[thread] The paradox of treating ARDS is this: because we don& #39;t have a drug to reverse lung injury, we provide supportive care with two therapies - oxygen and mechanical ventilation - that can both cause ARDS.
Like treating cancer w/ carcinogens. Or infections w/ pathogens.
1/n
Like treating cancer w/ carcinogens. Or infections w/ pathogens.
1/n
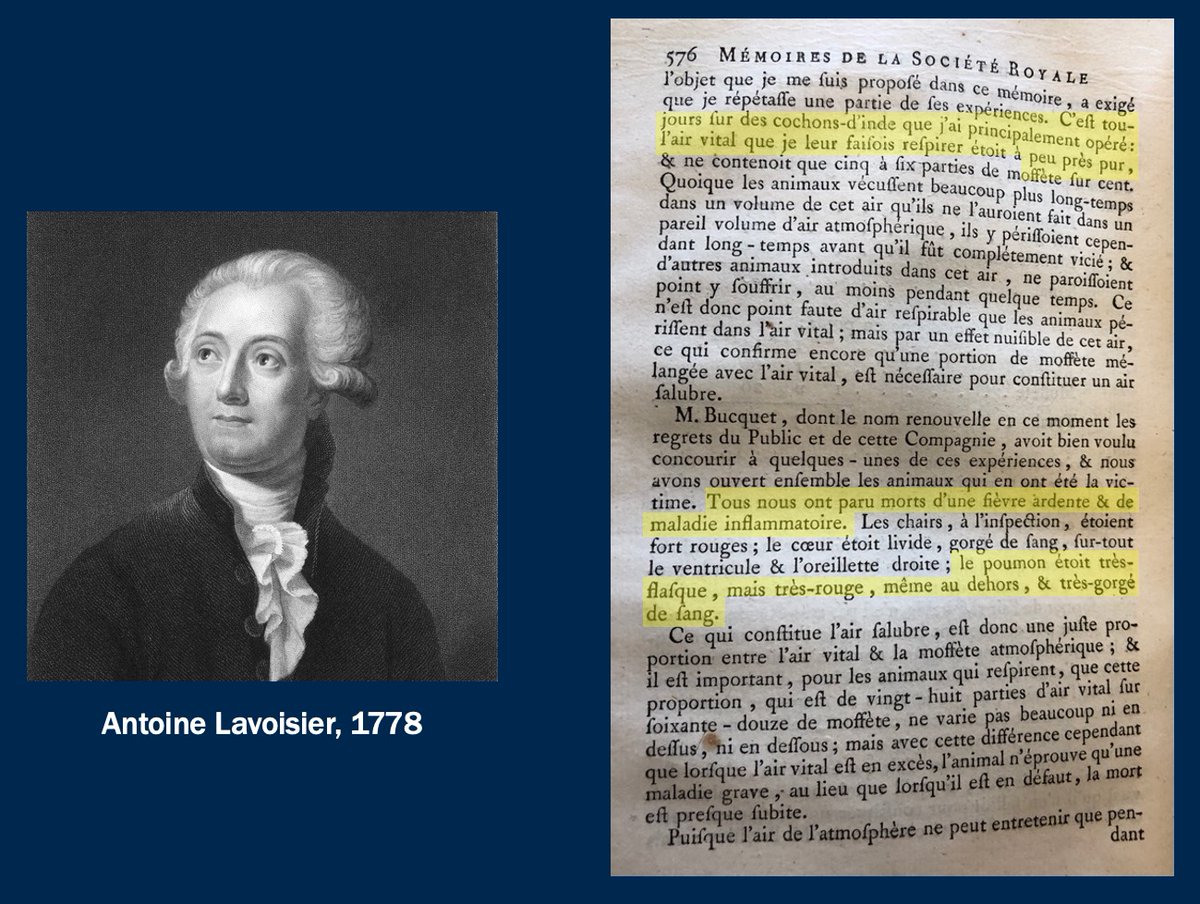
We& #39;ve known that oxygen causes lung injury for 250 years. Lavoisier stuck guinea pigs in "l& #39;air vital" and watched them die from "une fièvre ardente" and a "maladie inflammatoire." Their lungs were flacid, red, and engorged with blood. Their right ventricles were dilated.
