68 yo
RR 40, Sat 94% Room Air, BP 157/74 HR 124. Alert. Bibasilar crackles
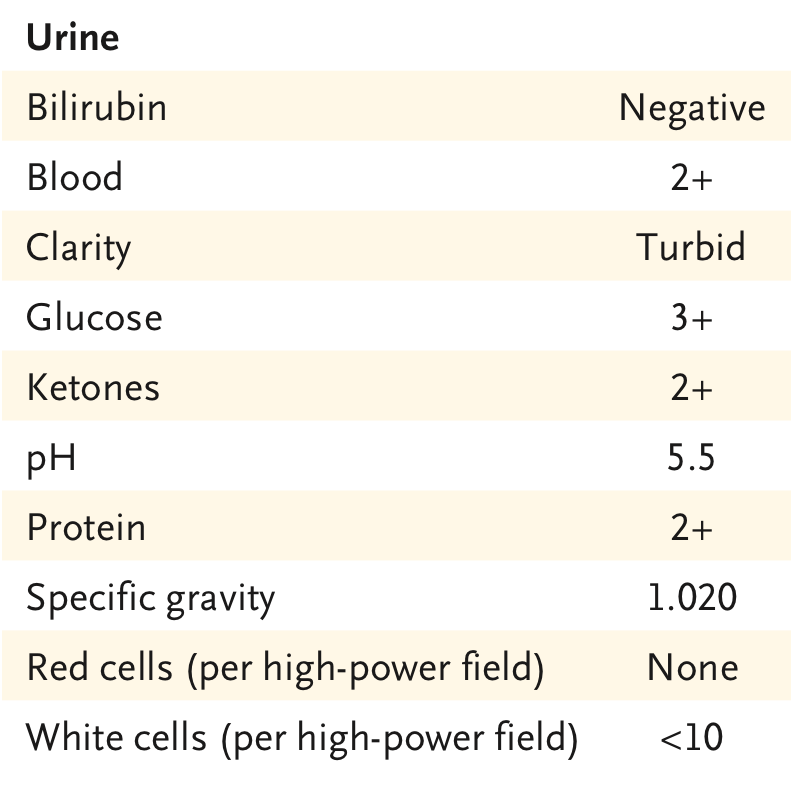
Labs: Cr 1.3 (baseline 0.8), WBC 10, K 5.4, HCO3 17, CK 184. UA and CXR
How would you manage this AKI initially? What is the likely cause of AKI in patients with #COVID19? (this last question discussed in thread  https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧵" title="Thread" aria-label="Emoji: Thread">)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧵" title="Thread" aria-label="Emoji: Thread">)
No easy answer except to say that FENa is very unlikely to be useful. It is not unreasonable to try fluids for AKI in the setting of perceived hypovolemia. However, this gets complicated when the potential for worsening ARDS exists. I& #39;ll try to tackle the answers one by one  https://abs.twimg.com/emoji/v2/... draggable="false" alt="💪" title="Flexed biceps" aria-label="Emoji: Flexed biceps">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💪" title="Flexed biceps" aria-label="Emoji: Flexed biceps">
Infusing 1 L of HES to patients with compensated HFpEF altered intra-renal venous flow and this induced diuretic resistance. Increased CVP and alterations of IRVF have been linked to worsening renal function (Renosarca). ARDS / Sepsis is already a sign of poor volume tolerance https://abs.twimg.com/emoji/v2/... draggable="false" alt="🚨" title="Police cars revolving light" aria-label="Emoji: Police cars revolving light">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🚨" title="Police cars revolving light" aria-label="Emoji: Police cars revolving light">
Ideally you would want to know if patient will respond to fluids before giving them. This is hard to do on the ED. However, the reason to give fluids would be to increase  https://abs.twimg.com/emoji/v2/... draggable="false" alt="♥️" title="Heart suit" aria-label="Emoji: Heart suit">stroke volume. If stroke volume is normal/high, fluids make no sense! This can be measured easily!
https://abs.twimg.com/emoji/v2/... draggable="false" alt="♥️" title="Heart suit" aria-label="Emoji: Heart suit">stroke volume. If stroke volume is normal/high, fluids make no sense! This can be measured easily!
