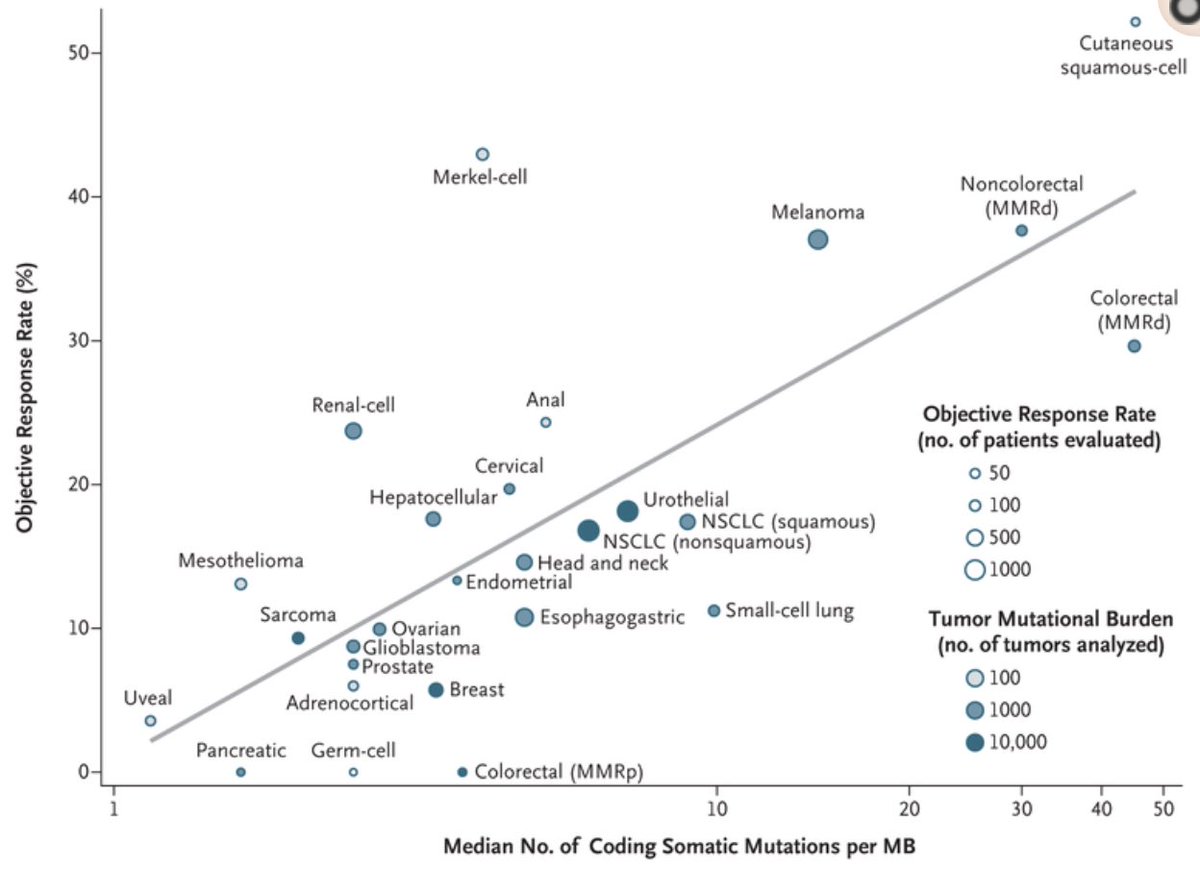
Clever paper by @MarkYarchoan from @hopkinskimmel showed correlation between response-rate and #TMB as continuous variable (no cut-off) https://bit.ly/3dejQ4m ">https://bit.ly/3dejQ4m&q...