2/n
2/n
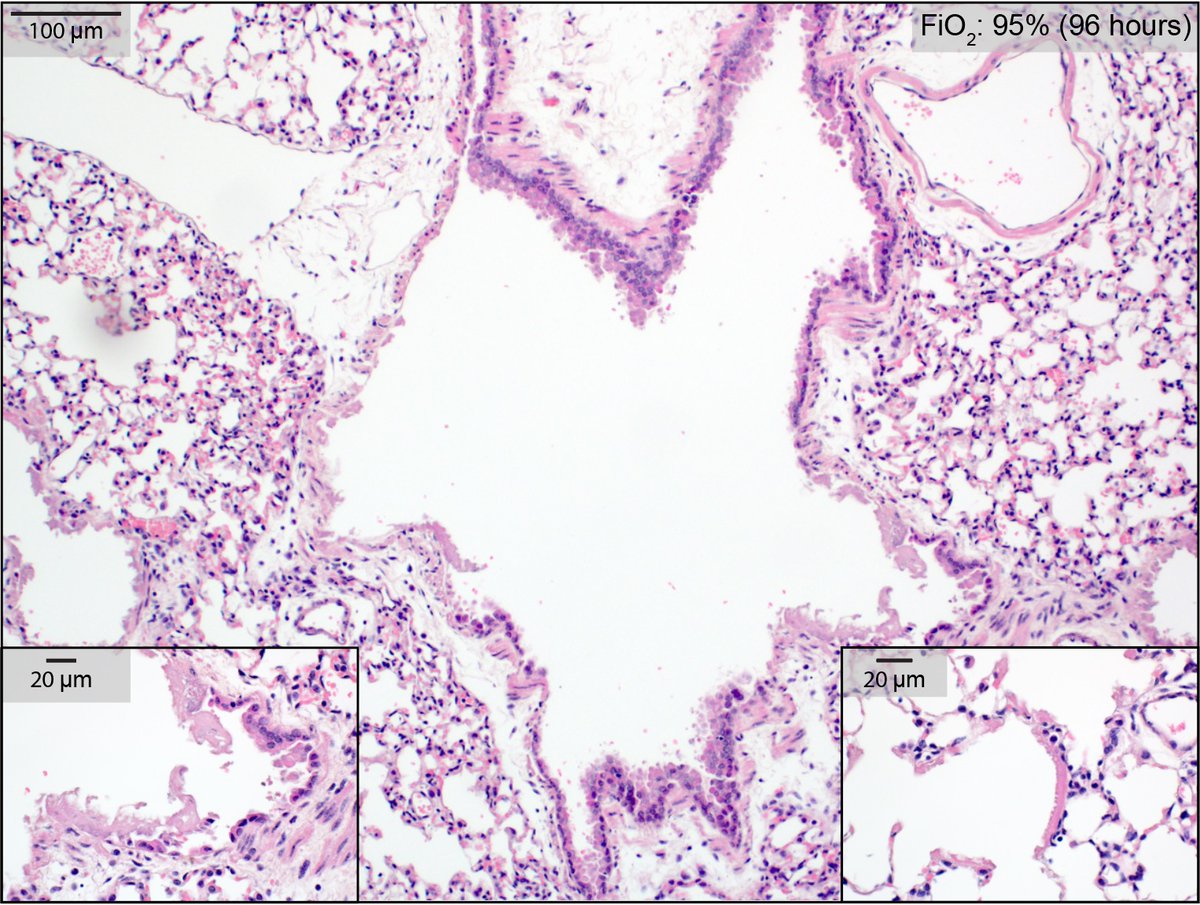
He was describing ARDS (w/ cor pulmonale), 200 years before we named it. If he& #39;d had microscopy, he& #39;d have seen epithelial necrosis, hyaline membranes: diffuse alveolar damage. Same injury pattern that COVID causes. (Image from my lab: healthy mouse, 95% FiO2 for 4 days.)