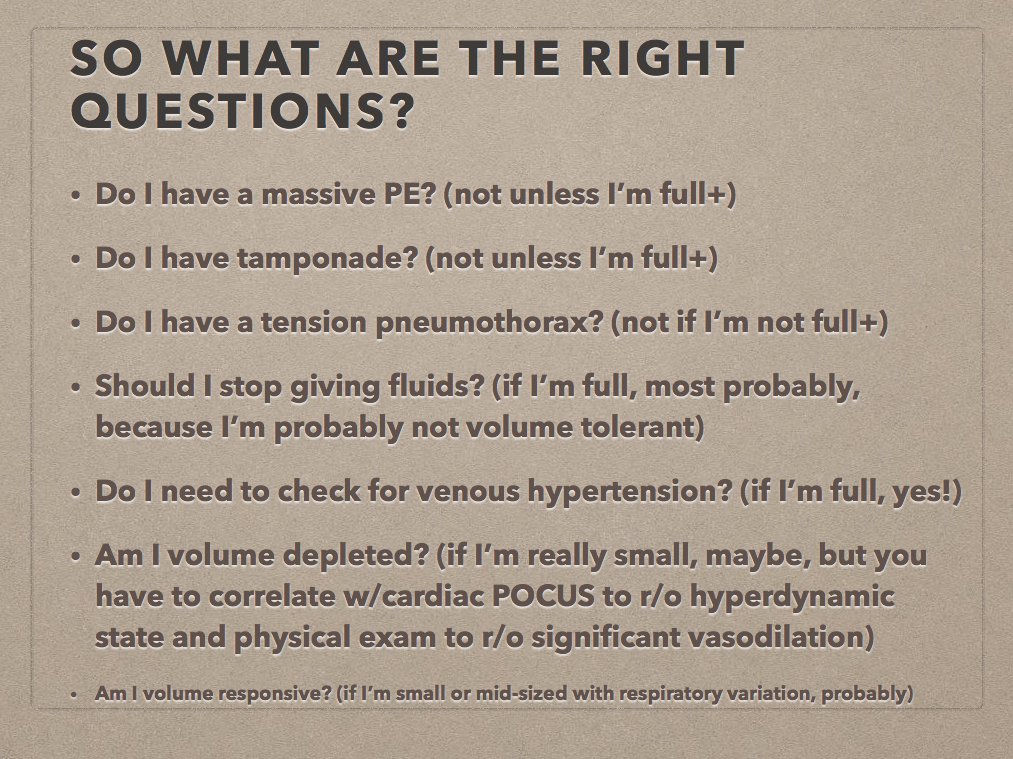
You should also want to asses venous congestion before giving fluids. Lung Ultrasound is going to be useless because of ARDS. #IVC can help a LOT if you ask the right questions. A plethoric IVC means pt is unlikely to respond to fluids https://thinkingcriticalcare.com/2019/03/13/my-friend-the-ivc-foamed-foamer-foamus-foamcc/">https://thinkingcriticalcare.com/2019/03/1...
#POCUS evaluation of stroke volume (LVOT VTI) and volume tolerance (IVC) takes 1-2 minutes and can add a ton of valuable information before deciding to give fluids!
If pt is transferred to the ICU and advanced monitoring is available, CO monitoring with Passive leg rise (PLR) guided fluid resuscitation has been shown to decrease the need for dialysis and mechanical ventilation.
*Before performing PLR authors determined if SV was inadequate
*Before performing PLR authors determined if SV was inadequate
Etiology of AKI in #COVID19 is likely to be complex. Definitely some patients can present with severe diarrhea and could have a component of volume depletion. However, it is likely that most AKI is not a volume problem https://twitter.com/VelezNephHepato/status/1250656930986680320?s=20">https://twitter.com/VelezNeph...
Reports from  https://abs.twimg.com/emoji/v2/... draggable="false" alt="🇨🇳" title="Flag of China" aria-label="Emoji: Flag of China"> show
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🇨🇳" title="Flag of China" aria-label="Emoji: Flag of China"> show  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">incidence of hematuria and proteinuria (as in this patient). Autopsies show tubular necrosis, obstruction of peritubular capillary lumens and glomerular capillary loops. Today @NEJM published convincing evidence of #SARSCov2 directly involving the kidney!
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">incidence of hematuria and proteinuria (as in this patient). Autopsies show tubular necrosis, obstruction of peritubular capillary lumens and glomerular capillary loops. Today @NEJM published convincing evidence of #SARSCov2 directly involving the kidney!
