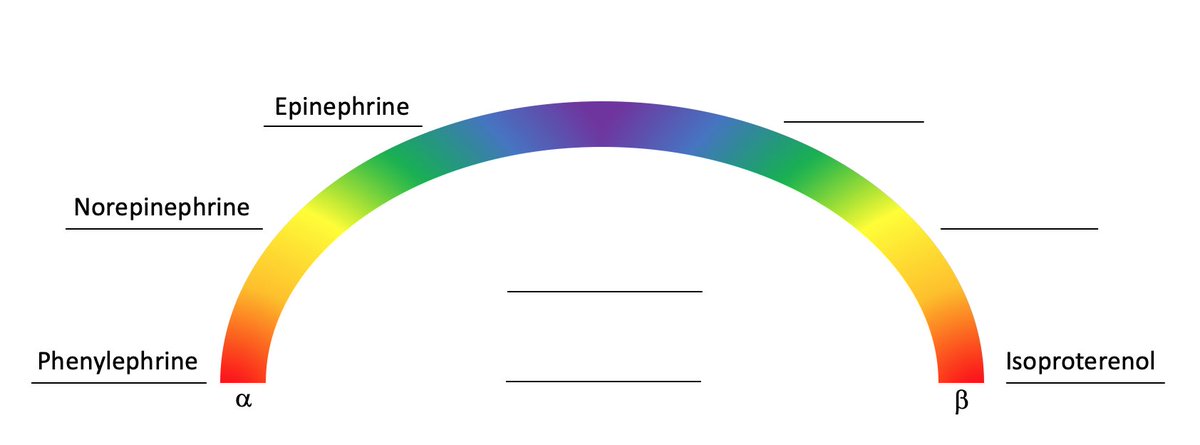
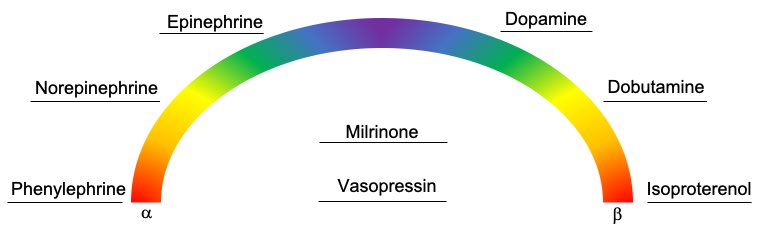
1/ Levo, Neo, Vaso oh my! Many interns worry about understanding these agents of the ICU/CCU. Here is a little #tweetorial #medtweetorial on a fun way to think about them, taught to me by my own senior, the pressor rainbow! Let’s #presstherainbow #medtwitter #MedStudentTwitter
2/ skip to the end for the final diagram, but don& #39;t forget as every graduation speech mentions, “Its the not the destination, It& #39;s the journey”. Before we start defending the MAP lets first look at the receptors we are going to be manipulating because #physiology is fun!
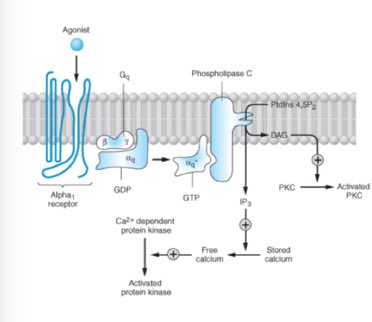
3/ Lets start with the a1 receptor, specifically those seen in the smooth muscles of our peripheral vasculature. Activation of these receptor -> activation of phopholipase C ->  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> release of free calcium -> smooth muscle contraction or VASOCONSTRICTION
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> release of free calcium -> smooth muscle contraction or VASOCONSTRICTION  https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol"> https://abs.twimg.com/emoji/v2/... draggable="false" alt="💪" title="Flexed biceps" aria-label="Emoji: Flexed biceps">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💪" title="Flexed biceps" aria-label="Emoji: Flexed biceps"> https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">
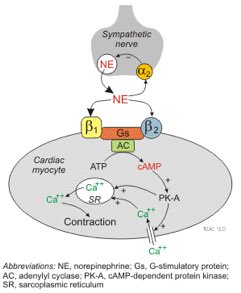
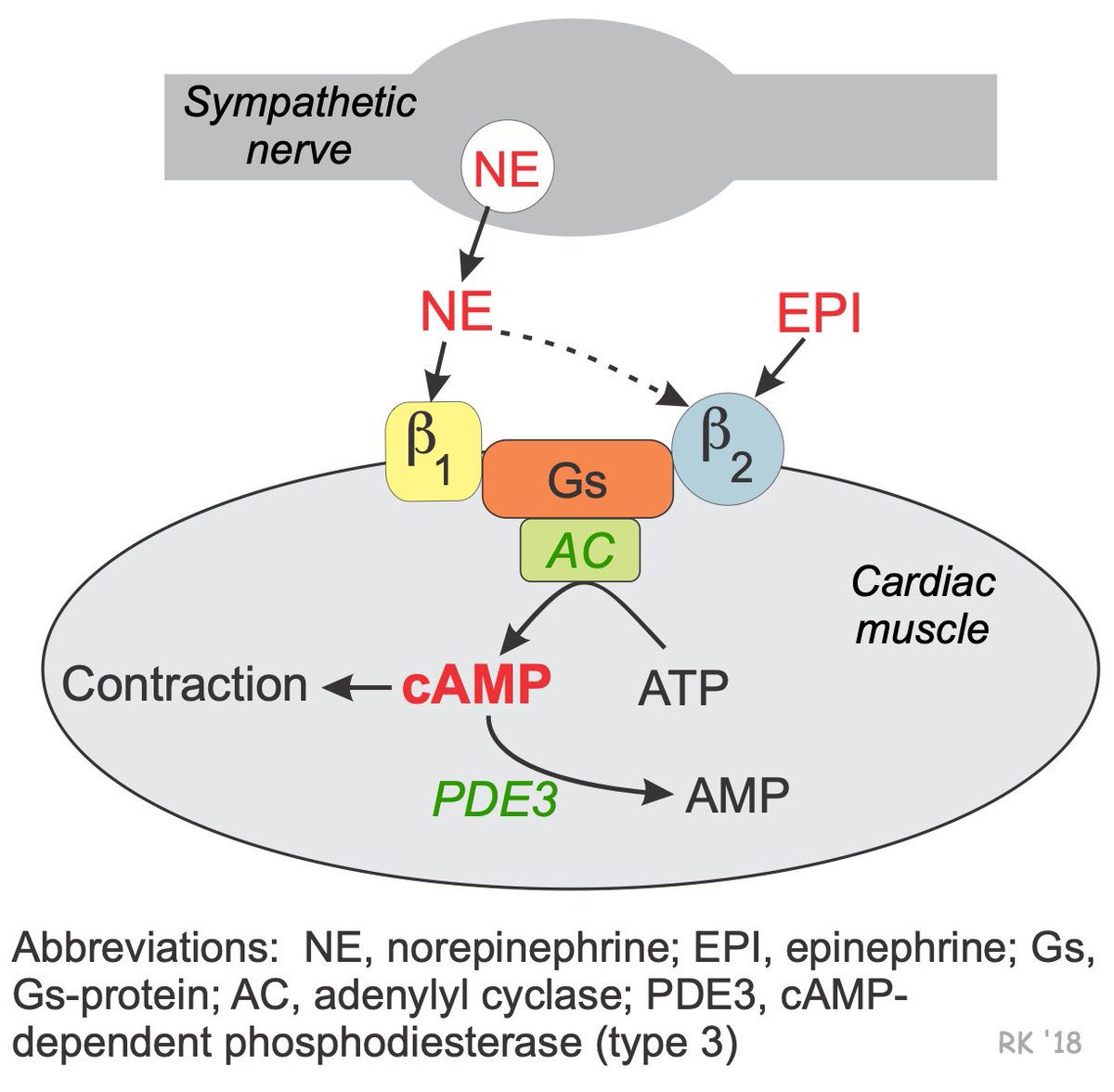
4/ B1 receptors are primarily seen in cardiac tissue. Receptor activation ->  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> AC activity ->
