Good morning! Based on my latest poll, I’m going to start off this (short!) week with a non COVID heme #tweetorial.
It turns out there are other conditions still affecting patients!
4yo previously healthy https://abs.twimg.com/emoji/v2/... draggable="false" alt="👦" title="Boy" aria-label="Emoji: Boy"> presents with dark urine and fever.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👦" title="Boy" aria-label="Emoji: Boy"> presents with dark urine and fever.
1/n
It turns out there are other conditions still affecting patients!
4yo previously healthy
1/n
Initial labs remarkable for hemoglobin of 6.6, LDH 2260, and bilirubin of 6.8 (largely indirect).
DAT is negative for IgG and 1+ for C3.
DAT (direct antiglobulin test or direct Coombs) detects in vivo sensitization of RBCs.
2/n
DAT is negative for IgG and 1+ for C3.
DAT (direct antiglobulin test or direct Coombs) detects in vivo sensitization of RBCs.
2/n
RBCs are washed to remove unbound antibodies. Anti-IgG (or complement) reagent is added. If antibody is present on RBCs—> agglutination!
Antibodies are then eluted off to determine specificity.
3/n
Antibodies are then eluted off to determine specificity.
3/n
IgG antibodies (seen in warm AIHA) bind preferentially at 37C, are removed primarily by the spleen, and cause extravascular hemolysis.
IgM antivirals bind optimally at 0-4C but can fix complement at normal body temperatures.
But, some IgG are cold reactive!
4/n
IgM antivirals bind optimally at 0-4C but can fix complement at normal body temperatures.
But, some IgG are cold reactive!
4/n
Paroxysmal cold hemoglobinuria (PCH) was first described clinically in 1872!
These two chaps (Donath and Landsteiner) discovered the antibody (which would later be named for them) in 1904.
5/n
These two chaps (Donath and Landsteiner) discovered the antibody (which would later be named for them) in 1904.
