MEGATHREAD on important recent findings on immunity against SARS-CoV-2 / COVID-19, including *duration* of immunity as well as *prevalence* of immunity among BOTH recovered individuals and uninfected, “susceptible” individuals. (1/n)
I have a degree in biochemistry and did some research in a genetics lab as a student (including performing PCR), but am not an expert on immunology, so apologies if I oversimplify some issues here. Everything is sourced for you to fact-check yourself. (2/n)
As brief background, we (humans) have both an “innate” immune system (nonspecific to a given threat) and an “adaptive” immune system (specific to a given threat.) (3/n)
Given that SARS-CoV-2 is a novel virus, some initially assumed that we would have no existing adaptive response, and had to rely entirely on the “innate” immune system. (4/n)
Additionally, serology testing has so far been focused on the presence of two kinds of antibodies - IgG and IgM - in blood, to determine what fraction of the population has acquired adaptive immunity to SARS-CoV-2. (5/n)
It turns out, importantly, that IgG and IgM are not the *only* adaptive immune mechanisms against SARS-CoV-2. There are also IgA antibodies and T-cells. (6/n)
Emerging research suggests that some people (particularly young people) produce IgA antibodies in mucosal tissue to fight off SARS-CoV-2, but this may not show up in blood tests because a systemic response is never needed. (7/n)
Moreover, it is also now becoming clear that many (most?) people have some degree of existing cross-reactive T-cell immunity to SARS-CoV-2 from previous exposure to endemic “common cold” coronaviruses, or potentially other animal coronaviruses. (8/n)
These factors may contribute to explaining why COVID-19’s exponential growth tails off well before anything close to the hypothetical homogeneous herd immunity threshold (CC @MLevitt_NP2013 ) and why children are less severely affected. (9/n)
Paper 1: “Systemic and mucosal antibody secretion specific to SARS-CoV-2.” https://www.biorxiv.org/content/10.1101/2020.05.21.108308v1.full.pdf">https://www.biorxiv.org/content/1... (10/n)
The authors note that in a (small) sample of healthcare workers, 15-20% of those who had no detectable antibodies in their blood did have IgA antibodies in their mucosa, and that younger subjects were less likely to demonstrate systemic response. (11/n)
Quote: “healthcare workers with negative SARS-CoV-2-specific IgA and IgG serum titers had detectable SARS-CoV-2-specific IgA antibodies in their nasal fluids and tears.” (12/n)
Quote: “Moreover, SARS-CoV-2-specific IgA levels in nasal fluids of these healthcare workers were inversely correlated with patient age.” (13/n)
The authors go on to make several observations about the correlation between milder, pneumonia-free cases and younger subjects with mucosal-specific (rather than systemic) responses. (14/n)
Quote: “These data might be a reflection of increased mucosal immunity in the young or decreased mucosal immunity in the old.” (15/n)
Quote: “previous data on coronavirus seroprevalence of HKU1-specific IgG showed an absence of systemic HKU1-specific antibodies in individuals younger than 20 years of age, with increasing seroprevalence with increasing age.” (16/n)
My takeaways: serology testing, particularly among younger cohorts, is likely to understate actual developed acquired immunity to SARS-CoV-2, as localized antibody response may be all that is needed. (17/n)
Paper 2: Presence of SARS-CoV-2-reactive T cells in COVID-19 patients and healthy donors. https://www.medrxiv.org/content/10.1101/2020.04.17.20061440v1.full.pdf">https://www.medrxiv.org/content/1... (18/n)
Background on T cells from Wikipedia: “Unlike CD8+ killer T cells, CD4+ helper T cells function by indirectly killing cells identified as foreign: they determine if and how other parts of the immune system respond to a specific, perceived threat.” (19/n)
SARS-CoV-2 is (genomically) very similar to SARS and generally pretty different from endemic “common cold” coronaviruses - but not *entirely* different. (20/n)