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> AC activity ->  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> cAMP -> cardiac myocytes to squeeze harder (inotropy) and squeeze faster (chronotropy)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> cAMP -> cardiac myocytes to squeeze harder (inotropy) and squeeze faster (chronotropy)  https://abs.twimg.com/emoji/v2/... draggable="false" alt="💖" title="Sparkling heart" aria-label="Emoji: Sparkling heart">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💖" title="Sparkling heart" aria-label="Emoji: Sparkling heart">
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Note that B2 receptors in the heart act by this exact same pathway.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Note that B2 receptors in the heart act by this exact same pathway. https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">
5/ B2 receptors though are not just found in cardiac tissue, they are also found in vascular smooth muscle. They act opposite our a1 friends from above. B1 receptor activation ->  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> AC activity ->
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> AC activity ->  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> cAMP ->
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> cAMP ->  https://abs.twimg.com/emoji/v2/... draggable="false" alt="❌" title="Cross mark" aria-label="Emoji: Cross mark">MLCK -> smooth muscle relaxation or VASODILATION
https://abs.twimg.com/emoji/v2/... draggable="false" alt="❌" title="Cross mark" aria-label="Emoji: Cross mark">MLCK -> smooth muscle relaxation or VASODILATION
6/ Let’s round out our receptor talk by mentioning 2 other receptors
Dopamine (D), located in splanchnic and renal circulation, causes vasodilation when activated.
