So, here’s some genuine questions to all you awesome critical care guys leading the fight against #COVID19. How frequently do you rely on ABGs for guiding management? #thread
It’s been over 2 months since our institute has been converted into a dedicated #COVID19 care centre, one of the largest in the state of Maharashtra. Would like to share a couple of observations from my limited experience with #COVID19 leading to these questions
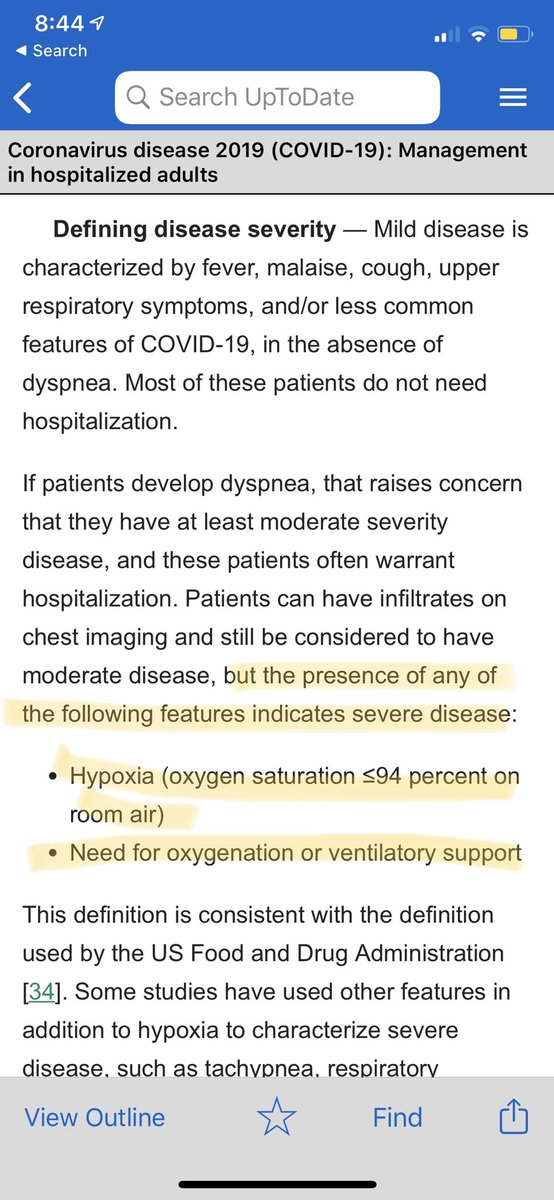
Frankly hypoxic patients with bad CXRs do quite well on increasing FiO2s on NRBM with reservoir. Respiratory fatigue also doesn’t set in so easily. The so called “happy hypoxia” appears real.
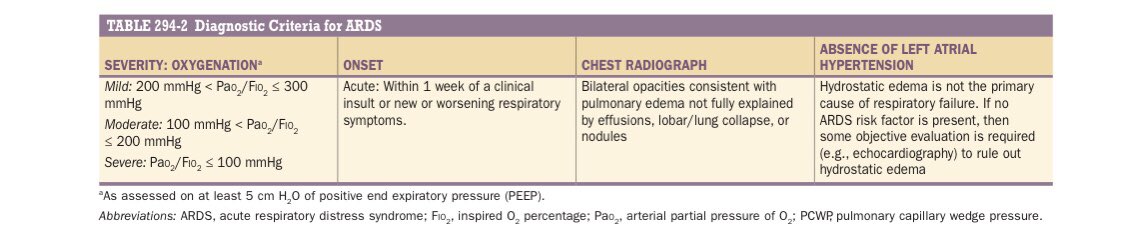
These patients appear to be maintaining Sats although low P/F ratios. However they do not deteriorate rapidly. And all classify as Severe COVID. And some frequently have P/F ratios of <100 but continue to sustain on NRBM with reservoir
There are of course certain subsets of patients who also rapidly worsen and continue to do so, despite early invasive machanical ventilation. And this would probably relate to ARDS subtypes, discussed in this fantastic thread by @robertpdickson https://twitter.com/robertpdickson/status/1254117056326389763">https://twitter.com/robertpdi...