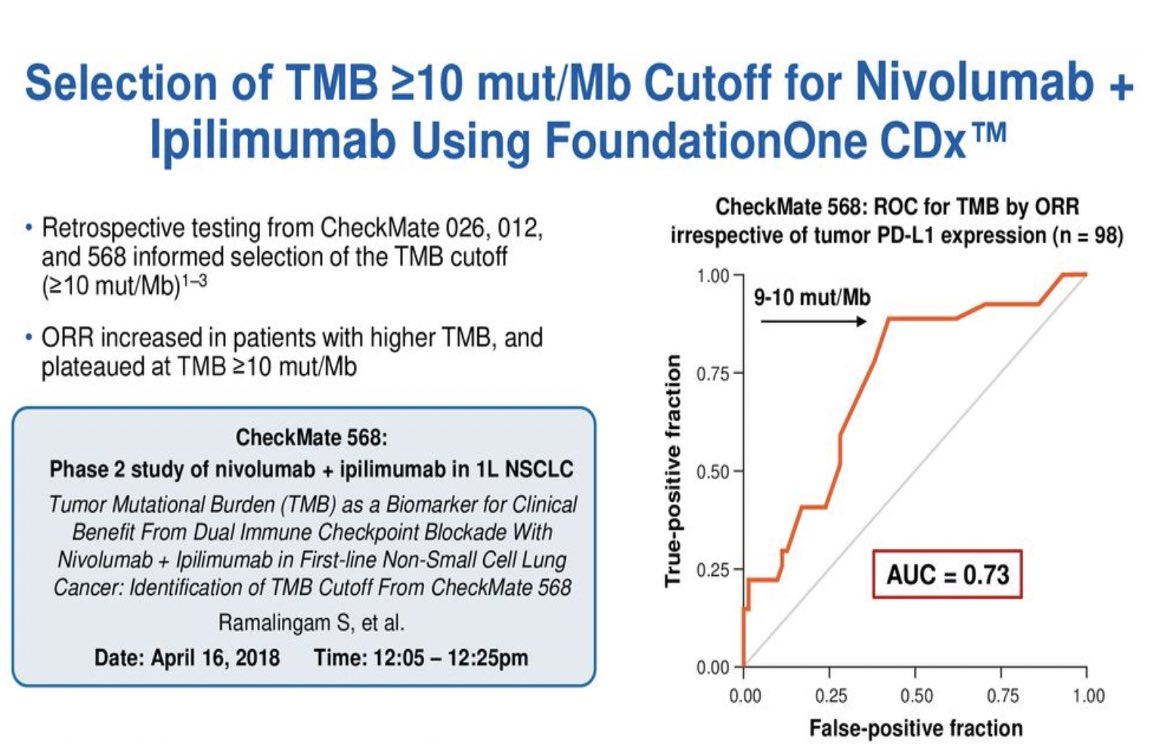
Why did #FoundationOne & #39;s definition of High TMB change over time from 20 mut/MB to 10 mut/MB , what was the justification?
This was the best I could find.
This was the best I could find.
Based off-retrospective studies of CM-026, 012 and 568, where in ROC curve of #TMB by ORR, beyond 10 mut/Mb the ORR plateaued. Basis of CM-227, the first prospective clinical trial using #TMB >10 mut/MB in NSCLC which was also predictive of PFS benefit https://bit.ly/2zKz3wh ">https://bit.ly/2zKz3wh&q...
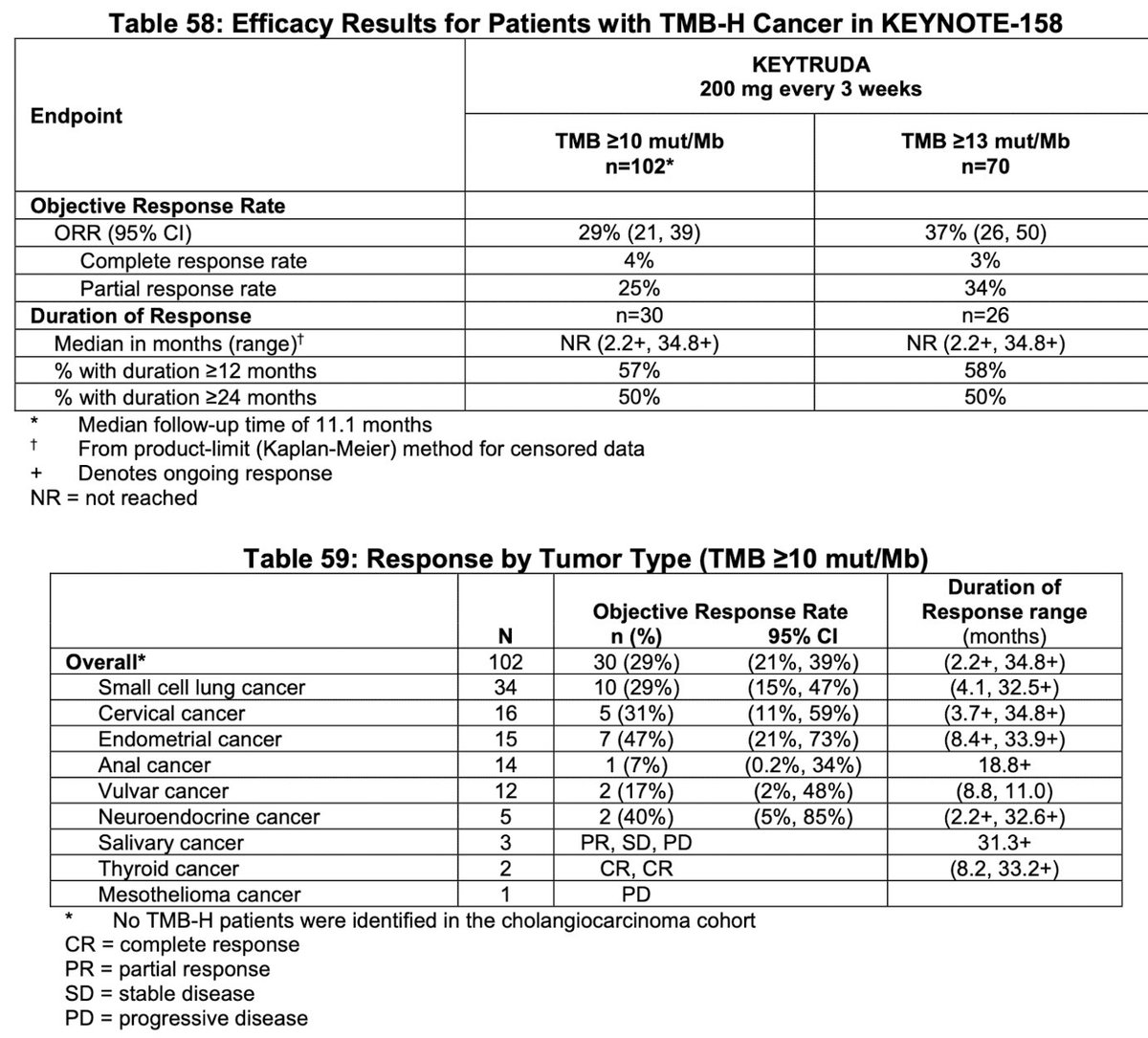
Lastly, KN-158 study- prospectively-planned retrospective analysis of 10 cohorts of patients with various previously treated unresectable or metastatic TMB-H solid tumors enrolled in a multicenter, non-randomized, open-label trial receiving pembrolizumab, ORR as primary endpoint
This is the most important table: Thanks to @agrothey for providing this. The approval was based off of these 100 patients in 10 tumor types
Curious to hear thoughts from the experts @VivekSubbiah @Dr_R_Kurzrock @StephenVLiu @n8pennell @VPrasadMDMPH @oncology_bg @Alfdoc2 @PatelOncology @JackWestMD @FAndreMD @DSolit @CharuAggarwalMD

 Read on Twitter
Read on Twitter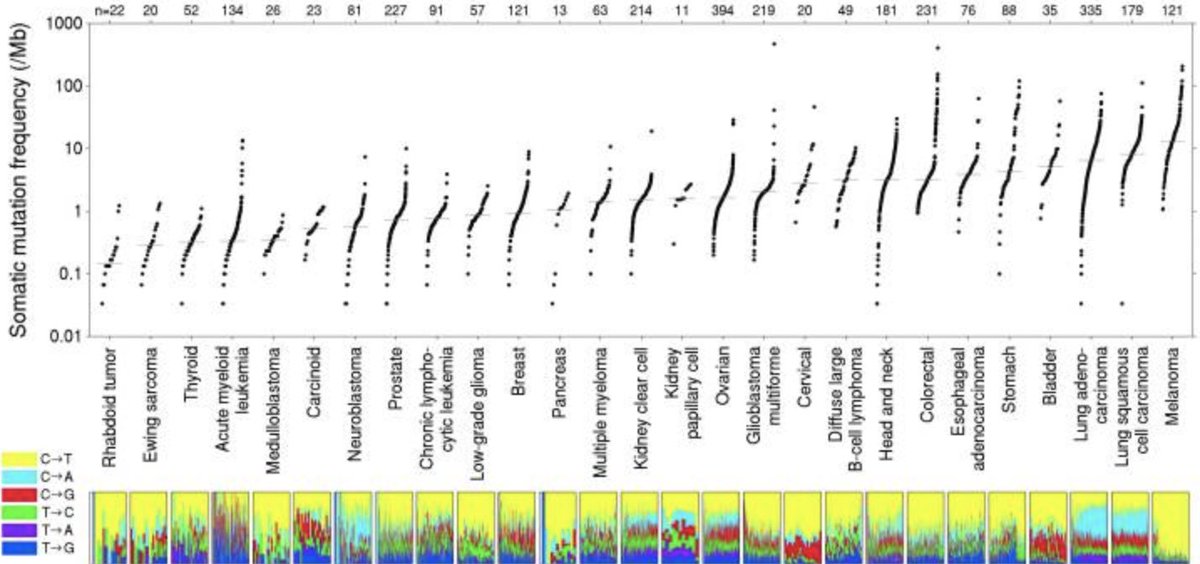 3,083 tumor/normal pairs across 27 tumors, 2,957 whole-exome and 126 whole-genome" title="Lawrence et al had https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts">3,083 tumor/normal pairs across 27 tumors, 2,957 whole-exome and 126 whole-genome" class="img-responsive" style="max-width:100%;"/>