Vasopressin (V1), also found in the peripheral vasculature, causes vasoconstriction when activated
Dopamine (D), located in splanchnic and renal circulation, causes vasodilation when activated.
Vasopressin (V1), also found in the peripheral vasculature, causes vasoconstriction when activated
7/ We got the receptors down but why are they specifically important in the roles of hemodynamic control?
Well it really comes down to two equations:
MAP=CO x SVR
CO=HR x SV
(MAP=Mean arterial pressure, CO=Cardiac Output, SVR=Systemic Vascular Resistance, SV=stroke volume)
Well it really comes down to two equations:
MAP=CO x SVR
CO=HR x SV
(MAP=Mean arterial pressure, CO=Cardiac Output, SVR=Systemic Vascular Resistance, SV=stroke volume)
8/ We can alter these variables by using those receptors we just used above
Activate a1 -> Vasoconstriction -> https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">SVR
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">SVR
Activate B1 -> https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">HR (chronotropy) and
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">HR (chronotropy) and  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">SV (inotropy) ->
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">SV (inotropy) ->  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">CO
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">CO
Activate B2 -> Vasodilation -> https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Downwards arrow" aria-label="Emoji: Downwards arrow">SVR
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Downwards arrow" aria-label="Emoji: Downwards arrow">SVR
Activate V1 -> Vasoconstriction -> https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">SVR
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">SVR
Activate a1 -> Vasoconstriction ->
Activate B1 ->
Activate B2 -> Vasodilation ->
Activate V1 -> Vasoconstriction ->
9/ Understanding this #physiology we can fit our agents into categories.
1.Inopressors = ↑ inotropy (β1) + vasoconstrict (α1)
2.Inodilators = ↑ inotropy (β1) + vasodilate (β2 or D1)
3.Vasopressors = vasoconstriction (α1 or V1)
Okay time to fill out that #pressorrainbow!
1.Inopressors = ↑ inotropy (β1) + vasoconstrict (α1)
2.Inodilators = ↑ inotropy (β1) + vasodilate (β2 or D1)
3.Vasopressors = vasoconstriction (α1 or V1)
Okay time to fill out that #pressorrainbow!
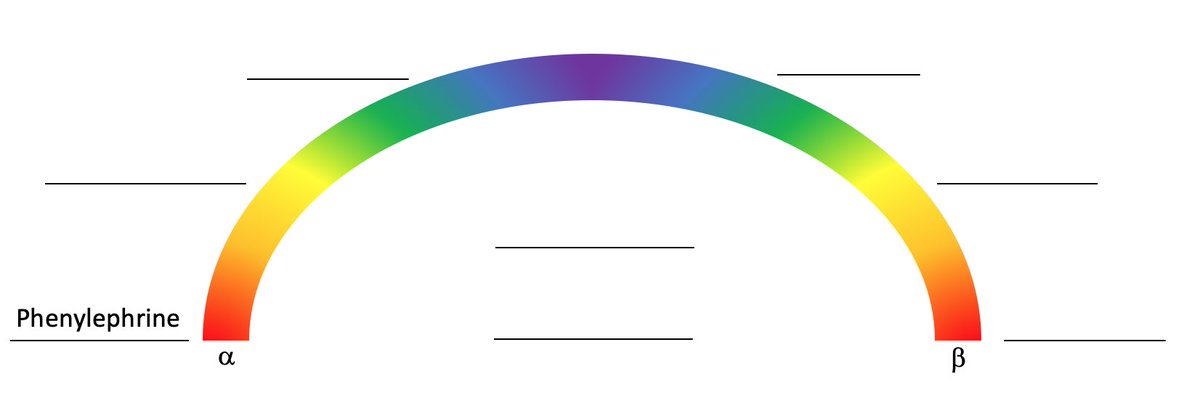
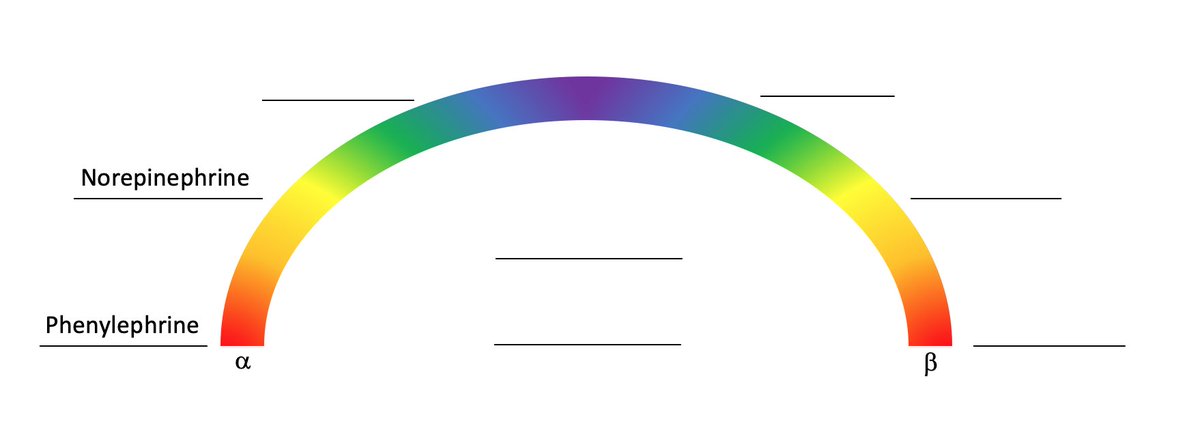
10/ So starting from the far left of the diagram which of these agents have only alpha activity?