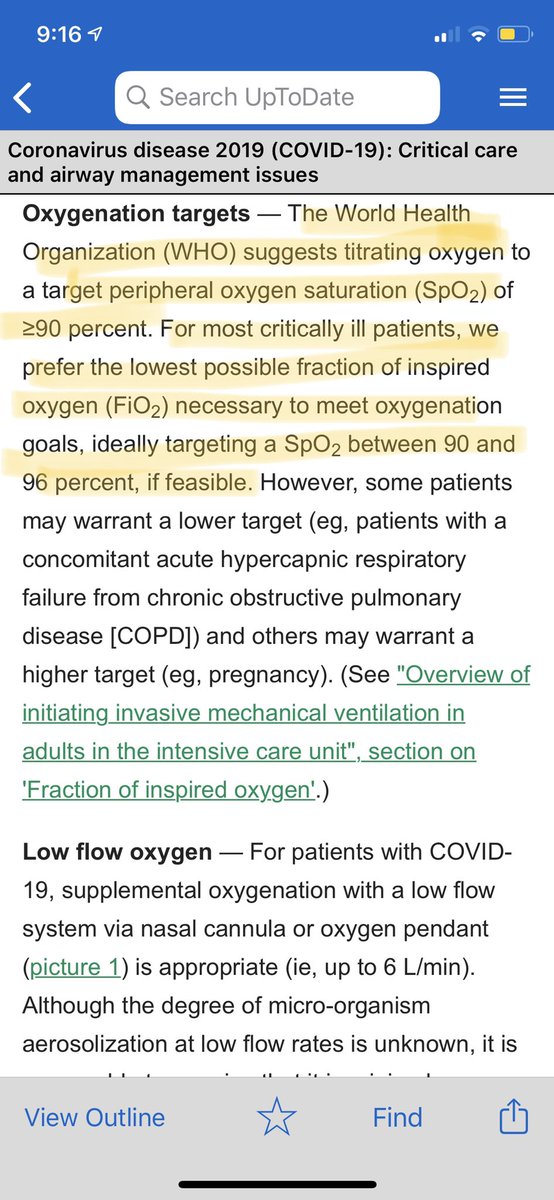
So, now the question is - what role does the P/F ratio hold in patients who are on oxygen only with high FiO2 and not on any form of mechanical ventilation? How useful is it do guide management and can the SpO2/ FiO2 ratio not be used instead as a non invasive substitute?
This study shows the usefulness of SpO2/ FiO2 ratio and that a S/F ratio of <235 correlated with a P/F ratio of <200 with 85% sensitivity and specificity
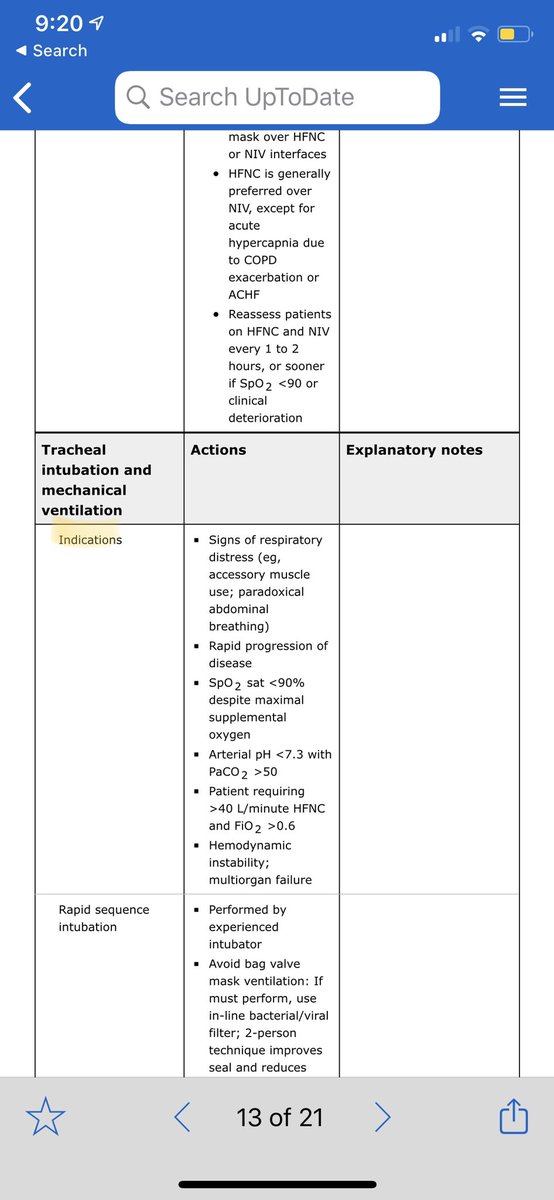
A formal ABG ofcourse additionally allows for evaluation of acid base status and PCO2 levels. Rising PCO2 levels could indicate early respiratory fatigue in the face of maintained SpO2 levels with high FiO2s and benefit from NIV. Also ABG parameters guide need for intubation
However one can consider doing ABGs with worsening clinical status, increasing oxygen requirements (this is with regards to patients not on mechanical ventilation). For patients who continue to maintain saturation in the recommended range - can we rely on S/F ratio instead?
Final questions -
ABGs in #COVID19 patients - when and how often?
Do P/F ratios hold any value outside the realm of mechanical ventilation to guide management?
S/F ratio a good non invasive monitoring measure for those on high FiO2s but not mechanical ventilation?
ABGs in #COVID19 patients - when and how often?
Do P/F ratios hold any value outside the realm of mechanical ventilation to guide management?
S/F ratio a good non invasive monitoring measure for those on high FiO2s but not mechanical ventilation?
All this on the background that no specific treatment for #COVID19 has shown a mortality benefit.
Note: The questions are genuine doubts. As a Cardiology fellow currently working with #COVID19 looking forward to advice and meaningful discussion.

 Read on Twitter
Read on Twitter