3/n
3/n
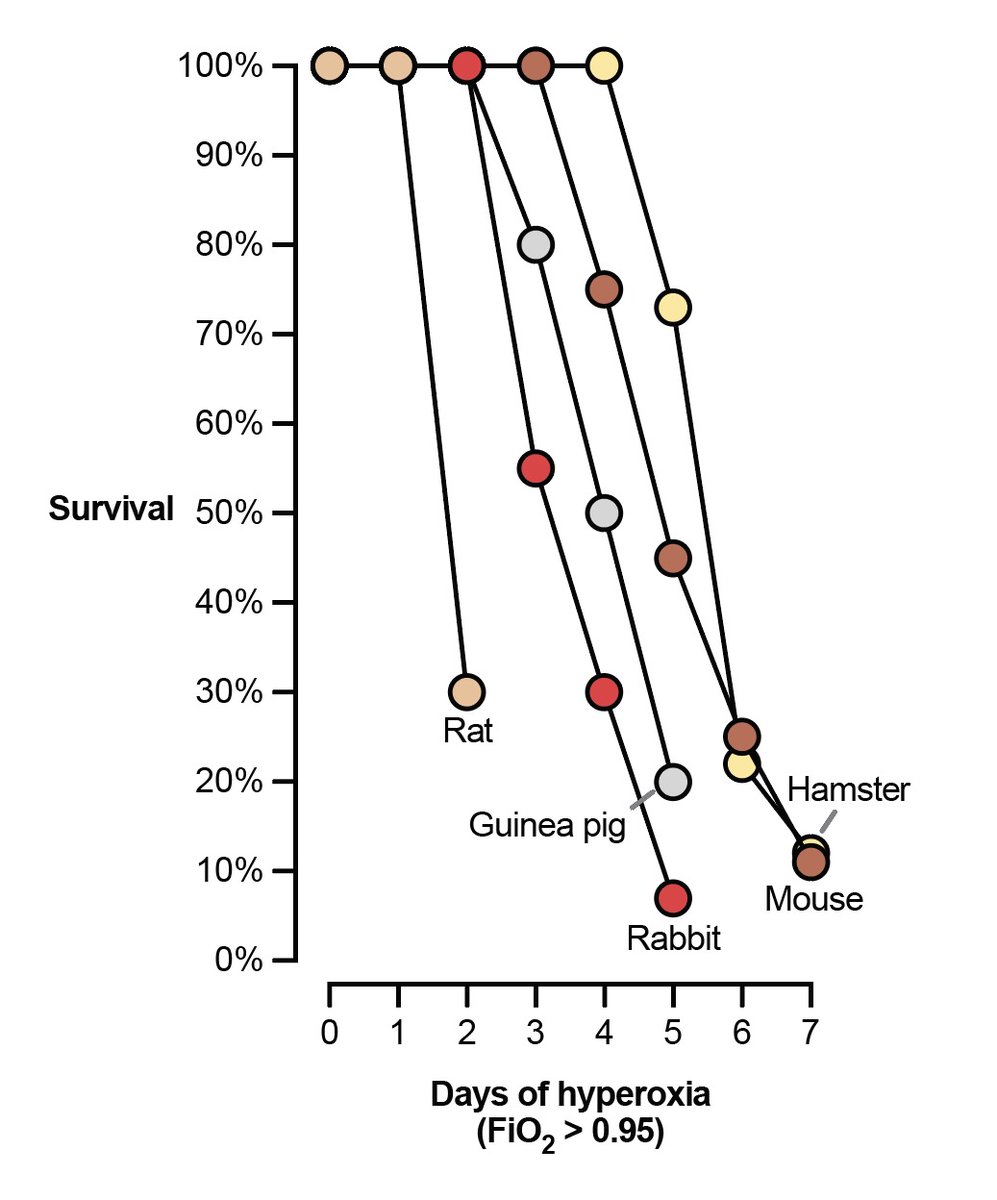
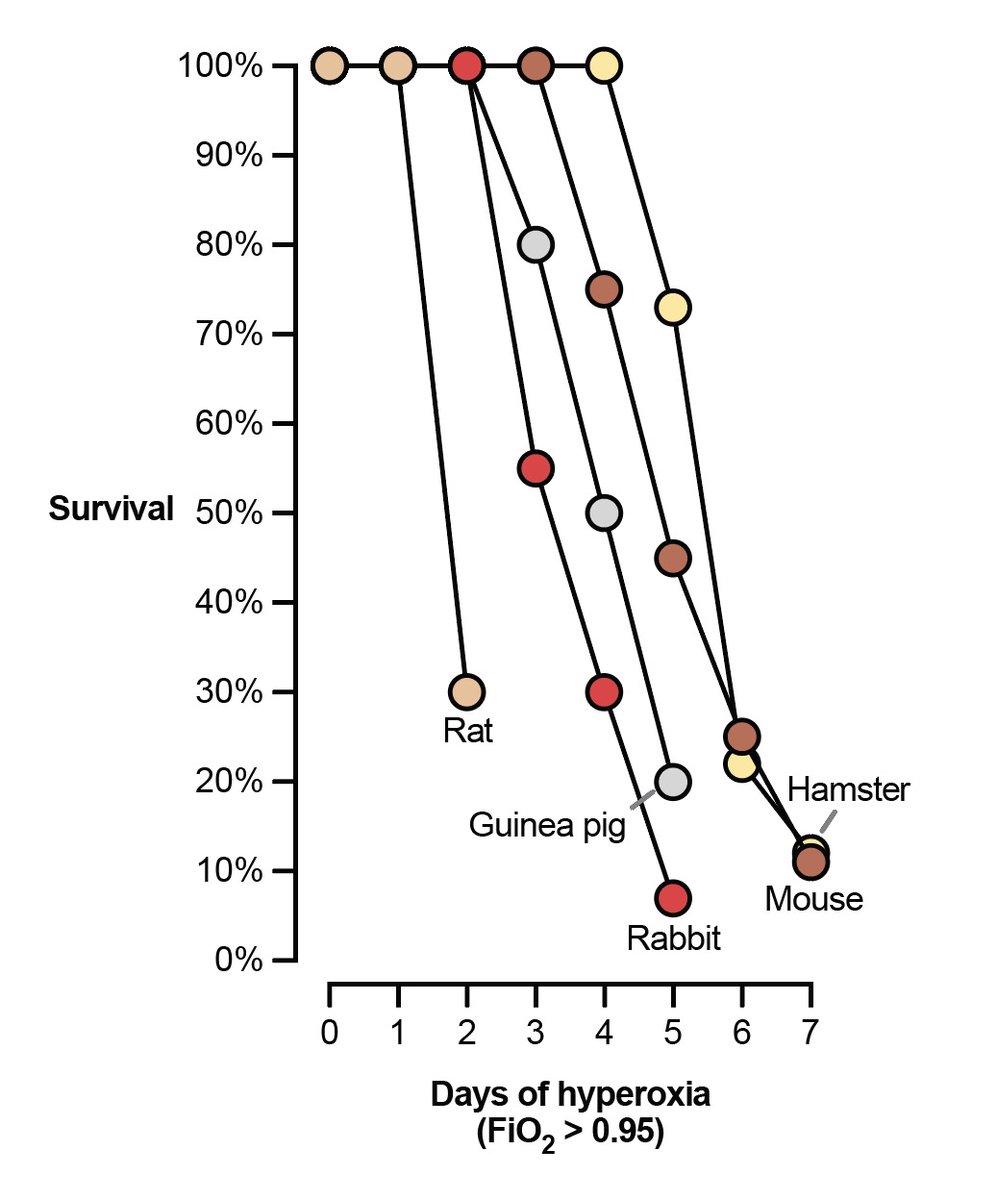
This observation (O2 --> ARDS) is universal among animals with lungs. If you give mammal pure oxygen to breathe, it& #39;ll die within a week with severe lung injury.
(Figure adapted from https://www.ncbi.nlm.nih.gov/pubmed/730565 )
4/n">https://www.ncbi.nlm.nih.gov/pubmed/73...
(Figure adapted from https://www.ncbi.nlm.nih.gov/pubmed/730565 )
4/n">https://www.ncbi.nlm.nih.gov/pubmed/73...