5/n
The DL antibody is a polyclonal IgG with P antigen specificity.
Side note: this is also a binding site for parvovirus which causes Fifth disease in kids.
It got this name as it just happened to be the 5th on a list of childhood diseases with rash https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤷♀️" title="Woman shrugging" aria-label="Emoji: Woman shrugging">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤷♀️" title="Woman shrugging" aria-label="Emoji: Woman shrugging">
6/n
Side note: this is also a binding site for parvovirus which causes Fifth disease in kids.
It got this name as it just happened to be the 5th on a list of childhood diseases with rash
6/n
DL causes biphasic hemolysis.
IgG binds P antigen and fixes complement at cold temperatures.
When RBCs are heated (as travel from periphery to core) to 37C the membrane attack complex is activated and lyses RBCs.
7/n
IgG binds P antigen and fixes complement at cold temperatures.
When RBCs are heated (as travel from periphery to core) to 37C the membrane attack complex is activated and lyses RBCs.
7/n
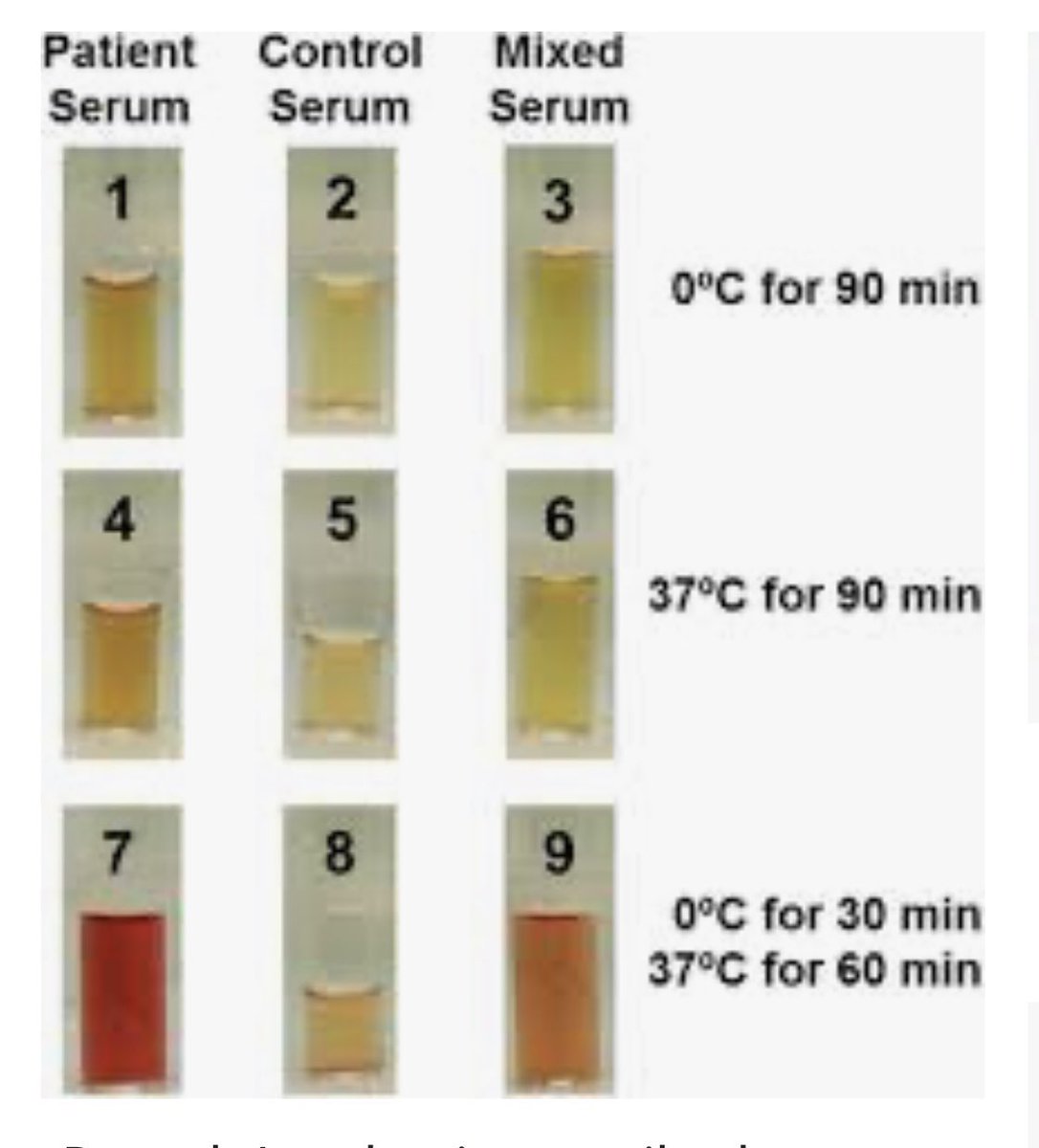
To test for DL, 3 specimens are used.
1. Patients serum
2. Donor serum
3. Mixture
P+ RBCs are added to each
Samples are kept at 4C, then heated to 37C and visualized for hemolysis.
Negative controls are kept at 4C and 37C throughout.
8/n
1. Patients serum
2. Donor serum
3. Mixture
P+ RBCs are added to each
Samples are kept at 4C, then heated to 37C and visualized for hemolysis.
Negative controls are kept at 4C and 37C throughout.
8/n
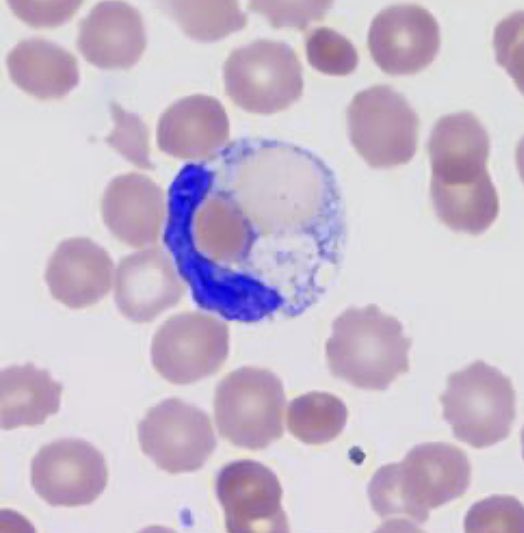
In addition to a positive antibody test, peripheral blood smear may reveal erythrophagocytosis (try saying that three times fast!)
Although this is seen with monocytes in other entities, neutrophil mediated erythrophagocytosis is rarely seen outside of PCH.