11/ Phenylephrine, a vasopressor
R: a1
Uses: refrac hypotension (not 1st line), Tachyarythmia w/ hypotension (produces reflex brady), HOCM ( https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">SVR (afterload) helps stent open the outflow track)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">SVR (afterload) helps stent open the outflow track)
Don’t use: Cardiogenic shock (pure https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> afterload makes it hard for
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> afterload makes it hard for  https://abs.twimg.com/emoji/v2/... draggable="false" alt="💖" title="Sparkling heart" aria-label="Emoji: Sparkling heart"> to pump
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💖" title="Sparkling heart" aria-label="Emoji: Sparkling heart"> to pump
R: a1
Uses: refrac hypotension (not 1st line), Tachyarythmia w/ hypotension (produces reflex brady), HOCM (
Don’t use: Cardiogenic shock (pure
12/ Now moving clockwise on the diagram which of these agents has mainly alpha agonism but also some beta agonism?
13/ Norepinephrine, an inopressor
R: a1>b1 (will increase both SVR and CO)
Use: 1st line in septic shock
Side effects: arrhythmogenic, digital ischemia
R: a1>b1 (will increase both SVR and CO)
Use: 1st line in septic shock
Side effects: arrhythmogenic, digital ischemia
14/ Next is Epinephrine, an inopressor
R: a1>b1>b2 (higher doses)
Use: ACLS, Anaphylaxis, Septic shock (2nd line), symptomatic bradycardia (not first line)
Side effects: arrhythmogenic, cardiac toxicity at prolonged doses
R: a1>b1>b2 (higher doses)
Use: ACLS, Anaphylaxis, Septic shock (2nd line), symptomatic bradycardia (not first line)
Side effects: arrhythmogenic, cardiac toxicity at prolonged doses
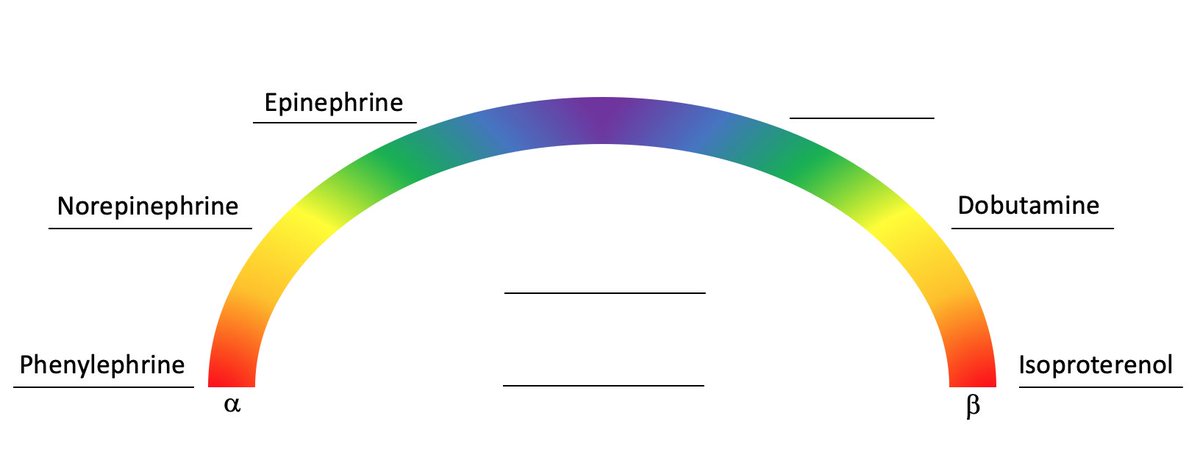
15/ Now that we have completed the left side of the rainbow let’s switch it up and start on the far right and then move counterclockwise. So which of these agents has only beta receptor agonism?