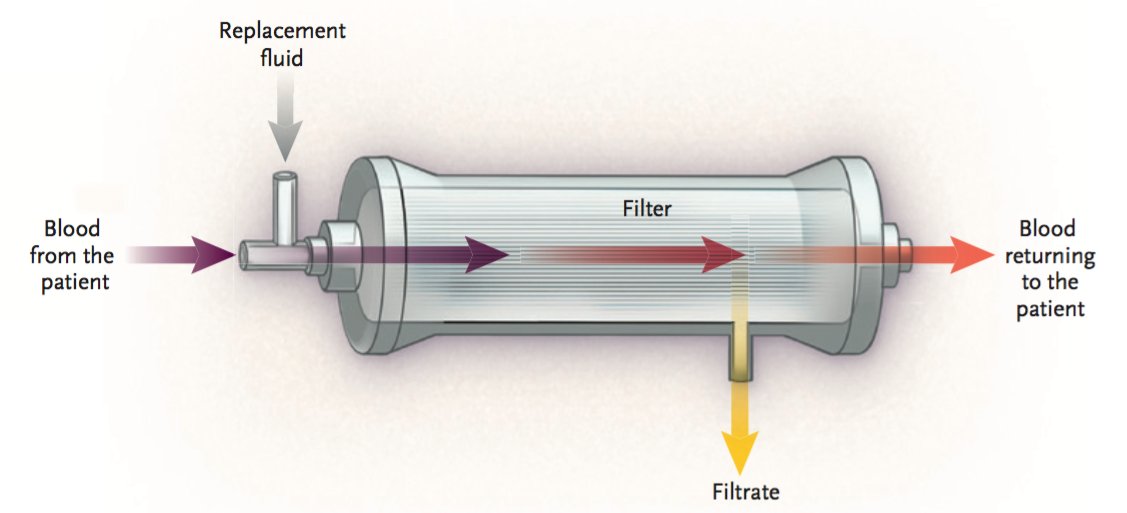
This patient was actually given 2 L IV fluid with no improvement on kidney function. Eventually required RRT with CRRT. Given I know nothing about CRRT, I hope my good friend @galindozip can complement this thread with his awesome knowledge!
Thank you for reading! Here is a link to the full case: https://www.nejm.org/doi/full/10.1056/NEJMcpc2002418?query=featured_home">https://www.nejm.org/doi/full/...

 Read on Twitter
Read on Twitter AKI and #COVID19 68 yo https://abs.twimg.com/emoji/v2/... draggable="false" alt="♂️" title="Male sign" aria-label="Emoji: Male sign"> PMH obesity, HTN, CAD w stent, OSA, T2DMhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Rightwards arrow" aria-label="Emoji: Rightwards arrow"> ED w SOB + fever 39.9°C. Poor oral intakeRR 40, Sat 94% Room Air, BP 157/74 HR 124. Alert. Bibasilar cracklesLabs: Cr 1.3 (baseline 0.8), WBC 10, K 5.4, HCO3 17, CK 184. UA and CXRhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Down pointing backhand index" aria-label="Emoji: Down pointing backhand index"> (case from @NEJM)" title="https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧵" title="Thread" aria-label="Emoji: Thread"> AKI and #COVID19 68 yo https://abs.twimg.com/emoji/v2/... draggable="false" alt="♂️" title="Male sign" aria-label="Emoji: Male sign"> PMH obesity, HTN, CAD w stent, OSA, T2DMhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Rightwards arrow" aria-label="Emoji: Rightwards arrow"> ED w SOB + fever 39.9°C. Poor oral intakeRR 40, Sat 94% Room Air, BP 157/74 HR 124. Alert. Bibasilar cracklesLabs: Cr 1.3 (baseline 0.8), WBC 10, K 5.4, HCO3 17, CK 184. UA and CXRhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Down pointing backhand index" aria-label="Emoji: Down pointing backhand index"> (case from @NEJM)">
AKI and #COVID19 68 yo https://abs.twimg.com/emoji/v2/... draggable="false" alt="♂️" title="Male sign" aria-label="Emoji: Male sign"> PMH obesity, HTN, CAD w stent, OSA, T2DMhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Rightwards arrow" aria-label="Emoji: Rightwards arrow"> ED w SOB + fever 39.9°C. Poor oral intakeRR 40, Sat 94% Room Air, BP 157/74 HR 124. Alert. Bibasilar cracklesLabs: Cr 1.3 (baseline 0.8), WBC 10, K 5.4, HCO3 17, CK 184. UA and CXRhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Down pointing backhand index" aria-label="Emoji: Down pointing backhand index"> (case from @NEJM)" title="https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧵" title="Thread" aria-label="Emoji: