1/ Interesting paper in @TheLancet from New York reporting the epidemiology and outcomes for critically ill COVID-19 patients: https://www.thelancet.com/action/showPdf?pii=S0140-6736%2820%2931189-2.
They">https://www.thelancet.com/action/sh... did some inferential modeling to try to find associations with mortality in COVID, which I think could be misleading...
They">https://www.thelancet.com/action/sh... did some inferential modeling to try to find associations with mortality in COVID, which I think could be misleading...
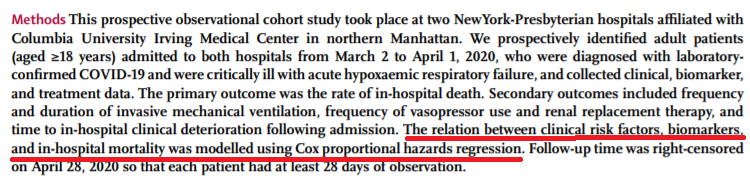
2/ They used a Cox proportional hazards model to test the association between multiple variables and in-hospital death.
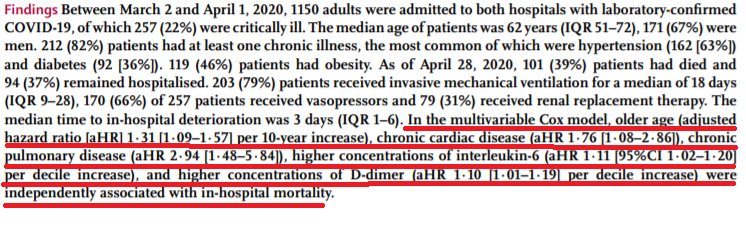
Unsurprisingly significant associations were found for age, and cardiac and pulmonary disease. They also found significant associations for D-dimer and IL-6.
Unsurprisingly significant associations were found for age, and cardiac and pulmonary disease. They also found significant associations for D-dimer and IL-6.
3/ IL-6 had an adjusted hazard ratio of 1.11!! So that means for a 1 unit increase in IL-6 you have a:
a) 11% increase in risk of death
b) 11% increase in risk of death at any given time assuming you have survived until that point in time
a) 11% increase in risk of death
b) 11% increase in risk of death at any given time assuming you have survived until that point in time
4/ B has more words...so is obviously the right answer.
5/ What I think is important here is that the hazard ratio involves time because the unit of analysis in a Cox model is patient time. Patients contribute time to the analysis until they have a failure (death) or are censored (discharged or the study period has ended).
6/ This means that a patient admitted at the start of the study period, who remains ventilated and in the ICU at the end of the study contributes more to the analysis than the patient who either dies or is discharged within 1 day.
7/ This also means that same patient has had an outcome (still being in hospital) that is considered the same as being discharged from hospital.
Particularly problematic when there is a reasonable chance some of these patients who are in hospital will still die.
Particularly problematic when there is a reasonable chance some of these patients who are in hospital will still die.
8/ When you combine the above 2 points, the model actually seems to favor variables associated with patients having long stays in hospital and not yet dying over patients who get better and discharged quickly.
9/ Imagine a study with 40 pts (enrolled on day 1), 20 receive drug X and 20 receive placebo. It turns out this drug gets patients better and discharged from hospital in 2 days. Unfortunately, every patient in the placebo group is still in the ICU at the study end on day 28.
10/ 2 patients, 1 in each group, are so sick, they die on day 5 no matter what you do.
So, intervention: 1 patient died on day 5 and 19 patients were discharged from hospital on day 2.
Control: 1 patient died on day 5 and 19 patients were still in the ICU day 28.
So, intervention: 1 patient died on day 5 and 19 patients were discharged from hospital on day 2.
Control: 1 patient died on day 5 and 19 patients were still in the ICU day 28.
11/ What is the hazard ratio associating the drug with death?
12/ The answer is 20 (harmful). That is because of the longer follow-up time for the placebo group. This is despite the fact that the treatment in this made-up example was clearly beneficial.
This is the danger of using survival analysis when studying mortality in the ICU.
This is the danger of using survival analysis when studying mortality in the ICU.
13/ Alternatively, ICU studies investigating associations with mortality often use logistic regression models.
The unit of analysis for these models is individual patients, so a patient admitted for 48 hours contributes as much as one admitted for the entire study.
The unit of analysis for these models is individual patients, so a patient admitted for 48 hours contributes as much as one admitted for the entire study.
14/ Studies using these models often follow patients for 28 days* because they still need enough follow-up time for the patient to have an event (death) if they are going to have one.
*28 days will likely not be long enough in COVID
*28 days will likely not be long enough in COVID
15/ This can still be flawed, in the above example a logistic regression model would find drug X to have an OR of 1 because 1/20 people died in each group, but at least it didn& #39;t find harm.
16/ The benefit of using a Cox model here is that there is more patient time available to analyze than there are patients. This means that you have more power (probability of accepting the alternate hypothesis when it is true) for a given sample size.
17/ This may be OK in a study like this where associations with mortality are not the focus of the paper and clearly meant to be hypothesis generating only.
However, I personally think it would be best not to do any inferential analysis at all in a scenario like this...
However, I personally think it would be best not to do any inferential analysis at all in a scenario like this...
18/ ...but if you were, I think it would be better to either perform a competing risk analysis for ICU/hospital discharge with death being a competing risk.

 Read on Twitter
Read on Twitter