16/ Isoproterenol, an Inodilator
R: B1, B2 ( https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> HR/CO
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> HR/CO  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Downwards arrow" aria-label="Emoji: Downwards arrow"> SVR)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Downwards arrow" aria-label="Emoji: Downwards arrow"> SVR)
Use: Bradycardia, Mg refractory torsades
Side Effects: arrhythmogenic, decreases BP, flushing
R: B1, B2 (
Use: Bradycardia, Mg refractory torsades
Side Effects: arrhythmogenic, decreases BP, flushing
17/ Next is Dobutamine, an inodilator
R: B1>B2 ( https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">CO
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">CO  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Downwards arrow" aria-label="Emoji: Downwards arrow">SVR)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Downwards arrow" aria-label="Emoji: Downwards arrow">SVR)
Use: Cardiogenic Shock
Side Effects: arrhythmogenic, can see tachyphylaxis as prolonged use cause downregulation of B1 receptors
R: B1>B2 (
Use: Cardiogenic Shock
Side Effects: arrhythmogenic, can see tachyphylaxis as prolonged use cause downregulation of B1 receptors
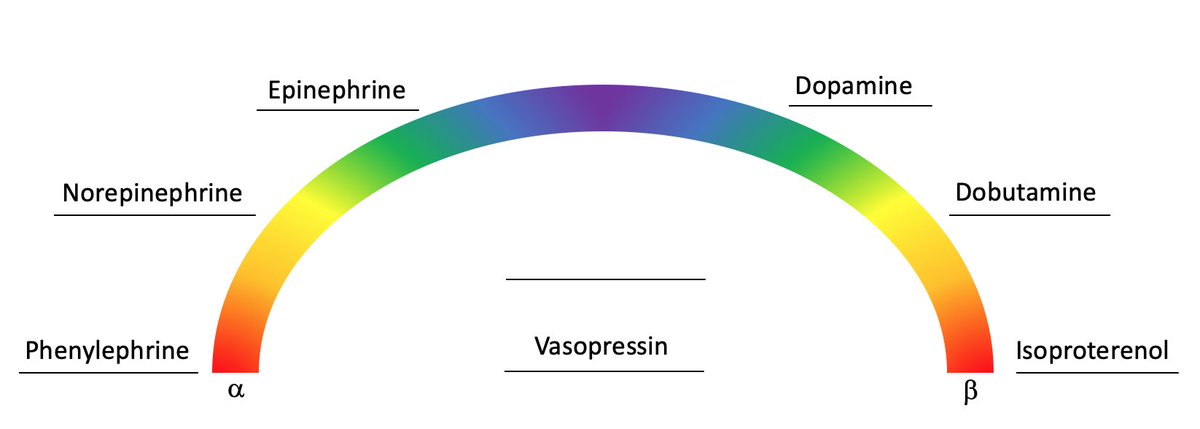
18/ finally, Dopamine, an Inoconstrictor
R: B1>D1>a1 (at low-med doses), a1>B1>D1 (at high doses)
Use: symptomatic bradycardia
SE: Tachyarrhymias (Of note, SOAP-II demonstrated increase risk of adverse events compared to norepi in shock treatment)
https://pubmed.ncbi.nlm.nih.gov/20200382/ ">https://pubmed.ncbi.nlm.nih.gov/20200382/...
R: B1>D1>a1 (at low-med doses), a1>B1>D1 (at high doses)
Use: symptomatic bradycardia
SE: Tachyarrhymias (Of note, SOAP-II demonstrated increase risk of adverse events compared to norepi in shock treatment)
https://pubmed.ncbi.nlm.nih.gov/20200382/ ">https://pubmed.ncbi.nlm.nih.gov/20200382/...
19/ That completes the main rainbow! now you may be wondering what those two blank spots are for? Well, they a for two major agents that don& #39;t fall along the rainbow because they don& #39;t act on alpha and beta receptors. Those being Vasopressin and Milrinone. Let’s discuss briefly.
20/ Vasopressin, a vassopressor (no way https://abs.twimg.com/emoji/v2/... draggable="false" alt="‼️" title="Double exclamation mark" aria-label="Emoji: Double exclamation mark">)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="‼️" title="Double exclamation mark" aria-label="Emoji: Double exclamation mark">)
R: V1 receptors ( https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> SVR)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> SVR)
Use: Adjunct to norepi in septic shock, VAATS trial showed in subgroup of patients with less severe septic shock vaso+norepi provided mortality benefit compared to norepi alone
https://pubmed.ncbi.nlm.nih.gov/18305265/ ">https://pubmed.ncbi.nlm.nih.gov/18305265/...
R: V1 receptors (
Use: Adjunct to norepi in septic shock, VAATS trial showed in subgroup of patients with less severe septic shock vaso+norepi provided mortality benefit compared to norepi alone
https://pubmed.ncbi.nlm.nih.gov/18305265/ ">https://pubmed.ncbi.nlm.nih.gov/18305265/...
21/ Milrinone already uses similar mechanisms we have talked about. It is a a Phosphodiesterase inhibitor (PDE-I).