SARS-CoV-2 uses the now-infamous “spike” protein to bind to human cells. It turns out that parts of this spike (though not all) are shared with endemic coronaviruses. (21/n)
Quote: “Although the overall amino acid sequence homology of spike 172 glycoproteins is relatively low among HCoV, there is an overlap of MHC-II epitopes located 173 especially in the C-terminal domain.” (22/n)
Given this overlap, it turns out that a meaningful portion - a third! - of a 68-person sample of COVID-19 negative subjects nonetheless had CD4 T cells that could recognize SARS-CoV-2. (23/n)
Quote: “We demonstrate the presence of S-reactive CD4+ 52 T cells in 83% of COVID-19 patients, 53 as well as in 34% of SARS-CoV-2 seronegative healthy donors (HD), albeit at lower frequencies.” (24/n)
Paper 3: “Targets of T cell responses to SARS-CoV-2 coronavirus.” https://www.cell.com/cell/pdf/S0092-8674(20)30610-3.pdf?_returnURL=https%3A%2F%2Flinkinghub.elsevier.com%2Fretrieve%2Fpii%2FS0092867420306103%3Fshowall%3Dtrue">https://www.cell.com/cell/pdf/... (25/n)
This paper corroborates the previous paper’s findings on reactive helper T cells among non-COVID-19 subjects, and also finds that COVID-19 patients develop both helper and killer T cells. (We’ll see why this is important later.) (26/n)
Quote: “circulating SARS-CoV-2−specific CD8+ and CD4+ T cells were identified in ~70% and 100% of COVID-19 convalescent patients, respectively.” (27/n)
Quote: “Importantly, we detected SARS-CoV-2−reactive CD4+ T cells in ~40-60% of unexposed individuals, suggesting cross-reactive T cell recognition between circulating ‘common cold’ coronaviruses and SARS-CoV-2.” (28/n)
The authors go on to discuss the potential implications of the presence of these T cells for protection against COVID-19. (29/n)
Quote: “Whether this immunity is relevant in influencing clinical outcomes is unknown… but it is tempting to speculate that the crossreactive CD4+ T cells may be of value in protective immunity, based on SARS mouse models” (30/n)
They make a comparison to influenza, where one of the reasons H1N1 (which caused the Spanish Flu) turned out to be a relative non-event in 2009 was that much of the adult population had cross-reactive immunity already. (31/n)
Quote: “In the context of the 2009 H1N1 influenza pandemic, preexisting T cell immunity existed in the adult population, which focused on the more conserved internal influenza viral proteins.” (32/n)
Quote: “The presence of crossreactive T cells was found to correlate with less severe disease. The frequent availability of crossreactive memory T cell responses might have been one factor contributing to the lesser severity of the H1N1 flu pandemic.” (33/n)
Takeaways: although we obviously haven’t yet directly observed these cross-reactive helper T cells protecting people against severe COVID-19, we have strong reason to believe that this is indeed the case. (34/n)
Final paper: “Different pattern of pre-existing SARS-COV-2 specific T cell immunity.” https://www.biorxiv.org/content/10.1101/2020.05.26.115832v1.full.pdf">https://www.biorxiv.org/content/1... (35/n)
One major question many have debated is how long acquired immunity to SARS-CoV-2 will last. This is obviously of critical importance. (36/n)
Some have pointed to data demonstrating a decline, over time, in antibody levels. This paper provides encouraging news - remember from post 27 how 70/100% of the sample of recovered COVID-19 patients had specific killer/helper T cells? (37/n)
This paper observes that although coronavirus antibodies fade over a period of several years, T cells remain detectable for much longer. (38/n)
Quote: “All [six coronaviruses] trigger antibody and T cell responses in infected patients: however, antibody levels appear to wane relatively quicker than T cells.” (39/n)
Quote: “In SARS recovered patients, SARS-CoV-specific antibodies dropped below detection limit within 2 to 3 years, while SARS-CoV-specific memory T cells can be detected even at 11 years after infection.” (40/n)
