Every day I walk to work @BCMRadiology, I am asked #COVID19 screening questions and handed a mask  https://abs.twimg.com/emoji/v2/... draggable="false" alt="😷" title="Face with medical mask" aria-label="Emoji: Face with medical mask"> to wear. I investigate the reasoning behind some of the gastrointestinal screening questions further on this #meded #radres #tweetorial. 1/19
https://abs.twimg.com/emoji/v2/... draggable="false" alt="😷" title="Face with medical mask" aria-label="Emoji: Face with medical mask"> to wear. I investigate the reasoning behind some of the gastrointestinal screening questions further on this #meded #radres #tweetorial. 1/19
This was inspired by a @RSNA_Radiology article by Bhayana et al available at https://pubs.rsna.org/doi/10.1148/radiol.2020201908.">https://pubs.rsna.org/doi/10.11... An investigation by @MGHImaging of 224 abdominal imaging studies done in #COVID19 positive patients over a 2-week period. 2/19
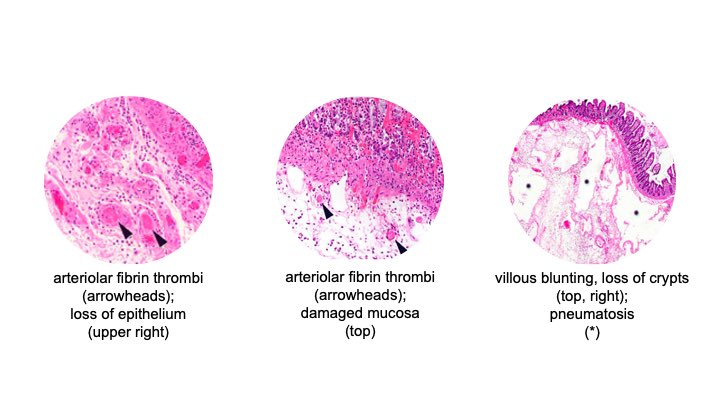
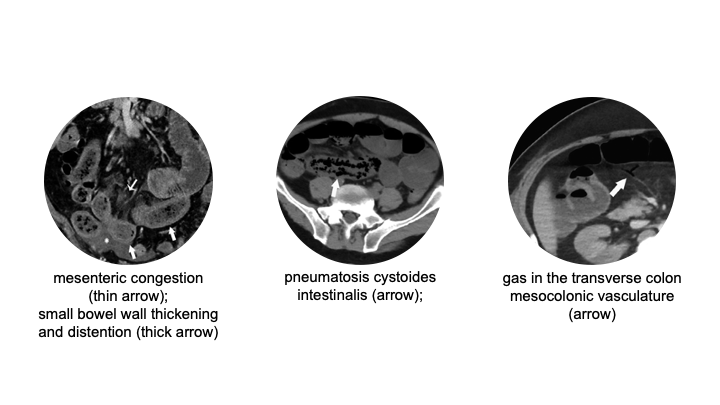
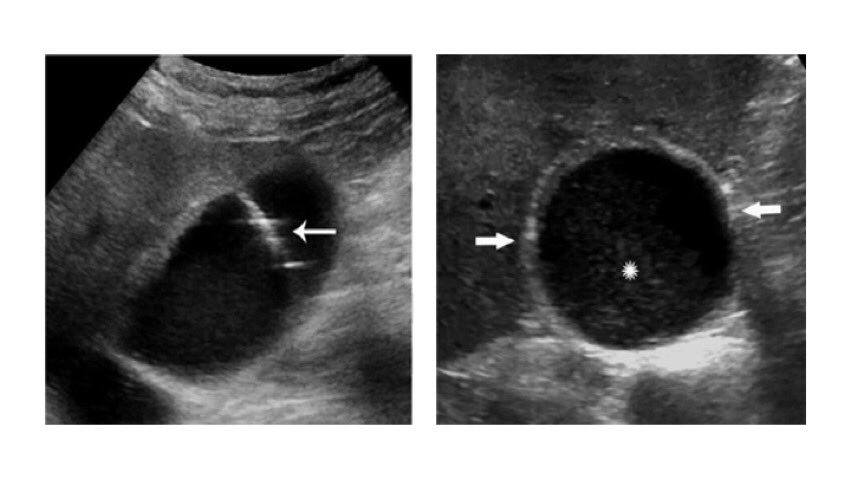
All imaging, gross pathology, and histopathology figures are taken from the manuscript. OK, a [leading] poll question to start off: Which of the following symptoms may a COVID-19 patient present with? 3/19
A. nausea
B. vomiting
C. diarrhea
D. abdominal pain
E. loss of appetite
A. nausea
B. vomiting
C. diarrhea
D. abdominal pain
E. loss of appetite
Ans: all of them. #COVID19 throughout the world continues to claim lives, now >102,000 deaths in the USA alone. While traditionally associated with respiratory symptoms, we are also seeing #COVID19 patients present with GI symptoms. 4/19
As radiologists, we may be the first to detect findings that indicate severe underlying GI pathology in known #COVID-19 patients, who may otherwise have fairly nonspecific GI symptoms. 5/19
For example, though radiographs are not very sensitive for portal venous gas (left), because they are done so prevalently, the radiologist may be the one who spots this sign for underlying bowel infarction (right). 6/19
The 224 abdominal imaging cases represented 33% of admitted #COVID19 patients. The most common indications for CT studies included abdominal pain or sepsis; the most common indication for ultrasound (US) included abnormal liver function labs. 7/19
Let’s get some pathophysiology in here. The authors discuss how lung alveolar epithelium, small bowel enterocytes, and vascular endothelium all express angiotensin converting enzyme 2 (ACE2) surface receptors, a target for #SARS_CoV_2. 8/19
Via these surface receptors, the #SARS_CoV_2 virus can enter the human host cell and proliferate from within, causing inflammation. In alveolar epithelium, this leads to lung tissue damage and ARDS. However, in the small bowel, this leads to enteritis. 9/19