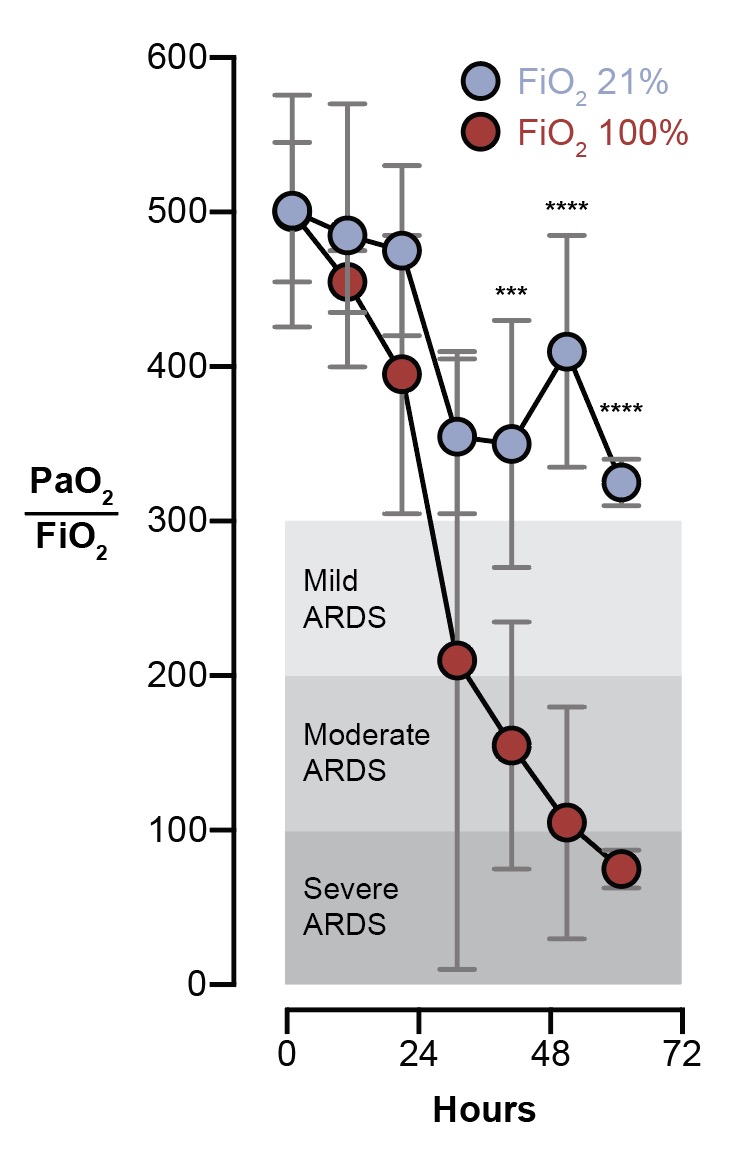
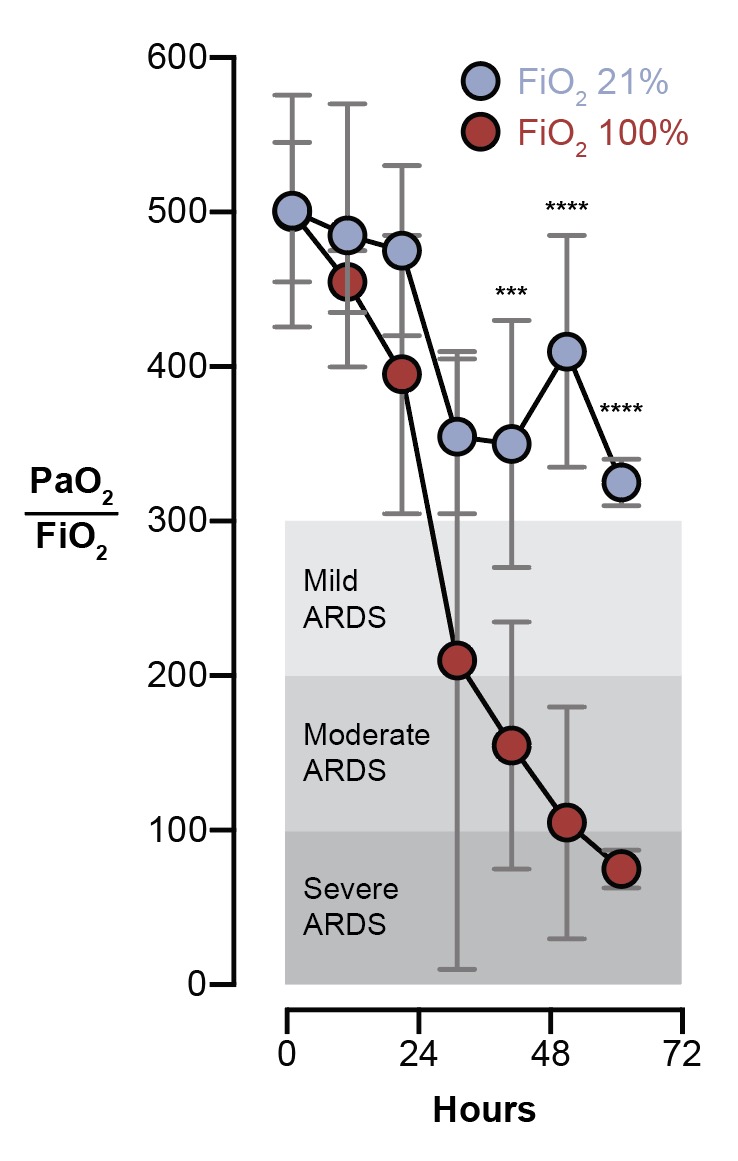
Humans are not an exception. If you take a group of brain dead patients and give half of them 100% FiO2, they& #39;ll have severe hypoxic respiratory failure within 3 days. The control group (21% FiO2) will not.