3,083 tumor/normal pairs across 27 tumors, 2,957 whole-exome and 126 whole-genome" title="Lawrence et al had https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts">3,083 tumor/normal pairs across 27 tumors, 2,957 whole-exome and 126 whole-genome" class="img-responsive" style="max-width:100%;"/>
 neoantigenshttps://abs.twimg.com/emoji/v2/... draggable="false" alt="🌟" title="Leuchtender Stern" aria-label="Emoji: Leuchtender Stern">https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts">TMB was thought to be a surrogate marker for neoantigen burdenhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">immunogenecityhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">susceptibility to checkpoint blockadeRandom slide on tumor mutations" title="Tumor mutations creates targets for T-cell recognition= https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌟" title="Leuchtender Stern" aria-label="Emoji: Leuchtender Stern">neoantigenshttps://abs.twimg.com/emoji/v2/... draggable="false" alt="🌟" title="Leuchtender Stern" aria-label="Emoji: Leuchtender Stern">https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts">TMB was thought to be a surrogate marker for neoantigen burdenhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">immunogenecityhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">susceptibility to checkpoint blockadeRandom slide on tumor mutations" class="img-responsive" style="max-width:100%;"/>
neoantigenshttps://abs.twimg.com/emoji/v2/... draggable="false" alt="🌟" title="Leuchtender Stern" aria-label="Emoji: Leuchtender Stern">https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts">TMB was thought to be a surrogate marker for neoantigen burdenhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">immunogenecityhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">susceptibility to checkpoint blockadeRandom slide on tumor mutations" title="Tumor mutations creates targets for T-cell recognition= https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌟" title="Leuchtender Stern" aria-label="Emoji: Leuchtender Stern">neoantigenshttps://abs.twimg.com/emoji/v2/... draggable="false" alt="🌟" title="Leuchtender Stern" aria-label="Emoji: Leuchtender Stern">https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts">TMB was thought to be a surrogate marker for neoantigen burdenhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">immunogenecityhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">susceptibility to checkpoint blockadeRandom slide on tumor mutations" class="img-responsive" style="max-width:100%;"/>
 Snyder et al in melanoma with CTLA-4 blockade https://bit.ly/3fPDup5&q... class="Emoji" style="height:16px;" src=" " title="First two papers to validate this: https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts">Snyder et al in melanoma with CTLA-4 blockade https://bit.ly/3fPDup5&q... class="Emoji" style="height:16px;" src=" " class="img-responsive" style="max-width:100%;"/>
