In a new study, we& #39;ve measured how many children visiting a Seattle hospital have serological evidence of prior infection with #SARSCoV2: https://www.medrxiv.org/content/10.1101/2020.05.26.20114124v1
Why">https://www.medrxiv.org/content/1... is this important and what did we find? (1/14)
Why">https://www.medrxiv.org/content/1... is this important and what did we find? (1/14)
Children are under-represented in #COVID19 case counts. Are they less likely to be infected, or are their infections just overlooked because they often only get mildly sick? Serology identifies antibodies from infection independent of symptoms, so can help answer this. (2/14)
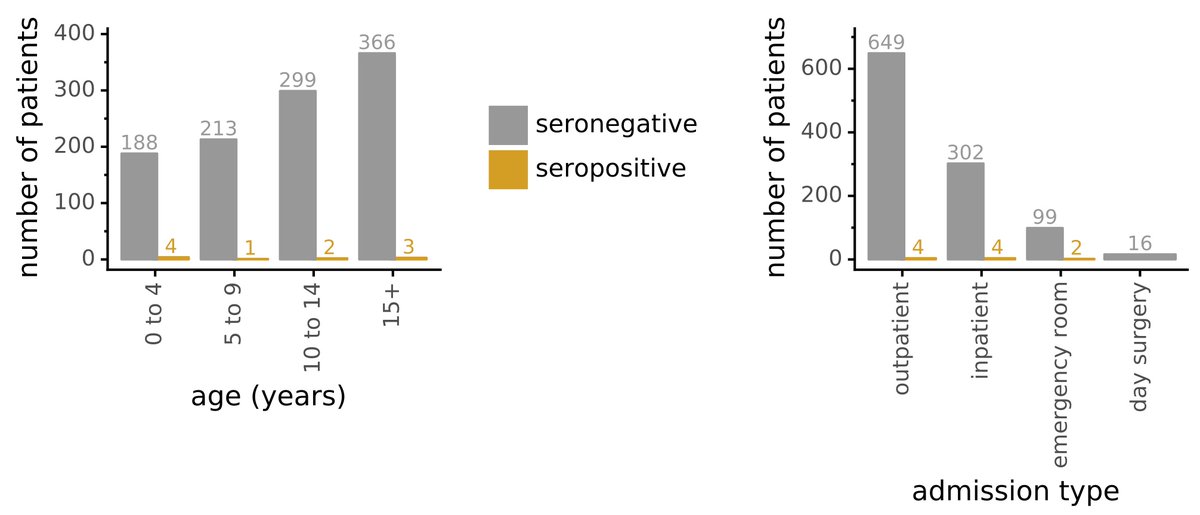
Our collaborator Jan Englund ( @seattlechildren& #39;s hospital) collected 1,775 residual serum samples from 1,076 children in March & April during early Seattle outbreak. Samples from children seeking medical care for any reason: respiratory illness, surgery, routine care, etc. (3/14)
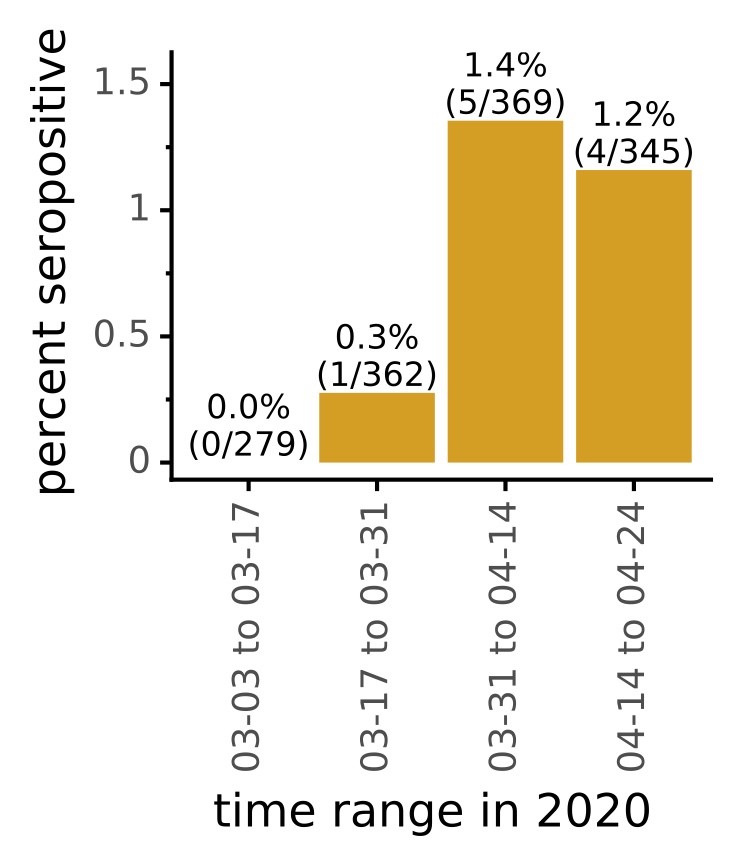
Then @AdamDingens here @fredhutch @HutchBasicSci tested sera for reactivity to #SARSCoV2 by multiple assays w/ stringent cutoffs to avoid false positives. Overall, 10 of 1,076 children were seropositive. Frequency increased from very low to bit over 1% from March to April. (4/14)
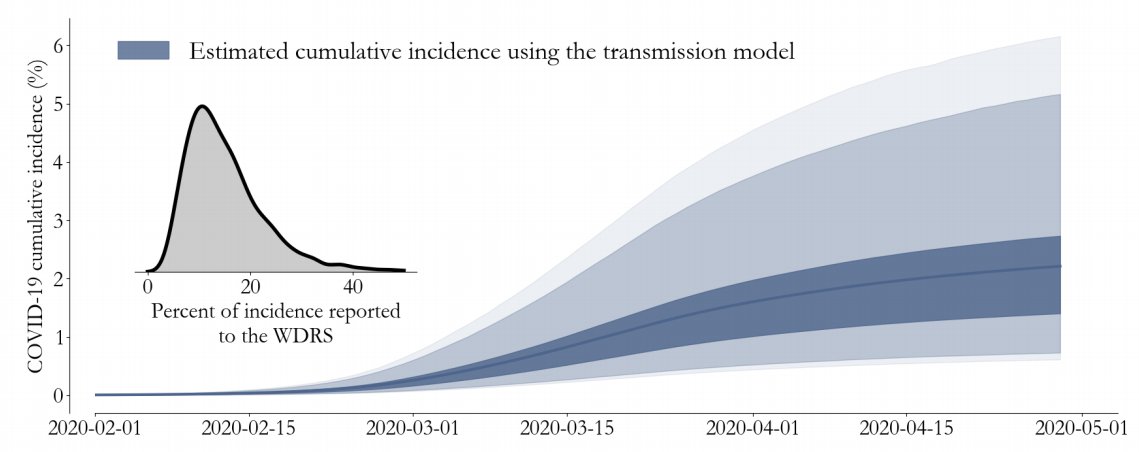
Although apples-to-oranges, @famulare_mike @IDMOD_ORG estimate from testing/mortality that all-age cumulative incidence in Seattle is 1-2% (fig from them). Our serology of children seeking medical care match their all-population estimates (takes 1-2 wks to be seropositive) (5/14)
Had seropositive children been sick? 2/10 had reported symptoms & tested + for virus. 3 others tested - for virus in routine screening pre surgery. Other 5 never tested. Also, 1 child w + viral test at <1 wk post symptom was seronegative (expected, antibodies take 1-2 wk). (6/14)