(Figure adapted from https://www.ncbi.nlm.nih.gov/pubmed/4921729 )
5/n">https://www.ncbi.nlm.nih.gov/pubmed/49...
(Figure adapted from https://www.ncbi.nlm.nih.gov/pubmed/4921729 )
5/n">https://www.ncbi.nlm.nih.gov/pubmed/49...
For all the bad press that mechanical ventilation has gotten recently, I worry what will happen when the word gets out about oxygen. It& #39;s pretty toxic for lungs!
6/n
6/n
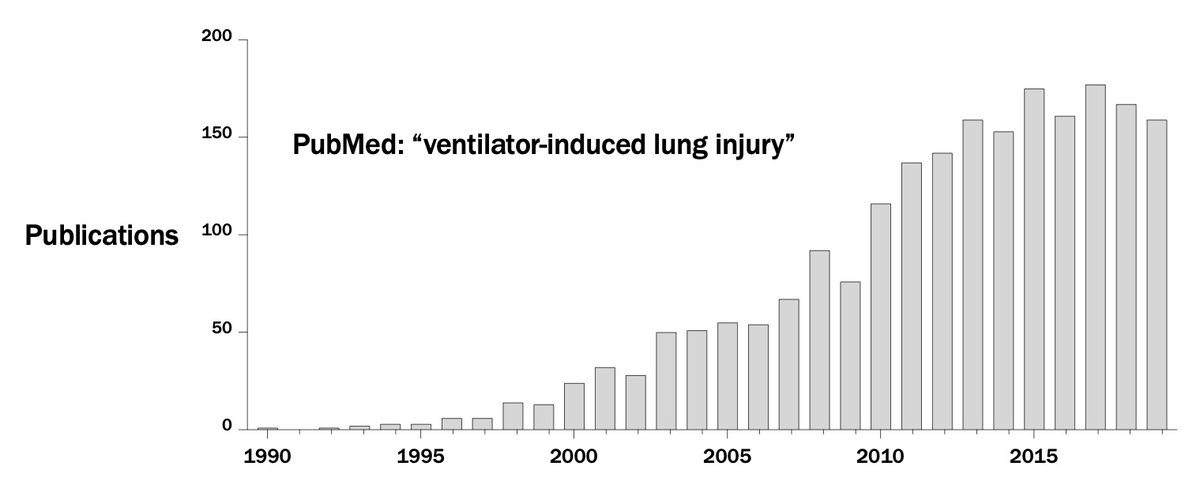
And while you might get the impression that "some doctors" and Elon Musk have recently discovered the danger of ventilators, this has been a topic of intense study for 30 years. It is unambiguous that mechanical ventilation can cause... ARDS.
