#Medstudenttwitter: Here& #39;s a case for you. 42 yo M presents with palpitations, BP is 125/84, HR is 250 on the monitor. Anxious but otherwise stable. The next post has his old ECG for comparison followed by a poll for what you should do next?
Feel free to post your answer and justify why you choose what you choose or to suggest an alternative treatment.
I don& #39;t expect many to get this right. Its an obscure teaching pearl, but for the #EMbound folks, this will be on your boards someday. It& #39;s also in the ACLS algorithm. The answer takes some explanation.
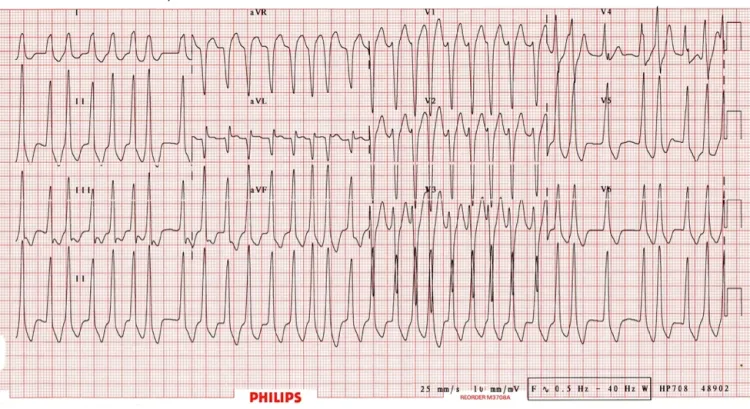
First you have to identify the ECG. If you saw my previous post on dx tachyarrythmias, this is an irregular/wide complex tachycardia. DDx: Afib with BBB, Afib with WPW, and VF/torsades. It& #39;s not the classic torsades or VF, which leaves the first two.
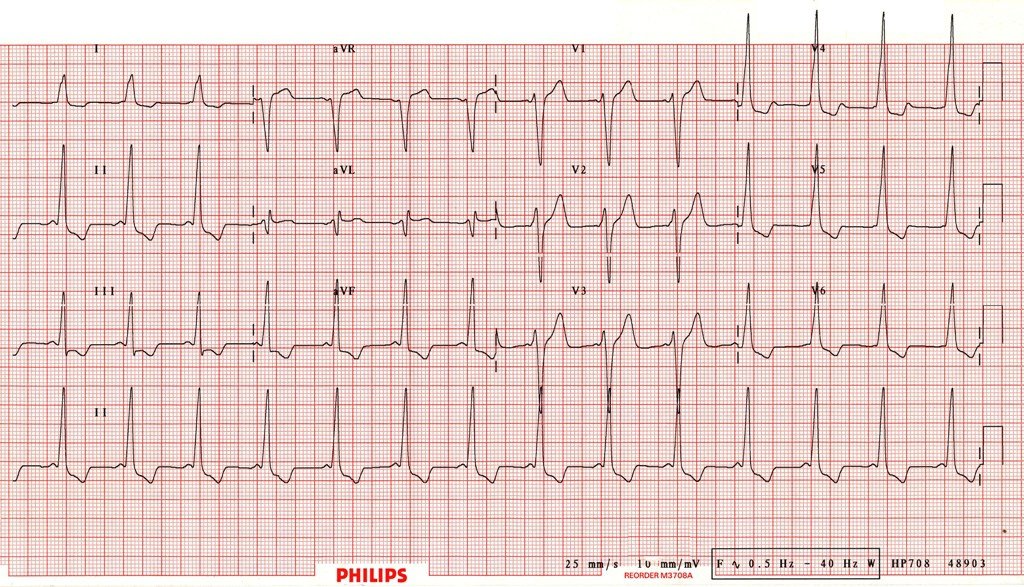
The old ECG confirms the dx. This is Afib with WPW. The old ECG shows the short PR and delta wave (upsloping start to the qrs) classic of WPW.
So how do you treat AF with WPW? And why does it matter? Well, in Afib the atria are fibrillating at like 300 times a minute. Conduction goes down both the AV node and accessory pathway. Typically, conduction is faster down the accessory pathway.
Agents that block the AV node, therefore, have the potential to cause all conduction down the accessory pathway, thereby increasing the HR, and making the patient worse. Like... dead worse. So, therefore, adenosine and diltiazem are wrong answers.
What about defibrillation? Well there is a reason I said defib and not synchronized cardioversion. Sync CV would be a legitimate treatment here. But defibrillation and sync CV are not the same thing. Defibrillation is strictly reserved for pulseless VT and VF.
You do not defibrillate someone with a pulse. You cardiovert them, with the shock synchronized so it occurs at the height of the QRS complex.
So that leaves the correct answer, which is procainamide. Not an antiarrhythmic we use commonly. But its the agent of choice for stable Afib with WPW in the ACLS algorithm because it does not affect conduction down the AV node.
If the patient was unstable, you would just perform synchronized cardioversion.
Complex case but it highlights a few good teaching points, and it is one that all the future EM docs out there need to know bc it is a favorite of board exams. And who knows, maybe you& #39;ll actually see a patient with it.

 Read on Twitter
Read on Twitter