Appreciated the opportunity to comment on 2 excellent cohort studies led by @jLewnard (Kaiser) and @leorahorwitzmd (NYU) in @bmj_latest that give us a much better understanding of who gets sick from #COVID19. A thread putting this work into perspective https://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Down pointing backhand index" aria-label="Emoji: Down pointing backhand index">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Down pointing backhand index" aria-label="Emoji: Down pointing backhand index">
https://www.bmj.com/content/369/bmj.m2082.full">https://www.bmj.com/content/3...
https://www.bmj.com/content/369/bmj.m2082.full">https://www.bmj.com/content/3...
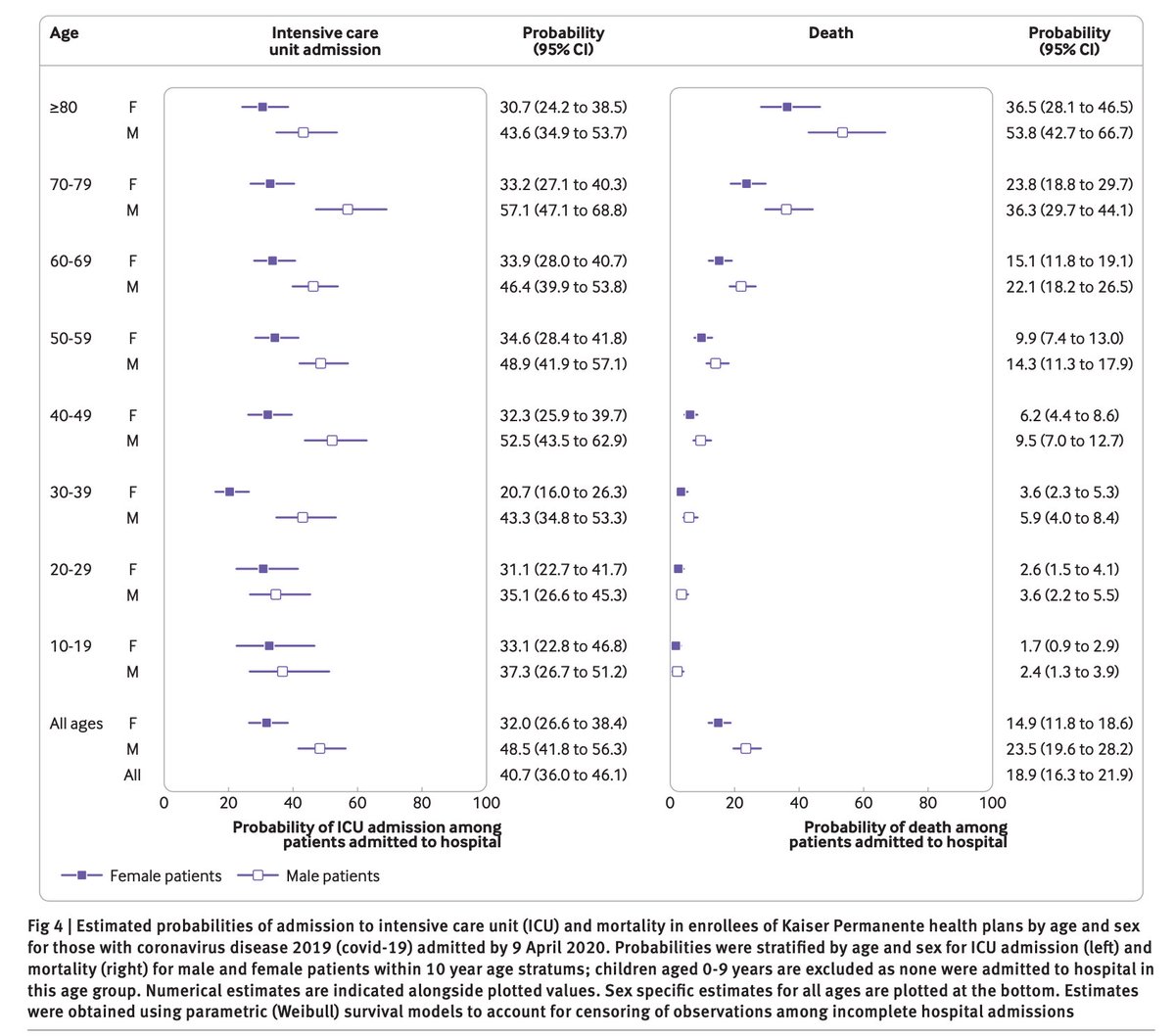
2/ Take away #1: It& #39;s not just the elderly who get sick.