Quote: “... 17 years after infection [with SARS, those individuals still possess virus-specific memory T cells.” (41/n)
Quote: “These findings demonstrate that virus-specific memory T cells induced by betacoronavirus infection are long-lasting, which supports the notion that COVID-19 patients would develop long-term T cell immunity.” (42/n)
Moving on, the authors also corroborate the other findings above with regards to protective T cells present in subjects who have not had COVID-19. (43/n)
Quote: “This may suggest that perhaps not only human “common cold” coronaviruses, but other presently unknown coronaviruses, possibly of animal origin, can induce cross-reactive SARS-CoV-2 memory T cells in the general population.” (44/n)
Quote: “It was remarkable to find that NSP7/13-specific T cells were detected in 9 out of 18 (50%) SARS-CoV-1/2 unexposed donors, despite the fact that our analysis was performed with peptides that cover only 10% (684aa) of the ORF1 proteome (7096aa).” (45/n)
It gets a bit technical here, so I will translate after the next quote. (46/n)
“Importantly, the ORF-1 region contains domains that are extremely conserved among many different coronaviruses.” (47/n)
“The distribution of these viruses in different animal species might result in periodic human contact and subsequently induction of ORF-1-specific T cells with cross-reactive ability against SARS-CoV-2.” (48/n)
Translation: an “ORF” is an open reading frame - part of SARS-CoV-2’s genome that codes for certain proteins. (49/n)
This specific ORF, ORF-1, is “extremely conserved” among many different coronaviruses - this means that that specific sequence does not evolve/mutate much, usually because it’s pretty important. (50/n)
MedicineNet: “Evolutionarily conserved gene: A gene that has remained essentially unchanged throughout evolution. Conservation of a gene indicates that it is unique and essential.” (51/n)
So per the authors, most coronaviruses have essentially the same genetic sequence here in ORF-1. What does it code for? (52/n)
Quote: “ In coronavirus infected cells, the ORF-1 coded proteins are necessary for the formation of the viral replicase transcriptase complex in which viral replication and transcription occur.” (53/n)
Quote: “Therefore, an ORF-1-specific T cell can be envisioned to abort viral production in infected cells by lyses of SARS-CoV-2 infected cells even before the formation of mature virions.” (54/n)
Translation: T-cells that can recognize ORF-1 could help prevent the virus from replicating. To call this helpful would be an understatement. (55/n)
Returning to 48/49 above: the authors were surprised to find that half of a very small sample (18) of uninfected patients had T cells targeting proteins in this segment, likely due to previous exposure to other coronaviruses whether animal or human. (56/n)
“In individuals with no history of SARS, COVID-19 or contact with SARS/COVID-19 patients (n=18). Half of them (9/18) possess T cells targeting the ORF-1 coded proteins NSP7 and 13.” (57/n)
CONCLUSIONS. (58/n)
First, I think it’s worth discussing, briefly, the idea of heterogeneity. Here is a good tweet thread. https://twitter.com/mlipsitch/status/1258827506930667523">https://twitter.com/mlipsitch... (59/n)
Models that assume 60% is needed for “herd immunity” make a very unrealistic assumption: that human interaction is homogeneous; that is to say, that we are all just dots randomly bouncing around a box bumping into each other. (60/n)
In reality, our interactions are not random. We tend to shop at the same stores, eat at the same restaurants, work at the same workplace, visit the same friends, etc. (61/n)
Age-stratified heterogeneity in mixing is particularly important. Why? We now know that a substantial portion (sometimes 50%+) of COVID-19 deaths are from nursing homes. (62/n)
This is despite the fact that nursing homes are something like 0.6% of the population. https://twitter.com/Avik/status/1265616920000311297">https://twitter.com/Avik/stat... (63/n)