7/n
7/n
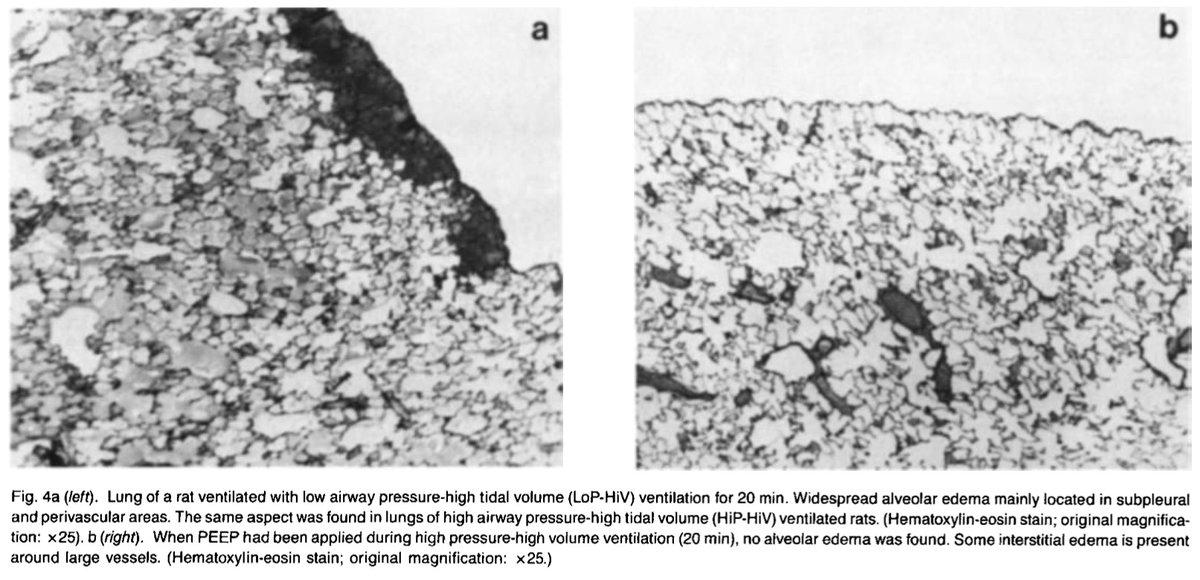
If you ventilate healthy animals with high pressures (w/ a vent) or high volumes (w/ an iron lung), you cause... diffuse alveolar damage. Again, the same pattern of injury we see in COVID lungs. Ventilators can cause ARDS.
(Image from https://www.ncbi.nlm.nih.gov/pubmed/3057957 ...">https://www.ncbi.nlm.nih.gov/pubmed/30... 1988!)
8/n
(Image from https://www.ncbi.nlm.nih.gov/pubmed/3057957 ...">https://www.ncbi.nlm.nih.gov/pubmed/30... 1988!)
8/n
So this is our challenge: in a patient with severe lung injury causing hypoxemia, our only options are 1) give them oxygen, which can cause ARDS; 2) mechanically ventilate them, which can cause ARDS; or 3) tolerate hypoxemia. That& #39;s a tough choice! We don& #39;t make it lightly.
9/n
9/n
Our imperfect solution is to use a combination of all three to minimize harm from any one of them. Tolerate lower-than-normal-but-not-life-threatening blood oxygen levels. Give just enough O2 and mechanical ventilation to support the patient without worsening the problem.
10/n
10/n
All of our effective therapies are basically harm reduction strategies. PEEP is an FiO2-sparing intervention. Lung-protective ventilation, neuromuscular blockade, and proning are all meant to reduce the violence we do to lungs with the ventilator.
11/n
11/n
Think of O2 and the ventilator like you think of a scalpel. It& #39;s a murder weapon, but if used sparingly and judiciously, it can save lives.
12/n
12/n
But UNLIKE with scalpels, we can& #39;t immediately tell that we& #39;re hurting patients with O2 and vents. My mice in 95% oxygen look great! You& #39;d never know by looking at them that they are 3-4 days away from severe ARDS.
13/n
13/n
Likewise with vents. Patients might look _better_ (in terms of oxygenation, comfort, etc.) with settings that worsen lung injury (e.g. the control arm in ARMA that didn& #39;t receive LPV).
You just can& #39;t tell by looking at a patient if your intervention is hurting them.
14/n
You just can& #39;t tell by looking at a patient if your intervention is hurting them.