Thread"> AKI and #COVID19 68 yo https://abs.twimg.com/emoji/v2/... draggable="false" alt="♂️" title="Male sign" aria-label="Emoji: Male sign"> PMH obesity, HTN, CAD w stent, OSA, T2DMhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Rightwards arrow" aria-label="Emoji: Rightwards arrow"> ED w SOB + fever 39.9°C. Poor oral intakeRR 40, Sat 94% Room Air, BP 157/74 HR 124. Alert. Bibasilar cracklesLabs: Cr 1.3 (baseline 0.8), WBC 10, K 5.4, HCO3 17, CK 184. UA and CXRhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Down pointing backhand index" aria-label="Emoji: Down pointing backhand index"> (case from @NEJM)">
 AKI and #COVID19 68 yo https://abs.twimg.com/emoji/v2/... draggable="false" alt="♂️" title="Male sign" aria-label="Emoji: Male sign"> PMH obesity, HTN, CAD w stent, OSA, T2DMhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Rightwards arrow" aria-label="Emoji: Rightwards arrow"> ED w SOB + fever 39.9°C. Poor oral intakeRR 40, Sat 94% Room Air, BP 157/74 HR 124. Alert. Bibasilar cracklesLabs: Cr 1.3 (baseline 0.8), WBC 10, K 5.4, HCO3 17, CK 184. UA and CXRhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Down pointing backhand index" aria-label="Emoji: Down pointing backhand index"> (case from @NEJM)" title="https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧵" title="Thread" aria-label="Emoji: Thread"> AKI and #COVID19 68 yo https://abs.twimg.com/emoji/v2/... draggable="false" alt="♂️" title="Male sign" aria-label="Emoji: Male sign"> PMH obesity, HTN, CAD w stent, OSA, T2DMhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Rightwards arrow" aria-label="Emoji: Rightwards arrow"> ED w SOB + fever 39.9°C. Poor oral intakeRR 40, Sat 94% Room Air, BP 157/74 HR 124. Alert. Bibasilar cracklesLabs: Cr 1.3 (baseline 0.8), WBC 10, K 5.4, HCO3 17, CK 184. UA and CXRhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Down pointing backhand index" aria-label="Emoji: Down pointing backhand index"> (case from @NEJM)">
AKI and #COVID19 68 yo https://abs.twimg.com/emoji/v2/... draggable="false" alt="♂️" title="Male sign" aria-label="Emoji: Male sign"> PMH obesity, HTN, CAD w stent, OSA, T2DMhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Rightwards arrow" aria-label="Emoji: Rightwards arrow"> ED w SOB + fever 39.9°C. Poor oral intakeRR 40, Sat 94% Room Air, BP 157/74 HR 124. Alert. Bibasilar cracklesLabs: Cr 1.3 (baseline 0.8), WBC 10, K 5.4, HCO3 17, CK 184. UA and CXRhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Down