PDE normally breaks down cAMP, but by inhibiting it we can increase the downstream signaling of cAMP, the same signaling that our Beta receptors normally cause!
PDE normally breaks down cAMP, but by inhibiting it we can increase the downstream signaling of cAMP, the same signaling that our Beta receptors normally cause!
22/ so to complete our rainbow
Milrinone, a inodilator and PDE-I ( https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> CO
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> CO  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Downwards arrow" aria-label="Emoji: Downwards arrow">SVR)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Downwards arrow" aria-label="Emoji: Downwards arrow">SVR)
Use: Cardiogenic shock, some studies ( https://pubmed.ncbi.nlm.nih.gov/9066407/ )">https://pubmed.ncbi.nlm.nih.gov/9066407/&... have demonstrated that milrinone https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Downwards arrow" aria-label="Emoji: Downwards arrow">Pulmonary VR and thus is thought to be beneficial in RH failure
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Downwards arrow" aria-label="Emoji: Downwards arrow">Pulmonary VR and thus is thought to be beneficial in RH failure
SE: arrhythmogenic
Milrinone, a inodilator and PDE-I (
Use: Cardiogenic shock, some studies ( https://pubmed.ncbi.nlm.nih.gov/9066407/ )">https://pubmed.ncbi.nlm.nih.gov/9066407/&... have demonstrated that milrinone
SE: arrhythmogenic
23/ and with that we have completed our pressor rainbow. Remember that the uses of of theses agents we discussed are typical for those specific clinical contexts but not hard and fast rules, you may see many of these being used in combination for certain clinical scenerios.
24/ Importance is not to memorize the indications verbatum, but understand the #physiology of these agents. With that understanding as a primer the knowledge and understanding of when to grab what agent will come. So have fun in those ICU/CCUs and get those knowledge reps in  https://abs.twimg.com/emoji/v2/... draggable="false" alt="💪" title="Flexed biceps" aria-label="Emoji: Flexed biceps">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💪" title="Flexed biceps" aria-label="Emoji: Flexed biceps">
Appreciate any feedback, edits, additions from any and all
@CPSolvers @cardionerds @runthelistpod @rabihmgeha @DxRxEdu @Dr_DanMD @AmitGoyalMD @CarineHamo @heatherkaganmd @thecurbsiders @MedTweetorials @LeivaOrly @WalkerReddM
@CPSolvers @cardionerds @runthelistpod @rabihmgeha @DxRxEdu @Dr_DanMD @AmitGoyalMD @CarineHamo @heatherkaganmd @thecurbsiders @MedTweetorials @LeivaOrly @WalkerReddM

 Read on Twitter
Read on Twitter
 release of free calcium -> smooth muscle contraction or VASOCONSTRICTION https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">https://abs.twimg.com/emoji/v2/... draggable="false" alt="💪" title="Flexed biceps" aria-label="Emoji: Flexed biceps">https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">" title="3/ Lets start with the a1 receptor, specifically those seen in the smooth muscles of our peripheral vasculature. Activation of these receptor -> activation of phopholipase C -> https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> release of free calcium -> smooth muscle contraction or VASOCONSTRICTION https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">https://abs.twimg.com/emoji/v2/... draggable="false" alt="💪" title="Flexed biceps" aria-label="Emoji: Flexed biceps">https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">" class="img-responsive" style="max-width:100%;"/>
release of free calcium -> smooth muscle contraction or VASOCONSTRICTION https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">https://abs.twimg.com/emoji/v2/... draggable="false" alt="💪" title="Flexed biceps" aria-label="Emoji: Flexed biceps">https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">" title="3/ Lets start with the a1 receptor, specifically those seen in the smooth muscles of our peripheral vasculature. Activation of these receptor -> activation of phopholipase C -> https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> release of free calcium -> smooth muscle contraction or VASOCONSTRICTION https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">https://abs.twimg.com/emoji/v2/... draggable="false" alt="💪" title="Flexed biceps" aria-label="Emoji: Flexed biceps">https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">" class="img-responsive" style="max-width:100%;"/>
 AC activity -> https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> cAMP -> cardiac myocytes to squeeze harder (inotropy) and squeeze faster (chronotropy) https://abs.twimg.com/emoji/v2/... draggable="false" alt="💖" title="Sparkling heart" aria-label="Emoji: Sparkling heart">https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Note that B2 receptors in the heart act by this exact same pathway.https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">" title="4/ B1 receptors are primarily seen in cardiac tissue. Receptor activation -> https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> AC activity -> https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> cAMP -> cardiac myocytes to squeeze harder (inotropy) and squeeze faster (chronotropy) https://abs.twimg.com/emoji/v2/... draggable="false" alt="💖" title="Sparkling heart" aria-label="Emoji: Sparkling heart">https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Note that B2 receptors in the heart act by this exact same pathway.https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">" class="img-responsive" style="max-width:100%;"/>
