The *alveolar poncho* (copyright @jopo899) theory of hyaline membrane deposition reminds me of a broader idea: maybe the more "pathognomonic" a finding is in a disease, the more likely it is to be protective, and the less beneficial it would be to reverse it.
1/n https://twitter.com/jopo899/status/1262125268388532225">https://twitter.com/jopo899/s...
1/n https://twitter.com/jopo899/status/1262125268388532225">https://twitter.com/jopo899/s...
Hyaline membranes are a hallmark of diffuse alveolar damage (DAD), which is the pathological hallmark of ARDS, which has been called "hyaline membrane disease" in the past. If you had to pick one specific biologic finding that implies ARDS: hyaline membranes.
2/n
2/n
So if I gave Drug X to my mice with lung injury, and found decreased hyaline membranes in the treatment group, I& #39;d think I& #39;m on the path (pardon the pun) to a cure for ARDS.
I& #39;d fling open the window of the lab and yell "I& #39;ve found the remedy for hyaline membrane disease!"
3/n
I& #39;d fling open the window of the lab and yell "I& #39;ve found the remedy for hyaline membrane disease!"
3/n
But the "alveolar poncho" theory reminds us that in biology, like in economics, every transaction has externalities. Unmeasured (and often unpredictable) costs.
I bet my hyaline membrane-free mice would have worsened alveolar flooding and slower resolution of lung injury.
4/n
I bet my hyaline membrane-free mice would have worsened alveolar flooding and slower resolution of lung injury.
4/n
If a feature of a disease is really "pathognomonic," especially in critical illness, there& #39;s reason to think that it& #39;s a product of millions of years of evolution trying to keep us alive long enough to reproduce. And blocking it may not help, and may even hurt.
5/n
5/n
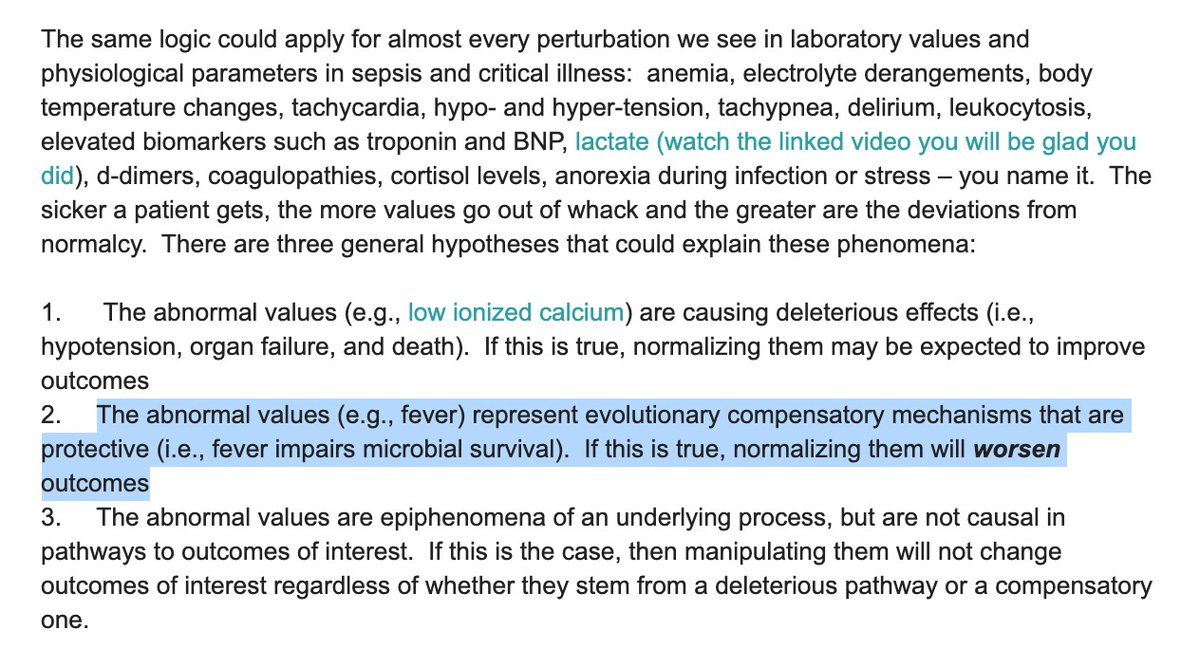
There are a couple of nice @phlegmfighter essays on this idea and the "normalization fallacy":
https://www.medicalevidenceblog.com/2017/02/quasipotent-tale-of-three-hypotheses.html
https://www.medicalevidenceblog.com/2017/02/q... href=" https://www.sciencedirect.com/science/article/abs/pii/S0306987709000334
6/n">https://www.sciencedirect.com/science/a...
https://www.medicalevidenceblog.com/2017/02/quasipotent-tale-of-three-hypotheses.html
6/n">https://www.sciencedirect.com/science/a...
