Promised to tweet out a few more thoughts from my reporting on #covid19 clustering and dispersion factor k. So here goes: https://twitter.com/kakape/status/1262876041237991424">https://twitter.com/kakape/st...
Quick recap first: Reproduction number R is an average. R = 3 does not mean every person infects three others. It’s more like busses that “come” every 10 minutes and you end up waiting 30 minutes and 3 come along.
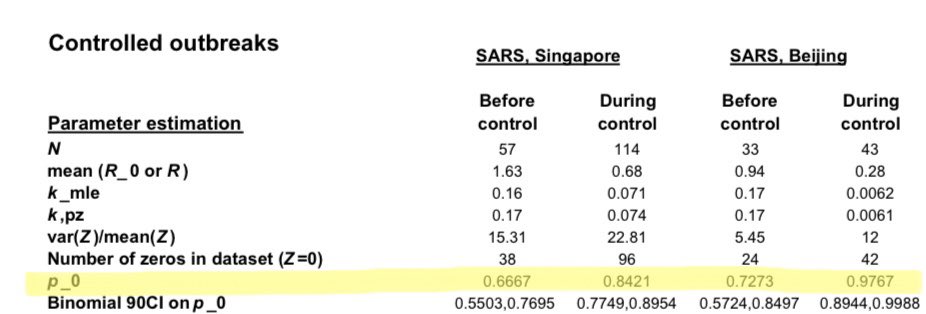
In reality some people infect a lot of people and most people infect no-one. That’s particularly pronounced in coronaviruses like SARS. In his 2004 Nature paper @jlloydsmith estimates that in Singapore before control measures 2/3 of people with #SARS did not transmit at all.
Data suggests that something similar is happening with #Covid19. This preprint by @AdamJKucharski and others estimates “that 80% of secondary transmissions may have been caused by a small fraction of infectious individuals (~10%)” https://wellcomeopenresearch.org/articles/5-67 ">https://wellcomeopenresearch.org/articles/...
That means spread of #covid19 “could be drastically reduced by preventing relatively rare superspreading events”. But to prevent them you have to know how/why/where they happen. And researchers know surprisingly little about this. But there are at least three levels at play:
1. The virus: Why do SARS and #SARSCoV2 cluster more than others? It’s not clear. It might have to do with mostly spreading via droplets and then sometimes - under the right circumstances - as an aerosol. It’s “a really interesting open scientific question,” says @ChristoPhraser
2. The individual: This is dicey. We avoid the term “superspreaders” to avoid stigmatizing people but that’s not to say that individual variation does not play a role. Infections develop differently in different people which could lead to higher or lower virus shedding.
There is other variation: Some people emit more particles when they speak, for instance. And behavior plays a role as well: How many social contacts does someone have? How often do they wash their hands? We know far too little to pinpoint people at a higher risk of superspreading
3. The setting: This is the one most likely to yield some actionable insights soon. We’ve all seen reports of outbreaks linked to cruise ships, meat processing plants, religious gatherings, workers dormitories, gyms, bars, clubs, restaurants.
As a first step we have to try and understand what settings are linked to #covid19 clusters. Gwenan Knight at @LSHTM has done that in this preprint (which comes with an online database of reported clusters) https://wellcomeopenresearch.org/articles/5-83/v1">https://wellcomeopenresearch.org/articles/...
As the paper points out there are all kinds of biases to contend with: People are more likely to remember big events for instance and thus attribute infection to those. Plus, of course, it’s hard to collect meaningful data on superspreading when large gatherings are banned.
But some hypotheses are emerging about what might link some of these settings incl. the idea that places where people sing/shout may be particularly prone to superspreading of #covid19. Way too early to know, but this is the kind of research I’d love to see more of.
For now, given what we know:
Banning large gatherings (and smaller ones) probably big part of #shutdown success
Working from home probably helps a lot with that
Masking everyone could help because then “superemitters” also wear masks and that might reduce spread from them
Banning large gatherings (and smaller ones) probably big part of #shutdown success
Working from home probably helps a lot with that
Masking everyone could help because then “superemitters” also wear masks and that might reduce spread from them
Where gathering people indoors (especially vulnerable populations) is hard to avoid (hospitals, prisons, etc) extra measures should be taken. In the case of prisons that includes release of some people. Good @WHO document on that here: https://www.who.int/news-room/detail/13-05-2020-unodc-who-unaids-and-ohchr-joint-statement-on-covid-19-in-prisons-and-other-closed-settings">https://www.who.int/news-room...
And finally: We need to understand clustering of #covid19 better. That means more data is needed, more testing, more contact tracing, incl. detailed epidemiological investigations.

 Read on Twitter
Read on Twitter