AC activity -> https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> cAMP -> cardiac myocytes to squeeze harder (inotropy) and squeeze faster (chronotropy) https://abs.twimg.com/emoji/v2/... draggable="false" alt="💖" title="Sparkling heart" aria-label="Emoji: Sparkling heart">https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Note that B2 receptors in the heart act by this exact same pathway.https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">" title="4/ B1 receptors are primarily seen in cardiac tissue. Receptor activation -> https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> AC activity -> https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> cAMP -> cardiac myocytes to squeeze harder (inotropy) and squeeze faster (chronotropy) https://abs.twimg.com/emoji/v2/... draggable="false" alt="💖" title="Sparkling heart" aria-label="Emoji: Sparkling heart">https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Note that B2 receptors in the heart act by this exact same pathway.https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">" class="img-responsive" style="max-width:100%;"/>
 AC activity -> https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> cAMP -> https://abs.twimg.com/emoji/v2/... draggable="false" alt="❌" title="Cross mark" aria-label="Emoji: Cross mark">MLCK -> smooth muscle relaxation or VASODILATION" title="5/ B2 receptors though are not just found in cardiac tissue, they are also found in vascular smooth muscle. They act opposite our a1 friends from above. B1 receptor activation -> https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> AC activity -> https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> cAMP -> https://abs.twimg.com/emoji/v2/... draggable="false" alt="❌" title="Cross mark" aria-label="Emoji: Cross mark">MLCK -> smooth muscle relaxation or VASODILATION" class="img-responsive" style="max-width:100%;"/>
AC activity -> https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> cAMP -> https://abs.twimg.com/emoji/v2/... draggable="false" alt="❌" title="Cross mark" aria-label="Emoji: Cross mark">MLCK -> smooth muscle relaxation or VASODILATION" title="5/ B2 receptors though are not just found in cardiac tissue, they are also found in vascular smooth muscle. They act opposite our a1 friends from above. B1 receptor activation -> https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> AC activity -> https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> cAMP -> https://abs.twimg.com/emoji/v2/... draggable="false" alt="❌" title="Cross mark" aria-label="Emoji: Cross mark">MLCK -> smooth muscle relaxation or VASODILATION" class="img-responsive" style="max-width:100%;"/>
 SVR (afterload) helps stent open the outflow track)Don’t use: Cardiogenic shock (pure https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> afterload makes it hard for https://abs.twimg.com/emoji/v2/... draggable="false" alt="💖" title="Sparkling heart" aria-label="Emoji: Sparkling heart"> to pump" title="11/ Phenylephrine, a vasopressor R: a1Uses: refrac hypotension (not 1st line), Tachyarythmia w/ hypotension (produces reflex brady), HOCM (https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">SVR (afterload) helps stent open the outflow track)Don’t use: Cardiogenic shock (pure https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> afterload makes it hard for https://abs.twimg.com/emoji/v2/... draggable="false" alt="💖" title="Sparkling heart" aria-label="Emoji: Sparkling heart"> to pump" class="img-responsive" style="max-width:100%;"/>
SVR (afterload) helps stent open the outflow track)Don’t use: Cardiogenic shock (pure https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> afterload makes it hard for https://abs.twimg.com/emoji/v2/... draggable="false" alt="💖" title="Sparkling heart" aria-label="Emoji: Sparkling heart"> to pump" title="11/ Phenylephrine, a vasopressor R: a1Uses: refrac hypotension (not 1st line), Tachyarythmia w/ hypotension (produces reflex brady), HOCM (https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">SVR (afterload) helps stent open the outflow track)Don’t use: Cardiogenic shock (pure https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> afterload makes it hard for https://abs.twimg.com/emoji/v2/... draggable="false" alt="💖" title="Sparkling heart" aria-label="Emoji: Sparkling heart"> to pump" class="img-responsive" style="max-width:100%;"/>

 HR/CO https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Downwards arrow" aria-label="Emoji: Downwards arrow"> SVR)Use: Bradycardia, Mg refractory torsadesSide Effects: arrhythmogenic, decreases BP, flushing" title="16/ Isoproterenol, an Inodilator R: B1, B2 (https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> HR/CO https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Downwards arrow" aria-label="Emoji: Downwards arrow"> SVR)Use: Bradycardia, Mg refractory torsadesSide Effects: arrhythmogenic, decreases BP, flushing" class="img-responsive" style="max-width:100%;"/>