Once you embrace this idea as plausible, you end up in some interesting places. Like: maybe the "cytokine storm" of sepsis (and COVID!) isn& #39;t a "dysregulated host response" but is instead the body& #39;s evolutionarily conserved and carefully-calibrated response to infection.
7/n
7/n
And maybe this helps explain why >150 clinical trials trying to blunt the immune response in sepsis haven& #39;t yielded a single effective therapy. And probably won& #39;t in COVID.
8/n
8/n
And maybe why the kidney injury in sepsis ISN& #39;T due to hypoperfusion and necrosis (and helped by augmented perfusion), but instead functional "hibernation."
https://www.atsjournals.org/doi/full/10.1164/rccm.201511-2285OC
9/n">https://www.atsjournals.org/doi/full/...
https://www.atsjournals.org/doi/full/10.1164/rccm.201511-2285OC
9/n">https://www.atsjournals.org/doi/full/...
And maybe why forcing more calories into critically ill patients to combat skeletal muscle loss hasn& #39;t helped them. Maybe the body knows better than we do whether anabolism vs catabolism is more appropriate.
https://podcasts.apple.com/us/podcast/coda-change/id648203376?i=1000463521058
10/n">https://podcasts.apple.com/us/podcas...
https://podcasts.apple.com/us/podcast/coda-change/id648203376?i=1000463521058
10/n">https://podcasts.apple.com/us/podcas...
And writ large: maybe organ failure itself in the ICU is a feature - not a bug - of how we survive tremendous surges of inflammation and stress.
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(04)16815-3/fulltext
11/n">https://www.thelancet.com/journals/...
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(04)16815-3/fulltext
11/n">https://www.thelancet.com/journals/...
I mean, how much of critical care research has been trying to cure shock by improving O2 delivery? By augmenting Hgb, SaO2, cardiac output, MAP, etc.. How many have worked?
12/n
12/n
I& #39;m not a therapeutic nihilist. I believe one day we& #39;ll have therapies that accelerate recovery of organ function, and we& #39;ll have more to offer our patients than supportive care. But it& #39;ll take a much less simplistic understanding of pathogenesis that we& #39;re currently using.
13/n
13/n
We identified the gene that causes cystic fibrosis > 30 years ago. And only last year did we get the "game changer" drug we were waiting for. And CF is a single-gene disorder! How much more primitive is our understanding of sepsis, ARDS, MOF?
14/n
14/n

 Read on Twitter
Read on Twitter
 https://www.sciencedirect.com/science/a..." title="There are a couple of nice @phlegmfighter essays on this idea and the "normalization fallacy": https://www.medicalevidenceblog.com/2017/02/q... href=" https://www.sciencedirect.com/science/article/abs/pii/S03069877090003346/n">https://www.sciencedirect.com/science/a...">
https://www.sciencedirect.com/science/a..." title="There are a couple of nice @phlegmfighter essays on this idea and the "normalization fallacy": https://www.medicalevidenceblog.com/2017/02/q... href=" https://www.sciencedirect.com/science/article/abs/pii/S03069877090003346/n">https://www.sciencedirect.com/science/a...">
 https://www.sciencedirect.com/science/a..." title="There are a couple of nice @phlegmfighter essays on this idea and the "normalization fallacy": https://www.medicalevidenceblog.com/2017/02/q... href=" https://www.sciencedirect.com/science/article/abs/pii/S03069877090003346/n">https://www.sciencedirect.com/science/a...">
https://www.sciencedirect.com/science/a..." title="There are a couple of nice @phlegmfighter essays on this idea and the "normalization fallacy": https://www.medicalevidenceblog.com/2017/02/q... href=" https://www.sciencedirect.com/science/article/abs/pii/S03069877090003346/n">https://www.sciencedirect.com/science/a...">