Here there is heterogeneity of both transmission and susceptibility. Obviously, most of us never actually visit a nursing home. I’ve been to a nursing home maybe 6 times in my life. Same goes for rest of my family and most of my friends. (64/n)
More sophisticated models will take into account not only the heterogeneity of mixing, but the heterogeneity of susceptibility. (65/n)
Two such models are here. https://www.medrxiv.org/content/10.1101/2020.04.27.20081893v3.full.pdf">https://www.medrxiv.org/content/1... https://arxiv.org/pdf/2005.03085.pdf">https://arxiv.org/pdf/2005.... (66/n)
Their conclusions, based on different approaches (heterogeneity of transmission and heterogeneity of susceptibility), is that herd immunity could be achieved at levels as low as 10-20% or 40% attack rates. (67/n)
Keep in mind as well the dose-dependency element. As discussed in one of the cited papers… (68/n)
“It is common to observe in humans the ability of a single virus to cause different pathological manifestations. This is often due to multiple contributory factors including the quantity of viral inoculum.” (69/n)
An interesting phenomenon that has been observed worldwide by those such as Michael Levitt ( @MLevitt_NP2013 ) and Sunetra Gupta of Oxford is that the virus appears to follow a similar trajectory regardless of interventions. (70/n)
Gupta interview here: https://unherd.com/2020/05/oxford-doubles-down-sunetra-gupta-interview/">https://unherd.com/2020/05/o... (71/n) (CC @unherd @freddiesayers)
An interesting observation, however, is that the virus has peaked at significantly different attack rates in different places. (72/n)
New York City and Northern Italy obviously saw very high symptomatic attack rates and death. Conversely, the Southern U.S., ex-Louisiana, was largely unscathed, despite locking down late and reopening early. (73/n)
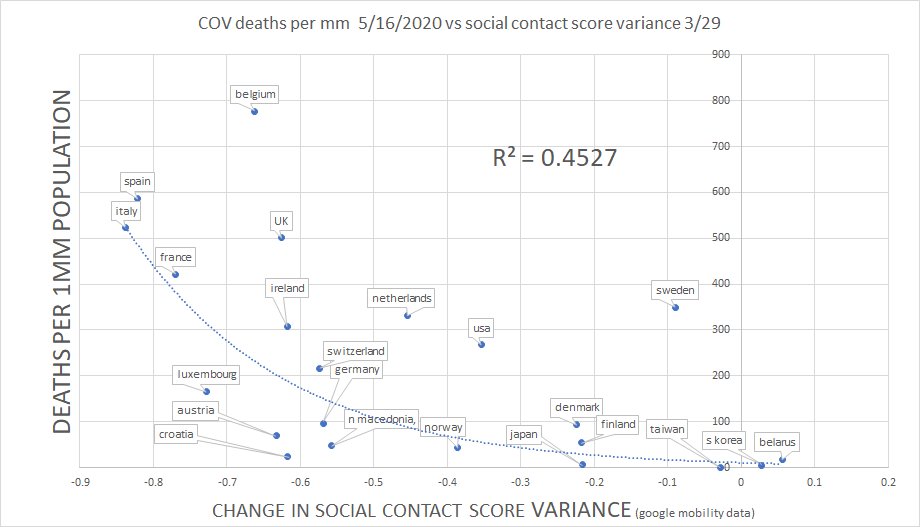
The very different experiences of countries and localities - that cannot be explained by interventions or time-aligned caseloads or even mobility data () - suggests significant heterogeneity. (74/n)
This heterogeneity could and likely is somewhat driven by geographic factors (temperature / humidity / Vitamin D status) and demographic factors (population density, age / race / health status, etc.) (75/n)
But based on the papers cited, another contributing factor may well be heterogeneity in existing adaptive immunity. (76/n)
The good news, from one of the heterogeneity papers: “More susceptible and more connected individuals have a higher propensity to be infected and thus are likely to become immune earlier.” (77/n)
We now have good hard data (in both the U.S. and Europe) demonstrating that reopening and increases in social mobility do not lead to R>1. (78/n)
This could, theoretically, be due to something entirely exogenous such as seasonality. We do know that existing coronaviruses are extremely seasonal, essentially entirely disappearing in the summer. https://academic.oup.com/jid/advance-article/doi/10.1093/infdis/jiaa161/5815743">https://academic.oup.com/jid/advan... (79/n)
The above papers about T cells and IgA responses, however, provide an interesting alternative hypothesis (both could be true). The virus could just be running out of truly “naive” susceptible individuals who are susceptible to severe infection and/or transmission. (80/n)
As we have seen, a substantial fraction of individuals - possibly above 50% - either have some pre-existing specific defenses (T cells) against SARS-CoV-2, or they are able to fight off the infection locally/mucosally without systemic immune response. (81/n)
Combining this idea with heterogeneity, this doesn’t have to confer complete, 100% immunity to prevent uncontrolled exponential spread of COVID-19. Rather, it just has to reduce likelihood of transmission (for example, by reducing viral replication.) (82/n)
Anyway, these are very interesting and optimistic findings, and hopefully more data on these topics will continue to emerge. (83/n)
@NahasNewman @Assaf_Nathan @boriquagato @ElonBachman @AlistairHaimes - you might find this thread of interest.

 Read on Twitter
Read on Twitter