HR/CO https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Downwards arrow" aria-label="Emoji: Downwards arrow"> SVR)Use: Bradycardia, Mg refractory torsadesSide Effects: arrhythmogenic, decreases BP, flushing" title="16/ Isoproterenol, an Inodilator R: B1, B2 (https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> HR/CO https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Downwards arrow" aria-label="Emoji: Downwards arrow"> SVR)Use: Bradycardia, Mg refractory torsadesSide Effects: arrhythmogenic, decreases BP, flushing" class="img-responsive" style="max-width:100%;"/>
 CO https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Downwards arrow" aria-label="Emoji: Downwards arrow">SVR)Use: Cardiogenic Shock Side Effects: arrhythmogenic, can see tachyphylaxis as prolonged use cause downregulation of B1 receptors" title="17/ Next is Dobutamine, an inodilatorR: B1>B2 (https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">CO https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Downwards arrow" aria-label="Emoji: Downwards arrow">SVR)Use: Cardiogenic Shock Side Effects: arrhythmogenic, can see tachyphylaxis as prolonged use cause downregulation of B1 receptors" class="img-responsive" style="max-width:100%;"/>
CO https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Downwards arrow" aria-label="Emoji: Downwards arrow">SVR)Use: Cardiogenic Shock Side Effects: arrhythmogenic, can see tachyphylaxis as prolonged use cause downregulation of B1 receptors" title="17/ Next is Dobutamine, an inodilatorR: B1>B2 (https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">CO https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Downwards arrow" aria-label="Emoji: Downwards arrow">SVR)Use: Cardiogenic Shock Side Effects: arrhythmogenic, can see tachyphylaxis as prolonged use cause downregulation of B1 receptors" class="img-responsive" style="max-width:100%;"/>

 ) R: V1 receptors (https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> SVR)Use: Adjunct to norepi in septic shock, VAATS trial showed in subgroup of patients with less severe septic shock vaso+norepi provided mortality benefit compared to norepi alone https://pubmed.ncbi.nlm.nih.gov/18305265/..." title="20/ Vasopressin, a vassopressor (no wayhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="‼️" title="Double exclamation mark" aria-label="Emoji: Double exclamation mark">) R: V1 receptors (https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> SVR)Use: Adjunct to norepi in septic shock, VAATS trial showed in subgroup of patients with less severe septic shock vaso+norepi provided mortality benefit compared to norepi alone https://pubmed.ncbi.nlm.nih.gov/18305265/..." class="img-responsive" style="max-width:100%;"/>
) R: V1 receptors (https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> SVR)Use: Adjunct to norepi in septic shock, VAATS trial showed in subgroup of patients with less severe septic shock vaso+norepi provided mortality benefit compared to norepi alone https://pubmed.ncbi.nlm.nih.gov/18305265/..." title="20/ Vasopressin, a vassopressor (no wayhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="‼️" title="Double exclamation mark" aria-label="Emoji: Double exclamation mark">) R: V1 receptors (https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> SVR)Use: Adjunct to norepi in septic shock, VAATS trial showed in subgroup of patients with less severe septic shock vaso+norepi provided mortality benefit compared to norepi alone https://pubmed.ncbi.nlm.nih.gov/18305265/..." class="img-responsive" style="max-width:100%;"/>
 CO https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Downwards arrow" aria-label="Emoji: Downwards arrow">SVR)Use: Cardiogenic shock, some studies ( https://pubmed.ncbi.nlm.nih.gov/9066407/&... have demonstrated that milrinone https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Downwards arrow" aria-label="Emoji: Downwards arrow">Pulmonary VR and thus is thought to be beneficial in RH failureSE: arrhythmogenic" title="22/ so to complete our rainbowMilrinone, a inodilator and PDE-I (https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> CO https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Downwards arrow" aria-label="Emoji: Downwards arrow">SVR)Use: Cardiogenic shock, some studies ( https://pubmed.ncbi.nlm.nih.gov/9066407/&... have demonstrated that milrinone https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Downwards arrow" aria-label="Emoji: Downwards arrow">Pulmonary VR and thus is thought to be beneficial in RH failureSE: arrhythmogenic" class="img-responsive" style="max-width:100%;"/>
CO https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Downwards arrow" aria-label="Emoji: Downwards arrow">SVR)Use: Cardiogenic shock, some studies ( https://pubmed.ncbi.nlm.nih.gov/9066407/&... have demonstrated that milrinone https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Downwards arrow" aria-label="Emoji: Downwards arrow">Pulmonary VR and thus is thought to be beneficial in RH failureSE: arrhythmogenic" title="22/ so to complete our rainbowMilrinone, a inodilator and PDE-I (https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> CO https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Downwards arrow" aria-label="Emoji: Downwards arrow">SVR)Use: Cardiogenic shock, some studies ( https://pubmed.ncbi.nlm.nih.gov/9066407/&... have demonstrated that milrinone https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Downwards arrow" aria-label="Emoji: Downwards arrow">Pulmonary VR and thus is thought to be beneficial in RH failureSE: arrhythmogenic" class="img-responsive" style="max-width:100%;"/>



