Now online @bmj_latest! #COVID19 outcomes & risks @nyulangone among 5,279 patients (2,741 hospitalized). Thread with details and some special twitter bonus content. @petrillimd @jones_prof @WhiteCoatLuke @Cerf_MD @Francois1Fritz https://www.bmj.com/content/369/bmj.m1966">https://www.bmj.com/content/3...
Those of you who saw our previous preprint: this version is substantially altered – updated data, comprehensive follow up, new analyses. E.g., 94% of the hospitalized patients have been discharged or died, giving us robust estimates of final outcomes. Some highlights follow.
Context: we include all patients testing positive for #COVID19 between March 1 and April 8, with follow up (in the paper) through May 5 (and here in this thread, through this morning!). We restrict to those positive before April 9 to ensure adequate follow up for outcomes.
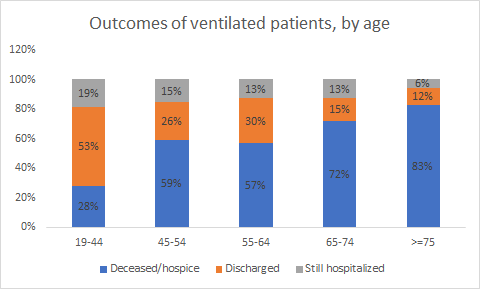
1st, outcomes for hospitalized patients: 24% died or went to hospice, 6% still hospitalized. (Bonus Twitter update: now at 25% died/hospice, 3% still hospitalized.) 647 (24%) were ventilated, of whom 60% died/hospice, 16% discharged, 23% still hospitalized (now 63%, 24%, 13%).
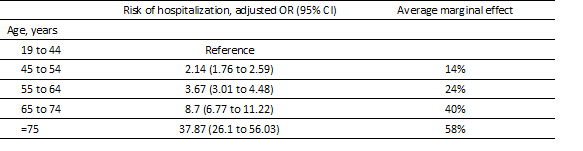
Now for factors associated with adverse outcomes. First, hospitalization. Biggest risk is still age. We now show average marginal effects to make ORs more interpretable: e.g. risk of hospitalization for >=75 years is 58 pct points higher than those 19-44. h/t @kit_delgadoMD
Other key risks heart failure (22pct points increased risk), male (16pp), chronic kidney disease (14pp), any increase in BMI (14pp for BMI 40+).
As previously shown current/former smoker “protective” BUT unknown smoking status 5pp increased risk. *I do not think smoking is good for you.* Other possible explanations: 1) smokers more likely to be tested b/c perceived higher risk; 2) smokers don’t want to admit it = unknown.
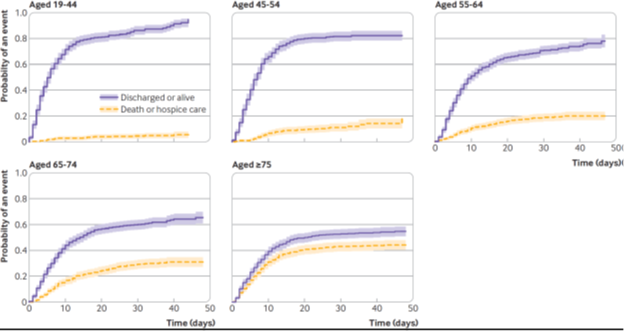
What about critical illness (ICU, ventilator, death) & death? As shown in preprint, additional risk age/comorbidity smaller once hospitalized though still present for age, unknown smoking status, BMI 40+, heart failure. Here& #39;s cumulative hazard of death by age group.
Special bonus Twitter-only graphic: unadjusted outcomes among the subset of ventilated patients, by age.
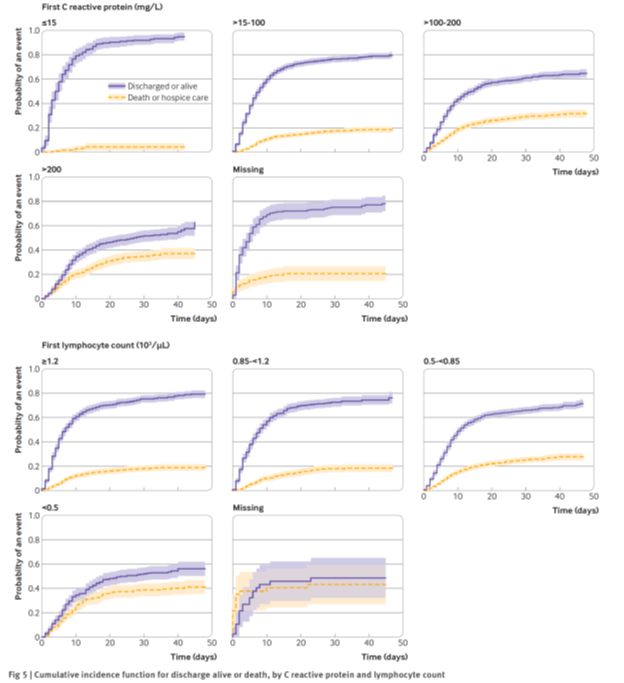
And still true: hypoxia on presentation and inflammatory labs bigger risks for critical illness than comorbidity among hospitalized group.
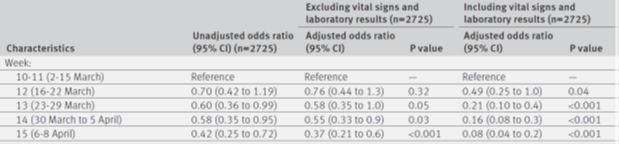
*New results* But this result is my favorite: adjusted risk of critical illness decreases every week. Are we getting better at taking care of these patients even without blockbuster drug, definitive treatments? I think we may be.
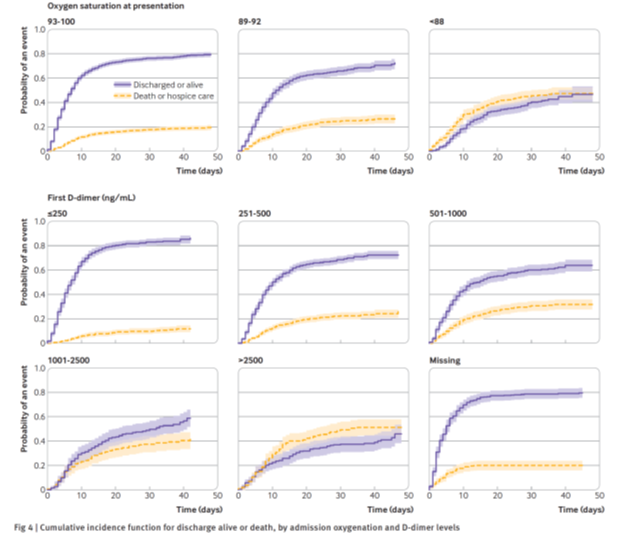
*New analyses* we have added a competing risk survival model for mortality to this paper (competing risk=discharge, since we don’t know if die post-discharge). Here you can see the dramatic differences in mortality by O2 sat and D-dimer on admission.
Finally, we do a number of sensitivity analyses (i.e. restricting non-hospitalized comparison group to those tested in ED; adding in ED patients with suspected covid but not tested to non-hospitalized groups) – similar results.
Thanks as always to extraordinary team here @nyulangone, to #medtwitter for feedback on preprint & to the thoughtful reviewers who inspired many improvements. BMJ has open peer review so you will be able to see their comments and names posted online with the paper.

 Read on Twitter
Read on Twitter