What other effects have been thought to be due to #SARS_CoV_2-induced inflammation (can select more than one)? 10/19
A. pulmonary embolism
B. DVT
C. portal venous thrombosis
D. mesenteric ischemia
E. pneumatosis intestinalis
F. cholestasis
A. pulmonary embolism
B. DVT
C. portal venous thrombosis
D. mesenteric ischemia
E. pneumatosis intestinalis
F. cholestasis
Ans: A, B, D, E. Many of the findings are related with hypercoagulability caused by ACE2 receptors on the vascular endothelium. Portal venous thrombosis was not seen. The authors suggest cholestasis in #COVID19 may be due to targeting of biliary epithelium or just ICU stay. 11/19
Histopathology in cases seen at the authors’ institution has shown fibrin thrombi within submucosal arterioles, villous blunting, loss of crypts, submucosal edema, and pneumatosis. 12/19
Among the CT cases, the authors found 31% of the #COVID19 cases showed bowel wall abnormalities. In particular, 20% of CTs done in ICU patients showed pneumatosis and/or portal venous gas. Some of the patients taken for ex-lap had bowel necrosis, but not all. 13/19
Among the US cases, the authors found cholestasis in 54% of the right upper quadrant studies. Patients with cholecystostomy tube placement had negative bacterial cultures. 14/19
So what should the radiologist should do on #COVID19 patient imaging studies? 15/19
A. rule out portal venous gas on XR
B. assume bowel abnormalities on CT means impending bowel necrosis
C. comment on any liquid stool on CT
D. assume cholestasis on US is due to biliary disease
A. rule out portal venous gas on XR
B. assume bowel abnormalities on CT means impending bowel necrosis
C. comment on any liquid stool on CT
D. assume cholestasis on US is due to biliary disease
Ans: C. Take-Away #1: XR is not sensitive enough to rule out portal venous gas, but should always look for this because it is more prevalently ordered. 16/19
Take-Away #2: Not all concerning bowel abnormalities on imaging showed bowel necrosis on ex-lap in this study, though many of the findings typically have a low threshold for referral to surgery. 17/19
Take-Away #3: Diarrhea may be the first image-apparent indication of GI manifestation of disease in #COVID19 patients, and the authors suggest we should comment on this more often when present. 18/19
Take-Away #4: The pathophysiology of increased incidence of cholestasis in #COVID19 patients is not well understood and may be correlated with their ICU stay rather than necessarily with underlying biliary targeting by #SARS_CoV_2. 19/19

 Read on Twitter
Read on Twitter