Snyder et al in melanoma with CTLA-4 blockade https://bit.ly/3fPDup5&q... class="Emoji" style="height:16px;" src=" " title="First two papers to validate this: https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts">Snyder et al in melanoma with CTLA-4 blockade https://bit.ly/3fPDup5&q... class="Emoji" style="height:16px;" src=" " class="img-responsive" style="max-width:100%;"/>
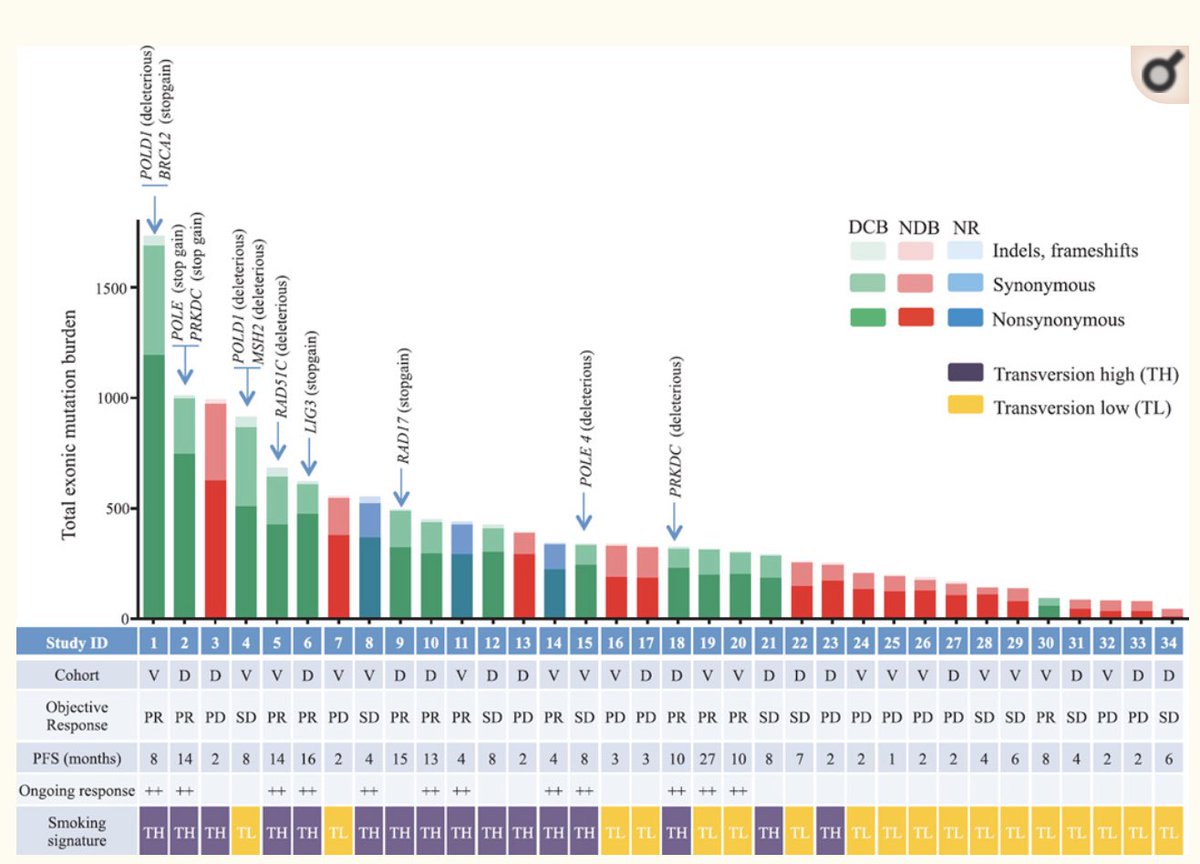
 Rizvi et al showed that higher somatic non-synonymous mutation burden was associated with clinical efficacy of pembrolizumab (synonymous mutations not analyzed)https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts">High #TMB defined as > 209 non-synonymous mutations/exome (come back to this later)" title="https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts">Rizvi et al showed that higher somatic non-synonymous mutation burden was associated with clinical efficacy of pembrolizumab (synonymous mutations not analyzed)https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts">High #TMB defined as > 209 non-synonymous mutations/exome (come back to this later)" class="img-responsive" style="max-width:100%;"/>
Rizvi et al showed that higher somatic non-synonymous mutation burden was associated with clinical efficacy of pembrolizumab (synonymous mutations not analyzed)https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts">High #TMB defined as > 209 non-synonymous mutations/exome (come back to this later)" title="https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts">Rizvi et al showed that higher somatic non-synonymous mutation burden was