My team recently asked WHY we give Fe to pts with HFrEF+anemia.
First answer: b/c someone told me so
Better answer: let me get back to you on that
Let’s explore and try to understand, #medtwitter #medstudenttwitter 0/14
First answer: b/c someone told me so
Better answer: let me get back to you on that
Let’s explore and try to understand, #medtwitter #medstudenttwitter 0/14
1/First off, it helps to review a general schema for anemia.
Blood loss, decreased production, increased destruction
So, why are patients with HFrEF anemic?
Blood loss, decreased production, increased destruction
So, why are patients with HFrEF anemic?
2/Controlling for other co-morbids or meds that can lead to blood loss and destruction, it turns out that ↓RBC production drives anemia in HFrEF.
Why?
Why?
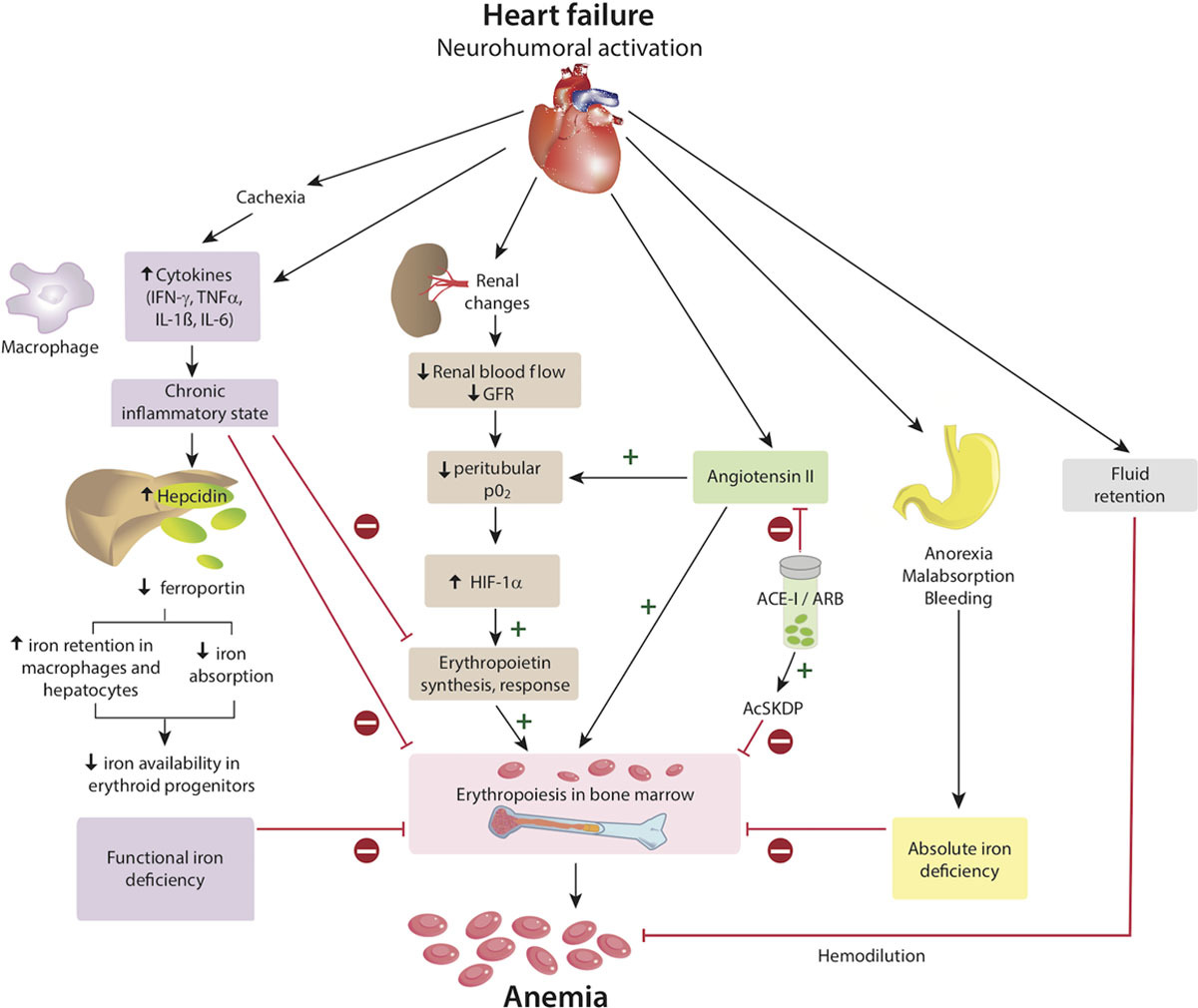
3/Turns out all these factors play a role! Some brief specifics:
Inflamm -> ↑hepcidin -> ↑sequestration ↓gut absorp
Dilution (acute exacerbation)
↓Fe (hepcidin)
CKD (EPO stimulation from ↓renal pO2 blocked by inflamm)
Graphic ( https://bit.ly/2A5BA41 )">https://bit.ly/2A5BA41&q...