pointing backhand index" aria-label="Emoji: Down pointing backhand index"> (case from @NEJM)" title="https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧵" title="Thread" aria-label="Emoji: Thread"> AKI and #COVID19 68 yo https://abs.twimg.com/emoji/v2/... draggable="false" alt="♂️" title="Male sign" aria-label="Emoji: Male sign"> PMH obesity, HTN, CAD w stent, OSA, T2DMhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Rightwards arrow" aria-label="Emoji: Rightwards arrow"> ED w SOB + fever 39.9°C. Poor oral intakeRR 40, Sat 94% Room Air, BP 157/74 HR 124. Alert. Bibasilar cracklesLabs: Cr 1.3 (baseline 0.8), WBC 10, K 5.4, HCO3 17, CK 184. UA and CXRhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Down pointing backhand index" aria-label="Emoji: Down pointing backhand index"> (case from @NEJM)">
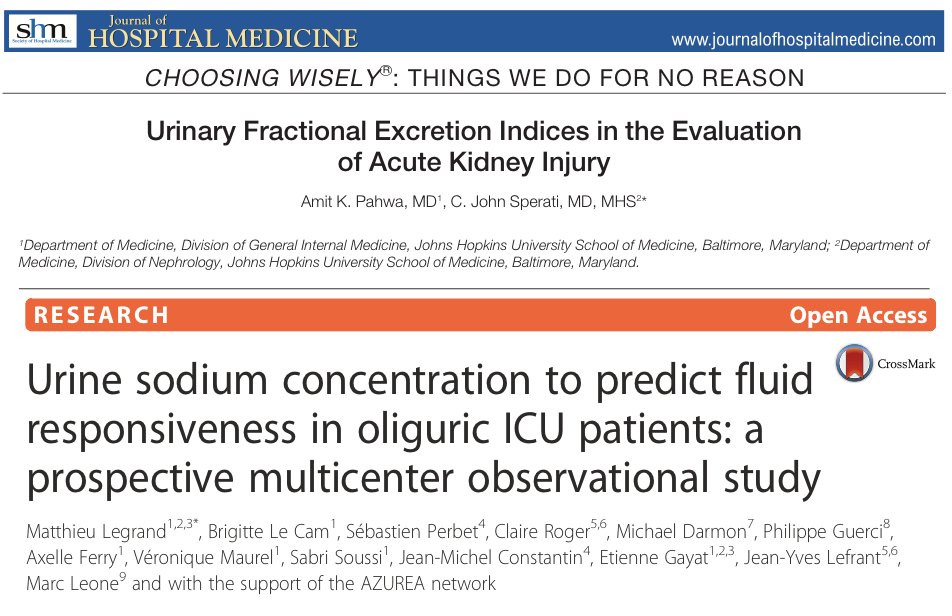 FENa: Hypovolemia + normal tubular function should lead to https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">Na reabsorption and a FENa < 1%. Tubular injury https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Rightwards arrow" aria-label="Emoji: Rightwards arrow"> inappropriate Na wasting https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Rightwards arrow" aria-label="Emoji: Rightwards arrow">FENa > 3%. https://abs.twimg.com/emoji/v2/... draggable="false" alt="🚨" title="Police cars revolving light" aria-label="Emoji: Police cars revolving light">Patchy tubular, glomerular and vascular disease can cause falsely low FENa thus is a poor predictor of fluid responsiveness." title="https://abs.twimg.com/emoji/v2/... draggable="false" alt="1⃣" title="Keycap digit one" aria-label="Emoji: Keycap digit one">FENa: Hypovolemia + normal tubular function should lead to https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">Na reabsorption and a FENa < 1%. Tubular injury https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Rightwards arrow" aria-label="Emoji: Rightwards arrow"> inappropriate Na wasting https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Rightwards arrow" aria-label="Emoji: Rightwards arrow">FENa > 3%. https://abs.twimg.com/emoji/v2/... draggable="false" alt="🚨" title="Police cars revolving light" aria-label="Emoji: Police cars revolving light">Patchy tubular, glomerular and vascular disease can cause falsely low FENa thus is a poor predictor of fluid responsiveness." class="img-responsive" style="max-width:100%;"/>