Otherwise nothing seemed different about seropositive children: about equal male vs female, of all ages, and visited hospital for a variety of inpatient / outpatient / emergency reasons. (7/14)
Then @khdcrawford ( @uwgenome @UW_MSTP grad student) measured how well seropositive children neutralized virus. 8/10 neutralized, some very potently, one >1:18,000. (Each point is different person, don& #39;t worry much about 2 non-neut children as unknown time post-infection). (8/14)
We think more systematically comparing neutralizing responses in children and adults over time is interesting area for future work, since children respond better/faster to some other viruses / vaccines. (9/14)
Overall caveats are that children-seeking medical care may not be representative of children more generally, & statistics are low as we identified only small number of seropositives. Nonetheless... (10/14)
... our results consistent w/ idea that cumulative incidence in Seattle is now approximately 1-2% across many groups, and that child infections are often being missed by viral testing. (11/14)
Thanks to many people who enabled study. Jan Englund & her group had vision to start saving residual sera @seattlechildren& #39;s hospital in early March; @AdamDingens designed study & performed almost all experiments @fredhutch along with @khdcrawford & Rachel Eguia. Plus... (12/14)
@HelenChuMD helped compare children to adults. @florian_krammer @FatimaAmanat were AMAZING in sharing serology reagents/protocols w us (& many others) as soon as they developed them. @KingLabIPD @veeslerlab @coronalexington enabled study by making spike and RBD antigen. (13/14).
Finally, all raw & processed serological data is available as supp files, along with as much clinical data as can share without compromising privacy (so binned by date, age, etc). Lots of interest in cutoffs in serology studies, so dig into data to see for yourself! (14/14)

 Read on Twitter
Read on Twitter