associated with clinical efficacy of pembrolizumab (synonymous mutations not analyzed)https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts">High #TMB defined as > 209 non-synonymous mutations/exome (come back to this later)" class="img-responsive" style="max-width:100%;"/>
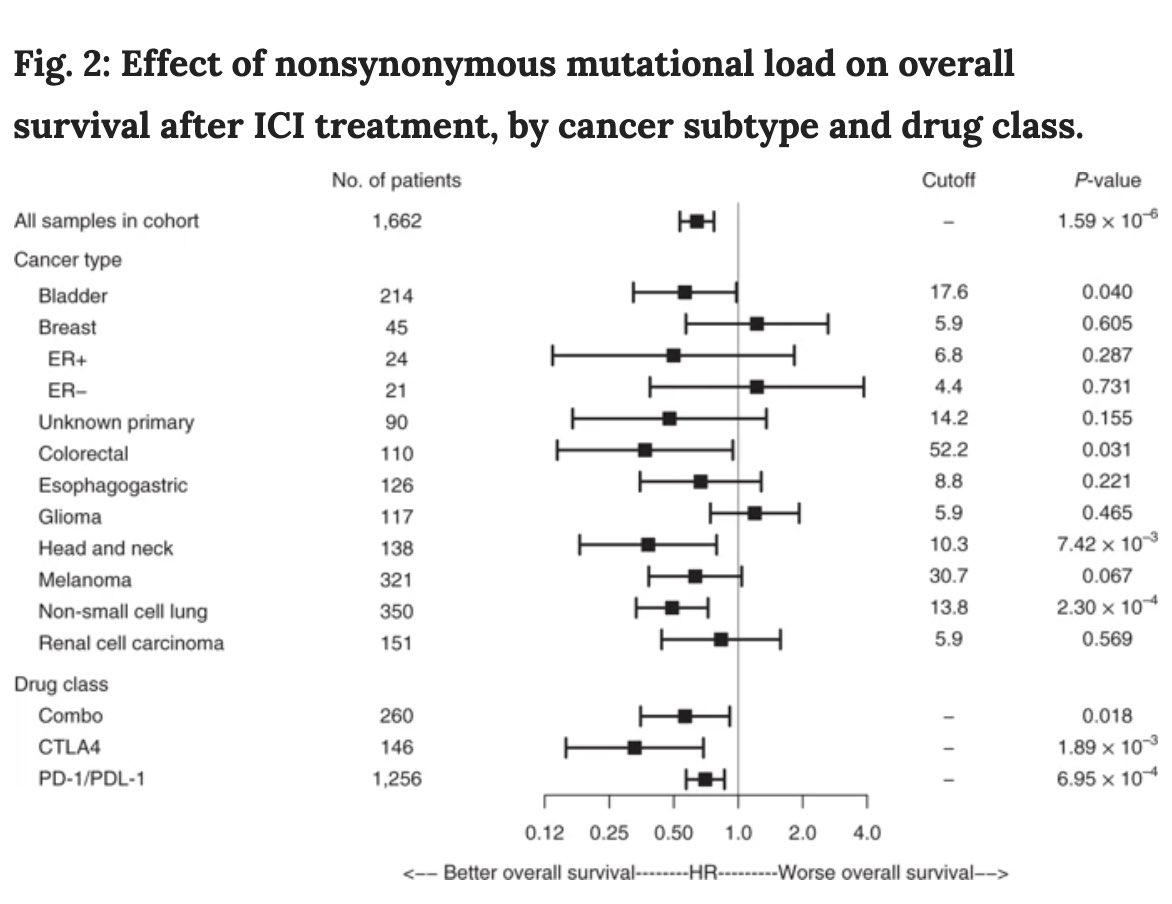 Lastly, IMO every tumor type has its own cut-off or threshold for High #TMB to be able to elicit response and improve survival with immunotherapy -shown in this elegant paper https://bit.ly/2YPRw2N&q... class="Emoji" style="height:16px;" src=" " title="https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts">Lastly, IMO every tumor type has its own cut-off or threshold for High #TMB to be able to elicit response and improve survival with immunotherapy -shown in this elegant paper https://bit.ly/2YPRw2N&q... class="Emoji" style="height:16px;" src=" " class="img-responsive" style="max-width:100%;"/>
Lastly, IMO every tumor type has its own cut-off or threshold for High #TMB to be able to elicit response and improve survival with immunotherapy -shown in this elegant paper https://bit.ly/2YPRw2N&q... class="Emoji" style="height:16px;" src=" " title="https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts">Lastly, IMO every tumor type has its own cut-off or threshold for High #TMB to be able to elicit response and improve survival with immunotherapy -shown in this elegant paper https://bit.ly/2YPRw2N&q... class="Emoji" style="height:16px;" src=" " class="img-responsive" style="max-width:100%;"/>