Pretty, no?
9/n
Although this is seen with monocytes in other entities, neutrophil mediated erythrophagocytosis is rarely seen outside of PCH.
Pretty, no?
9/n
Patients present with fever, chills, pain (abdominal, back, legs) as well as hemoglobinuria following cold exposure.
As the hemolysis is intravascular, free hemoglobin is released into plasma and filtered by the kidneys. Hence, hemoglobinuria!
10/n
As the hemolysis is intravascular, free hemoglobin is released into plasma and filtered by the kidneys. Hence, hemoglobinuria!
10/n
Anemia can be severe and even fatal.
History of cold exposure precipitating symptoms is helpful if elicited but given severity, don’t get any crazy ideas about using this to test/confirm.
11/n
History of cold exposure precipitating symptoms is helpful if elicited but given severity, don’t get any crazy ideas about using this to test/confirm.
11/n
Historically syphilis was the most common cause but now it mostly occurs in post viral kids.
Also seen in autoimmune disorders and malignancy.
How it develops isn’t entirely understood but molecular mimicry (infectious antigen shares similarity to P) is hypothesized.
12/n
Also seen in autoimmune disorders and malignancy.
How it develops isn’t entirely understood but molecular mimicry (infectious antigen shares similarity to P) is hypothesized.
12/n
In kids, PCH is acute, transient and less likely to be related to cold temps. Adults can have more chronic, relapsing courses.
Treatment is usually supportive with cold avoidance, fluids, and transfusion. Folate supplementation can help support effective erythropoiesis.
13/n
Treatment is usually supportive with cold avoidance, fluids, and transfusion. Folate supplementation can help support effective erythropoiesis.
13/n
PCH is not only fascinating from a pathophysiology perspective.
It also illustrates one of the many reasons that I love pediatrics: the resilience and strength of kids.
14/fin
It also illustrates one of the many reasons that I love pediatrics: the resilience and strength of kids.
14/fin

 Read on Twitter
Read on Twitter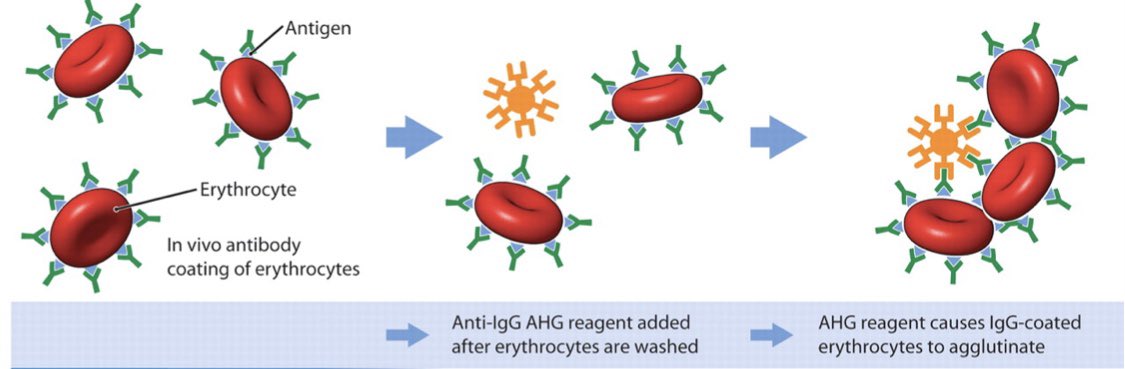
 6/n" title="The DL antibody is a polyclonal IgG with P antigen specificity. Side note: this is also a binding site for parvovirus which causes Fifth disease in kids. It got this name as it just happened to be the 5th on a list of childhood diseases with rash https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤷♀️" title="Woman shrugging" aria-label="Emoji: Woman shrugging">6/n" class="img-responsive" style="max-width:100%;"/>
6/n" title="The DL antibody is a polyclonal IgG with P antigen specificity. Side note: this is also a binding site for parvovirus which causes Fifth disease in kids. It got this name as it just happened to be the 5th on a list of childhood diseases with rash https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤷♀️" title="Woman shrugging" aria-label="Emoji: Woman shrugging">6/n" class="img-responsive" style="max-width:100%;"/>