14/n
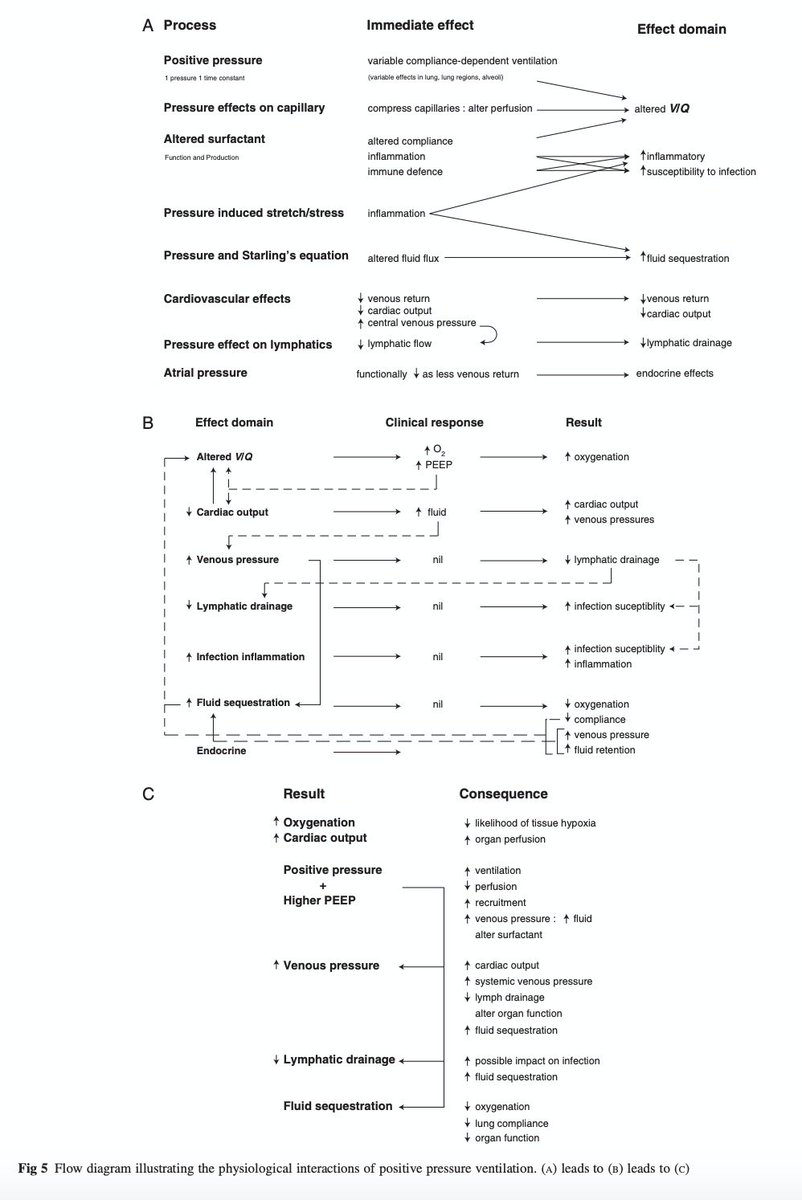
Every change we make on the vent has a cascade of effects across organ systems: not merely (merely!) pulmonary and cardiac, but also lymphatics, inflammation & coagulation, renal...
We should be humble when predicting effects of our interventions.
https://academic.oup.com/bja/article/101/4/446/290624
15/n">https://academic.oup.com/bja/artic...
We should be humble when predicting effects of our interventions.
https://academic.oup.com/bja/article/101/4/446/290624
15/n">https://academic.oup.com/bja/artic...
So when someone suggests we & #39;keep COVID patients off vents,& #39; I need to know the opportunity costs.
Are you ok with very high doses of O2 for days? As in, literally my animal model of ARDS? Are you sure that& #39;s better for patients than lower FiO2 with a modest PEEP setting?
16/n
Are you ok with very high doses of O2 for days? As in, literally my animal model of ARDS? Are you sure that& #39;s better for patients than lower FiO2 with a modest PEEP setting?
16/n
Embracing the theme of humility: I don& #39;t profess to know the optimal balance of harms caused by hypoxemia, O2 toxicity, and VILI.
But I know that as a field, we& #39;ve made steady, incremental progress in improving ARDS outcomes in recent decades. We& #39;re getting better at it.
17/n
But I know that as a field, we& #39;ve made steady, incremental progress in improving ARDS outcomes in recent decades. We& #39;re getting better at it.
17/n
And we are studying the hell out of these things. E.g. this month a 40K patient study of O2 targeting was launched that will make us smarter about minimizing O2 harm ( @DogICUma). We constantly strive to innovate and improve our vent management.
https://twitter.com/WellingtonICU/status/1259740148947808257
18/n">https://twitter.com/Wellingto...
https://twitter.com/WellingtonICU/status/1259740148947808257
18/n">https://twitter.com/Wellingto...

 Read on Twitter
Read on Twitter