Inflamm -> ↑hepcidin -> ↑sequestration ↓gut absorp
Dilution (acute exacerbation)
↓Fe (hepcidin)
CKD (EPO stimulation from ↓renal pO2 blocked by inflamm)
Graphic ( https://bit.ly/2A5BA41 )">https://bit.ly/2A5BA41&q...
4/The ACE-i bit confused me. Rabbit hole summary:
ACE nlly ↑RBCs through several pathways
ACE-i gets in the way by ↑goralatide, ↓IGF-1, and ↓IL-12 -> ↓RBCs
Clinically significant? Maybe, but still debated. I need a kidney doc.
@kidneyboy @NephJC help!
ACE nlly ↑RBCs through several pathways
ACE-i gets in the way by ↑goralatide, ↓IGF-1, and ↓IL-12 -> ↓RBCs
Clinically significant? Maybe, but still debated. I need a kidney doc.
@kidneyboy @NephJC help!
5/Phew, ok let’s uncross our eyes and do a quick recap:
So far we know that HFrEF -> multifactorial anemia. Inflammation probably leading the charge of ↓production.
Inflammation -> ↑hepcidin -> ↓available Fe ->↓Hb
So far we know that HFrEF -> multifactorial anemia. Inflammation probably leading the charge of ↓production.
Inflammation -> ↑hepcidin -> ↓available Fe ->↓Hb
6/This isn’t your everyday Fe-def anemia though.
Hepcidin is sequestering Fe in the liver and macrophages so we actually HAVE Fe, we just can’t use it -> FUNCTIONAL Fe deficiency.
Cool, so it’ll show up on Fe studies, right?
Sorta…
Hepcidin is sequestering Fe in the liver and macrophages so we actually HAVE Fe, we just can’t use it -> FUNCTIONAL Fe deficiency.
Cool, so it’ll show up on Fe studies, right?
Sorta…
7/The studies are a little tricky.
Normal Fe-def -> ↓Fe, ferritin, %sat; ↑TIBC
Fe-def in HFrEF -> ferritin <100 OR ferritin 100-299 + Tsat <20%
This criteria tries to account for ↑ferritin in inflammation (and used by all the Fe def+HF trials)
Normal Fe-def -> ↓Fe, ferritin, %sat; ↑TIBC
Fe-def in HFrEF -> ferritin <100 OR ferritin 100-299 + Tsat <20%
This criteria tries to account for ↑ferritin in inflammation (and used by all the Fe def+HF trials)
8/K, so we know Fe-def in HFrEF is functional and we can detect it. Why do we treat it?
These pts have ↓NYHA/exercise, QoL, and ↑mortality ( https://bit.ly/2A5BA41 )
Here’s">https://bit.ly/2A5BA41&q... the kicker: pts don’t have to be anemic! The Fe-def alone does it
These pts have ↓NYHA/exercise, QoL, and ↑mortality ( https://bit.ly/2A5BA41 )
Here’s">https://bit.ly/2A5BA41&q... the kicker: pts don’t have to be anemic! The Fe-def alone does it
9/Yikes! How do we treat it this? First thought was correct the anemia with ESAs. A little history:
In 2000, 142 pts in Tel Aviv w/anemia+HFrEF were given darbopoietin+Fe ->↑NYHA fxnl class.