Most who were hospitalized for #COVID19 were *under* the age of 65:
- 53% (n=1,452) in NYU cohort
- 60% (n=1,108) in Kaiser
Most who were hospitalized for #COVID19 were *under* the age of 65:
- 53% (n=1,452) in NYU cohort
- 60% (n=1,108) in Kaiser
3/ Take away #2: Those who were hospitalized spent 1-2 weeks in hospital. A trip to the hospital is no joke.
Median length of stay (75th percentile)
- NYU cohort: 7 days (13 days)
- Kaiser cohort: 10 days (17 days)
Median length of stay (75th percentile)
- NYU cohort: 7 days (13 days)
- Kaiser cohort: 10 days (17 days)
4/ Take away #3: A high proportion of #covid19 patients admitted to the hospital developed critical illness (life-support on a ventilator, ICU care, death, or discharge to hospice):
- NYU cohort: 36% (n=990)
- Kaiser cohort: 41% (n=749)
That& #39;s a lot of ICU admissions/beds
- NYU cohort: 36% (n=990)
- Kaiser cohort: 41% (n=749)
That& #39;s a lot of ICU admissions/beds
5/ Take away #4: Similar to prior studies, there are consistent patient characteristics that are more common in those who are high risk from #covid19 (hospitalization, critical illness, or death):
- Older age
- Male
- Obesity
- History of heart failure
- Older age
- Male
- Obesity
- History of heart failure
6/ The Kaiser cohort study presents a striking visualization showing that even after adjusting for key patient characteristics, men had worse outcomes than women in every age group.
Fellas, #WearAMask. Trust me, you do not want to roll the dice. (Ladies too)
Fellas, #WearAMask. Trust me, you do not want to roll the dice. (Ladies too)
7/ Take away #5: compelling evidence is provided in the NYU study on predictors of critical illness:
- elevated inflammatory markers, in particular: elevated d-dimer, c-reactive protein, troponin
- O2 sat <92% (speaks to potential value of walk tests in ED and home monitoring)
- elevated inflammatory markers, in particular: elevated d-dimer, c-reactive protein, troponin
- O2 sat <92% (speaks to potential value of walk tests in ED and home monitoring)
8/ Take away #6: decreased transmission rates were found in the Kaiser insured population corresponding to the time when social distancing policies were enacted:
- March 1 - infected patient transmitted to 1.3-2.5 others
- April 1 - infected patient transmitted to 0.8-0.9 others
- March 1 - infected patient transmitted to 1.3-2.5 others
- April 1 - infected patient transmitted to 0.8-0.9 others
9/ Most intrigued by decreasing mortality over time in NYU cohort. Potential reasons worth looking into:
- hospital capacity strain improved
- changes in care (e.g. proning or better ventilator management)
- changes in meds (e.g. more anticoagulation, less hydroxycholoroquine?)
- hospital capacity strain improved
- changes in care (e.g. proning or better ventilator management)
- changes in meds (e.g. more anticoagulation, less hydroxycholoroquine?)
10/ To wrap up, why are these #covid19 hospitalization studies important? Because for every person that succumbs to this terrible illness, four more will fight for days in the hospital. It& #39;s not just about risk of death. See prior thread: https://twitter.com/kit_delgadoMD/status/1264921326407561216?s=20">https://twitter.com/kit_delga...
11/ Kudos again to the study authors @leorahorwitzmd
and @jLewnard and colleagues for the rigorous work in a short amount of time.
Enjoyed working with awesome co-authors to put this together (rising super star @georgeanesi and the always wise @ScottHalpernMD)
and @jLewnard and colleagues for the rigorous work in a short amount of time.
Enjoyed working with awesome co-authors to put this together (rising super star @georgeanesi and the always wise @ScottHalpernMD)

 Read on Twitter
Read on Twitter https://www.bmj.com/content/3..." title="Appreciated the opportunity to comment on 2 excellent cohort studies led by @jLewnard (Kaiser) and @leorahorwitzmd (NYU) in @bmj_latest that give us a much better understanding of who gets sick from #COVID19. A thread putting this work into perspectivehttps://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Down pointing backhand index" aria-label="Emoji: Down pointing backhand index"> https://www.bmj.com/content/3..." class="img-responsive" style="max-width:100%;"/>
https://www.bmj.com/content/3..." title="Appreciated the opportunity to comment on 2 excellent cohort studies led by @jLewnard (Kaiser) and @leorahorwitzmd (NYU) in @bmj_latest that give us a much better understanding of who gets sick from #COVID19. A thread putting this work into perspectivehttps://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Down pointing backhand index" aria-label="Emoji: Down pointing backhand index"> https://www.bmj.com/content/3..." class="img-responsive" style="max-width:100%;"/>