FENa: Hypovolemia + normal tubular function should lead to https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">Na reabsorption and a FENa < 1%. Tubular injury https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Rightwards arrow" aria-label="Emoji: Rightwards arrow"> inappropriate Na wasting https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Rightwards arrow" aria-label="Emoji: Rightwards arrow">FENa > 3%. https://abs.twimg.com/emoji/v2/... draggable="false" alt="🚨" title="Police cars revolving light" aria-label="Emoji: Police cars revolving light">Patchy tubular, glomerular and vascular disease can cause falsely low FENa thus is a poor predictor of fluid responsiveness." title="https://abs.twimg.com/emoji/v2/... draggable="false" alt="1⃣" title="Keycap digit one" aria-label="Emoji: Keycap digit one">FENa: Hypovolemia + normal tubular function should lead to https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">Na reabsorption and a FENa < 1%. Tubular injury https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Rightwards arrow" aria-label="Emoji: Rightwards arrow"> inappropriate Na wasting https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Rightwards arrow" aria-label="Emoji: Rightwards arrow">FENa > 3%. https://abs.twimg.com/emoji/v2/... draggable="false" alt="🚨" title="Police cars revolving light" aria-label="Emoji: Police cars revolving light">Patchy tubular, glomerular and vascular disease can cause falsely low FENa thus is a poor predictor of fluid responsiveness." class="img-responsive" style="max-width:100%;"/>
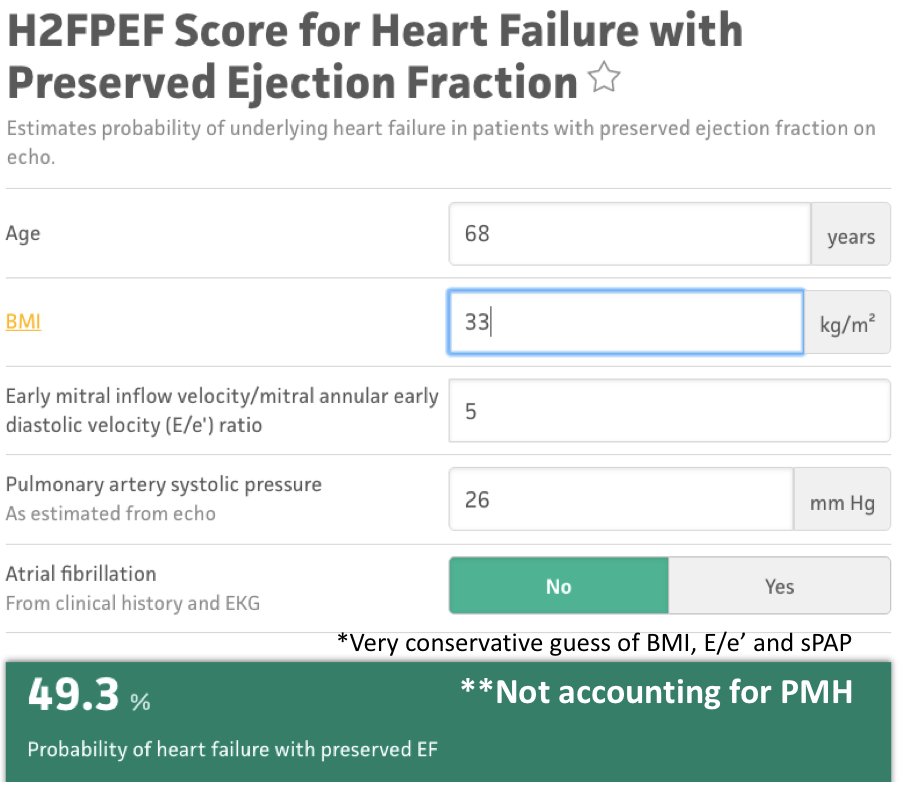 Evaluation of "volume status" using traditional clinical exam is not reliable. Hx of poor oral intake makes an empiric fluid challenge tempting. However some concerns in this case: Pt age, BMI and PMH (CAD, HTN, OSH, DM) put him at increased risk of having preexisting HFpEF" title="https://abs.twimg.com/emoji/v2/... draggable="false" alt="2⃣" title="Keycap digit two" aria-label="Emoji: Keycap digit two">Evaluation of "volume status" using traditional clinical exam is not reliable. Hx of poor oral intake makes an empiric fluid challenge tempting. However some concerns in this case: Pt age, BMI and PMH (CAD, HTN, OSH, DM) put him at increased risk of having preexisting HFpEF" class="img-responsive" style="max-width:100%;"/>