Darbo was made king and tons of ESA trials followed.
In 2000, 142 pts in Tel Aviv w/anemia+HFrEF were given darbopoietin+Fe ->↑NYHA fxnl class.
Darbo was made king and tons of ESA trials followed.
10/The RED-HF trial was the biggest study of darbo v placebo in pts w/ HFrEF+anemia (2278 pts, rndmizd, dbl-blnd).
Sadly, death and hospitalization didn’t improve, AND there were ↑strokes and thromboembolic events.
Darbo was done.
Sadly, death and hospitalization didn’t improve, AND there were ↑strokes and thromboembolic events.
Darbo was done.
11/But, a small study of 16 pts w/HFrEF+anemia that gave IV Fe alone was published just before RED-HF.
-> ↑NYHA class, Hb, and QoL! https://bit.ly/3gtqxSW
Great!">https://bit.ly/3gtqxSW&q... We may be able to answer the, “why” of Fe rx in HFrEF.
-> ↑NYHA class, Hb, and QoL! https://bit.ly/3gtqxSW
Great!">https://bit.ly/3gtqxSW&q... We may be able to answer the, “why” of Fe rx in HFrEF.
12/Oral vs IV?
IRON-OUT (oral Fe v placebo): no ∆ in VO2max, 6MWD, ntBNP
Most studies are IV Fe b/c presumed poor PO absorp from ↑hepcidin. Findings: ↑QoL, 6MWD, NYHA
Meta-analyses (IV Fe) -> ↓hospitalizations+CV mortality+ntBNP+↑QoL
IV Fe wins.
IRON-OUT (oral Fe v placebo): no ∆ in VO2max, 6MWD, ntBNP
Most studies are IV Fe b/c presumed poor PO absorp from ↑hepcidin. Findings: ↑QoL, 6MWD, NYHA
Meta-analyses (IV Fe) -> ↓hospitalizations+CV mortality+ntBNP+↑QoL
IV Fe wins.
13/Quick note on HFpEF
The jury is still out as to whether Fe replacement helps. The FAIR-HF-HFpEF study is currently recruiting pts to try to answer this question ( https://clinicaltrials.gov/ct2/show/NCT03074591)">https://clinicaltrials.gov/ct2/show/...
The jury is still out as to whether Fe replacement helps. The FAIR-HF-HFpEF study is currently recruiting pts to try to answer this question ( https://clinicaltrials.gov/ct2/show/NCT03074591)">https://clinicaltrials.gov/ct2/show/...
14/Summary
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">HFrEF is an inflammatory state -> fxnl Fe-deficiency via hepcidin
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">HFrEF is an inflammatory state -> fxnl Fe-deficiency via hepcidin
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">↓Fe worsens outcomes in HFrEF
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">↓Fe worsens outcomes in HFrEF
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">ESAs don’t help, make things worse
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">ESAs don’t help, make things worse
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">IV Fe helps! Give it!
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">IV Fe helps! Give it!
15/Big thanks to @noahrosenberg1 and @DoctorVig’s recent #tweetorial convo for nudging me to make this.
I learned a ton and realized there’s a ton left to learn. @cardionerds @myanamandala @SalKumarMD @ceciliaberard10, #cardiotwitter, teach us more!
Fin/
I learned a ton and realized there’s a ton left to learn. @cardionerds @myanamandala @SalKumarMD @ceciliaberard10, #cardiotwitter, teach us more!
Fin/
Further reading:
https://bit.ly/2Xpypfs
https://bit.ly/2Xpypfs&q... href=" https://bit.ly/2zuM8cK
https://bit.ly/2zuM8cK&q... href=" https://bit.ly/2A5BA41
https://bit.ly/2A5BA41&q... href=" https://bit.ly/3glmYy7
https://bit.ly/3glmYy7&q... href=" https://bit.ly/3gtqxSW
https://bit.ly/3gtqxSW&q... href=" https://bit.ly/3d3Ip4E ">https://bit.ly/3d3Ip4E&q... https://bit.ly/2AbPkdC ">https://bit.ly/2AbPkdC&q...
https://bit.ly/2Xpypfs

 Read on Twitter
Read on Twitter