Oh shit. Finally a study is out rigorously quantifying #SARSCoV2 #COVID19 #coronavirus in stool. Bad news...there& #39;s infectious virus in there. So fecal transmission is possible, but is it happening in the real world?
https://wwwnc.cdc.gov/eid/article/26/8/20-0681_article?deliveryName=USCDC_333-DM28664">https://wwwnc.cdc.gov/eid/artic...
https://wwwnc.cdc.gov/eid/article/26/8/20-0681_article?deliveryName=USCDC_333-DM28664">https://wwwnc.cdc.gov/eid/artic...
Previous data showed viral RNA in stool by PCR, but that doesn& #39;t measure infectious virus. To do that, you need to take the sample and see if it can kill cells in culture to form a plaque. By serially diluting the sample, you can quantify plaque-forming (infectious) units (PFU)
Here, Xiao et al report that they followed my PhD mentor @profvrr& #39;s old advice: real virologists always do the plaque assay. For more on plaque assays, check out Dr. Racaniello& #39;s great explainer piece:
https://www.virology.ws/2009/07/06/detecting-viruses-the-plaque-assay/">https://www.virology.ws/2009/07/0...
https://www.virology.ws/2009/07/06/detecting-viruses-the-plaque-assay/">https://www.virology.ws/2009/07/0...
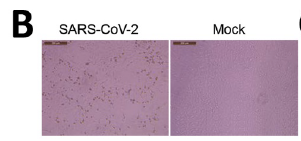
The study authors collected fecal samples from 28 patients hospitalized with #COVID19. 12 had stool that was PCR+ for #SARSCoV2 RNA. They tested stool from 3 pts to see if there was virus that could infect VeroE6 cells. 2/3 pts did. Cytopathic effect (CPE; dying cells) observed:
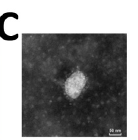
They also showed that you can detect virus particles being produced by VeroE6 cells in culture using transmission electron microscopy:
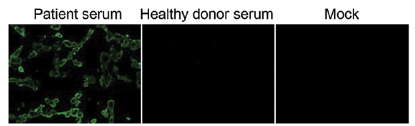
They also found anti-spike antibodies in the patient& #39;s blood, and used those antibodies to detect infectious virus from the stool swabs by immunofluorescent staining. That& #39;s the panel on the left. Antibodies bind virus being produced by infected cells, and they fluoresce green.
It& #39;s worth noting that they had to do this with 2 rounds of virus passage. They infected VeroE6 cells, waited a few days for virus to grow, then infected fresh cells with that virus. That may be because infectious virus titers were too low or the samples were toxic to the cells.
This is relevant because they actually didn& #39;t quantify infectious titers by plaque assay. I& #39;m not sure why they didn& #39;t...it& #39;s possible that either virus in fecal swabs was below the limit of detection of the plaque assay or the samples were too...um, crappy...to get clean plaques
They did do a standard curve with virus stock to estimate PFU equivalents by PCR. This shows that PFU equivalents in stool were higher than in nasal or oral swabs, and that there were 2 logs (100X) more virus in stool compared to oral swabs. That& #39;s somewhat alarming.
The authors bring up SARS classic transmission at Amoy Gardens housing complex in Hong Kong. 329 people were infected, and the source was later found to be faulty sewage lines that aerosolized virus in feces. But the real world implications of this study are somewhat unclear.
People have been worrying about "toilet plumes" for a long time (here& #39;s a fun review on the topic), but the actual risk probably depends a lot on the pathogen. It& #39;s hard to determine this experimentally for several reasons. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4692156/">https://www.ncbi.nlm.nih.gov/pmc/artic...
For #SARSCoV2, I don& #39;t know of epidemiological evidence of toilet plume transmission. Also, to test this in animals, you& #39;d need to do it in an ABSL-3 lab, & these aren& #39;t equipped with experimental toilets. Maybe aerobiologists can weigh in on toilet plume simulation models?
Also, the patient studied in detail was very sick. He died 2 weeks after the last sample was taken, so it& #39;s hard to say if people who recover from #COVID19 are producing infectious virus in their stool. The risk of fecal transmission remains unclear.

 Read on Twitter
Read on Twitter