Evaluation of "volume status" using traditional clinical exam is not reliable. Hx of poor oral intake makes an empiric fluid challenge tempting. However some concerns in this case: Pt age, BMI and PMH (CAD, HTN, OSH, DM) put him at increased risk of having preexisting HFpEF" title="https://abs.twimg.com/emoji/v2/... draggable="false" alt="2⃣" title="Keycap digit two" aria-label="Emoji: Keycap digit two">Evaluation of "volume status" using traditional clinical exam is not reliable. Hx of poor oral intake makes an empiric fluid challenge tempting. However some concerns in this case: Pt age, BMI and PMH (CAD, HTN, OSH, DM) put him at increased risk of having preexisting HFpEF" class="img-responsive" style="max-width:100%;"/>
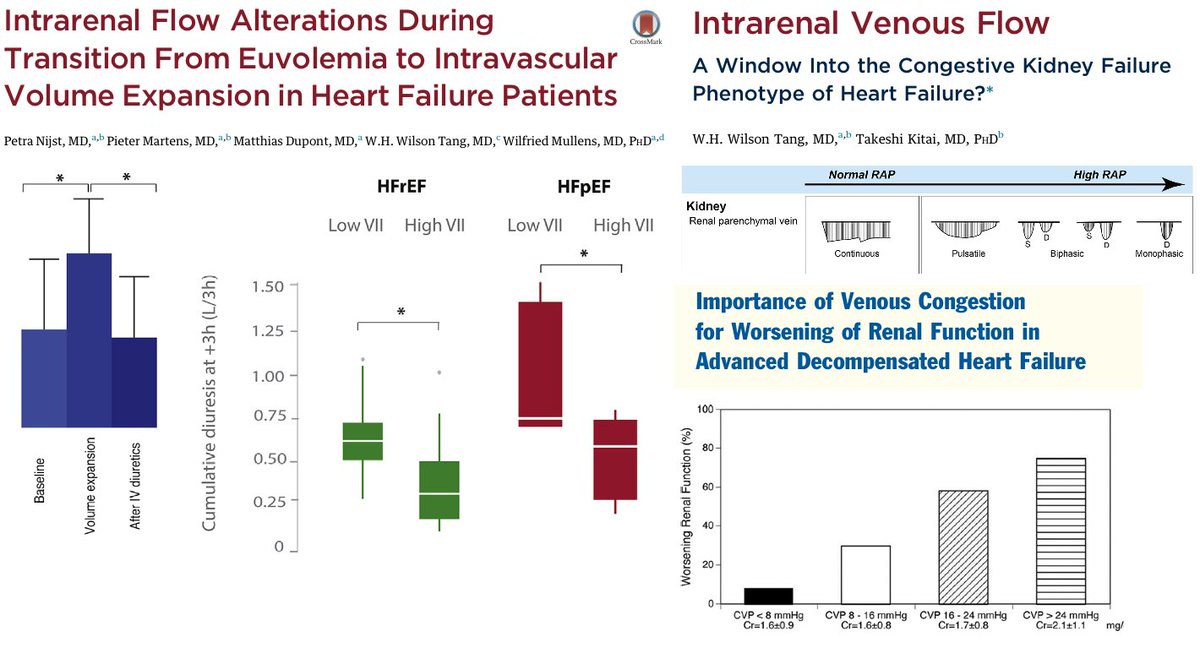 " title="Infusing 1 L of HES to patients with compensated HFpEF altered intra-renal venous flow and this induced diuretic resistance. Increased CVP and alterations of IRVF have been linked to worsening renal function (Renosarca). ARDS / Sepsis is already a sign of poor volume tolerancehttps://abs.twimg.com/emoji/v2/... draggable="false" alt="🚨" title="Police cars revolving light" aria-label="Emoji: Police cars revolving light">">
" title="Infusing 1 L of HES to patients with compensated HFpEF altered intra-renal venous flow and this induced diuretic resistance. Increased CVP and alterations of IRVF have been linked to worsening renal function (Renosarca). ARDS / Sepsis is already a sign of poor volume tolerancehttps://abs.twimg.com/emoji/v2/... draggable="false" alt="🚨" title="Police cars revolving light" aria-label="Emoji: Police cars revolving light">">
 " title="Infusing 1 L of HES to patients with compensated HFpEF altered intra-renal venous flow and this induced diuretic resistance. Increased CVP and alterations of IRVF have been linked to worsening renal function (Renosarca). ARDS / Sepsis is already a sign of poor volume tolerancehttps://abs.twimg.com/emoji/v2/... draggable="false" alt="🚨" title="Police cars revolving light" aria-label="Emoji: Police cars revolving light">">
" title="Infusing 1 L of HES to patients with compensated HFpEF altered intra-renal venous flow and this induced diuretic resistance. Increased CVP and alterations of IRVF have been linked to worsening renal function (Renosarca). ARDS / Sepsis is already a sign of poor volume tolerancehttps://abs.twimg.com/emoji/v2/... draggable="false" alt="🚨" title="Police cars revolving light" aria-label="Emoji: Police cars revolving light">">
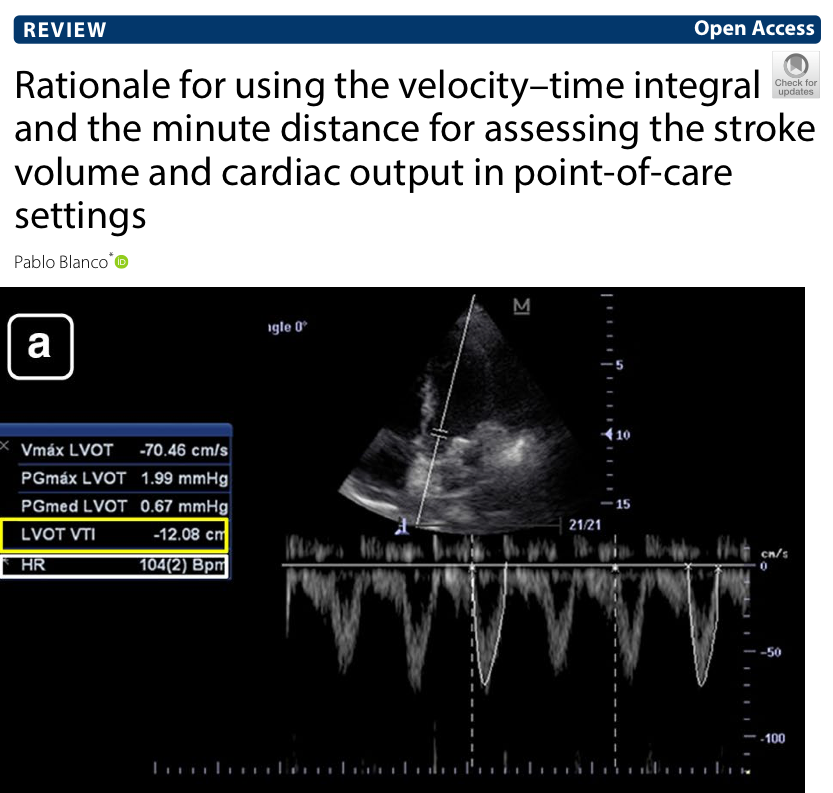 stroke volume. If stroke volume is normal/high, fluids make no sense! This can be measured easily!" title="Ideally you would want to know if patient will respond to fluids before giving them. This is hard to do on the ED. However, the reason to give fluids would be to increase https://abs.twimg.com/emoji/v2/... draggable="false" alt="♥️" title="Heart suit" aria-label="Emoji: Heart suit">stroke volume. If stroke volume is normal/high, fluids make no sense! This can be measured easily!" class="img-responsive" style="max-width:100%;"/>
stroke volume. If stroke volume is normal/high, fluids make no sense! This can be measured easily!" title="Ideally you would want to know if patient will respond to fluids before giving them. This is hard to do on the ED. However, the reason to give fluids would be to increase https://abs.twimg.com/emoji/v2/... draggable="false" alt="♥️" title="Heart suit" aria-label="Emoji: Heart suit">stroke volume. If stroke volume is normal/high, fluids make no sense! This can be measured easily!" class="img-responsive" style="max-width:100%;"/>

 show https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">incidence of hematuria and proteinuria (as in this patient). Autopsies show tubular necrosis, obstruction of peritubular capillary lumens and glomerular capillary loops. Today @NEJM published convincing evidence of #SARSCov2 directly involving the kidney!" title="Reports from https://abs.twimg.com/emoji/v2/... draggable="false" alt="🇨🇳" title="Flag of China" aria-label="Emoji: Flag of China"> show https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">incidence of hematuria and proteinuria (as in this patient). Autopsies show tubular necrosis, obstruction of peritubular capillary lumens and glomerular capillary loops. Today @NEJM published convincing evidence of #SARSCov2 directly involving the kidney!" class="img-responsive" style="max-width:100%;"/>
show https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">incidence of hematuria and proteinuria (as in this patient). Autopsies show tubular necrosis, obstruction of peritubular capillary lumens and glomerular capillary loops. Today @NEJM published convincing evidence of #SARSCov2 directly involving the kidney!" title="Reports from https://abs.twimg.com/emoji/v2/... draggable="false" alt="🇨🇳" title="Flag of China" aria-label="Emoji: Flag of China"> show https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">incidence of hematuria and proteinuria (as in this patient). Autopsies show tubular necrosis, obstruction of peritubular capillary lumens and glomerular capillary loops. Today @NEJM published convincing evidence of #SARSCov2 directly involving the kidney!" class="img-responsive" style="max-width:100%;"/>