As most states begin to reopen, we should remember that while there are some signs of hope and improvement, this pandemic is still far from over. (1/24)
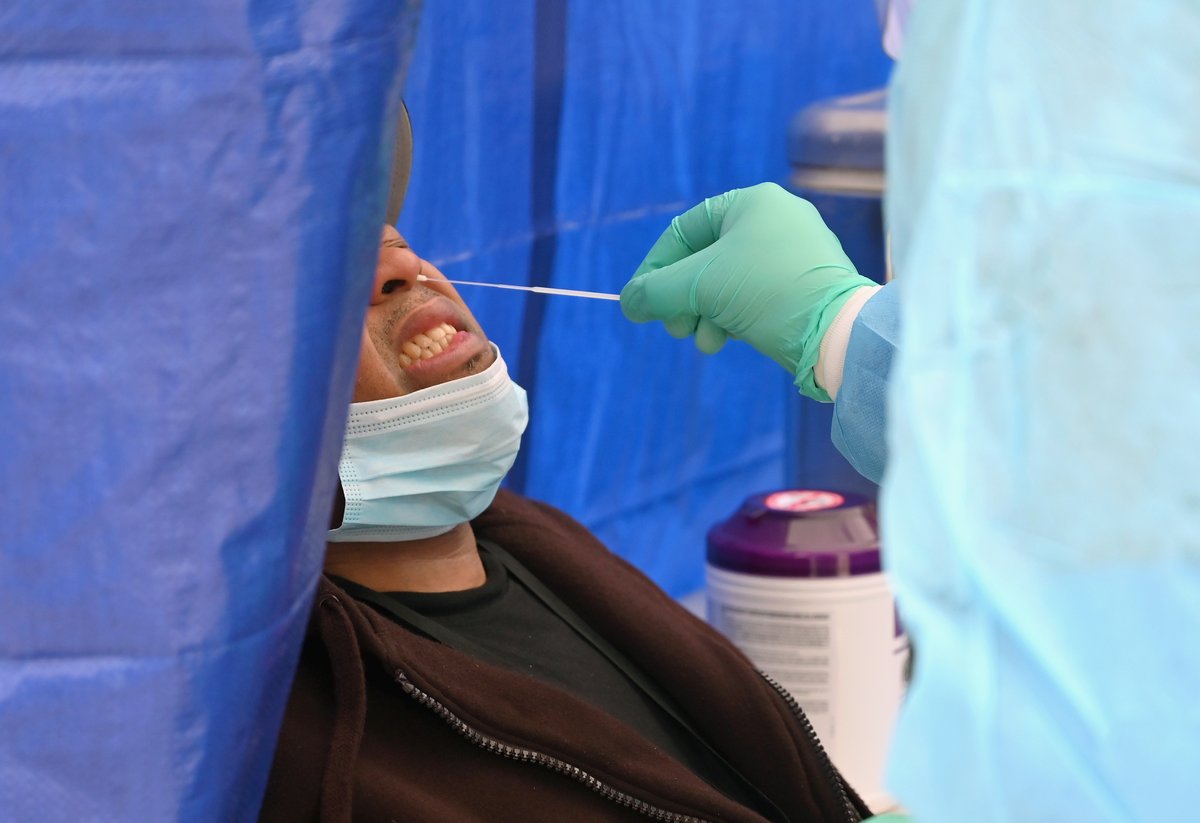
Public health experts have stressed repeatedly that the safest way to begin reopening the country is to test, test, test. But, you may be wondering: what does that mean? How many tests? How frequently? And, how reliable are they anyway? (2/24) https://cnn.it/2ST3tCZ ">https://cnn.it/2ST3tCZ&q...
As far as how many tests are required, numbers are all over the place. A team at the Harvard Global Health Institute says the US should be testing at least 900,000 people a day by May 15 if there is any hope of getting ahead of this pandemic. (3/24)
And according to Harvard’s “Roadmap to Pandemic Resilience,” we will need at least 5 million tests/day by early June and 20 million per day by early July. Yes, 20 mil/day. That’s roughly every American -- twice a month (4/24)
There is another way to approach the problem: don& #39;t worry about number of tests, but try instead to get below a 10% positivity rate. That happens when at least 9/10 people you test are negative. That usually means you are testing enough. (5/24)
But there’s another big problem that many Americans haven’t even heard about, and that’s the accuracy of the tests. Or, rather, the lack of accuracy. (6/24)
The FDA has already given emergency use authorization to more than 70 diagnostic tests for the coronavirus. Diagnostic tests help us identify people who are currently infected with the virus by looking for evidence of viral genes and proteins. (7/24)
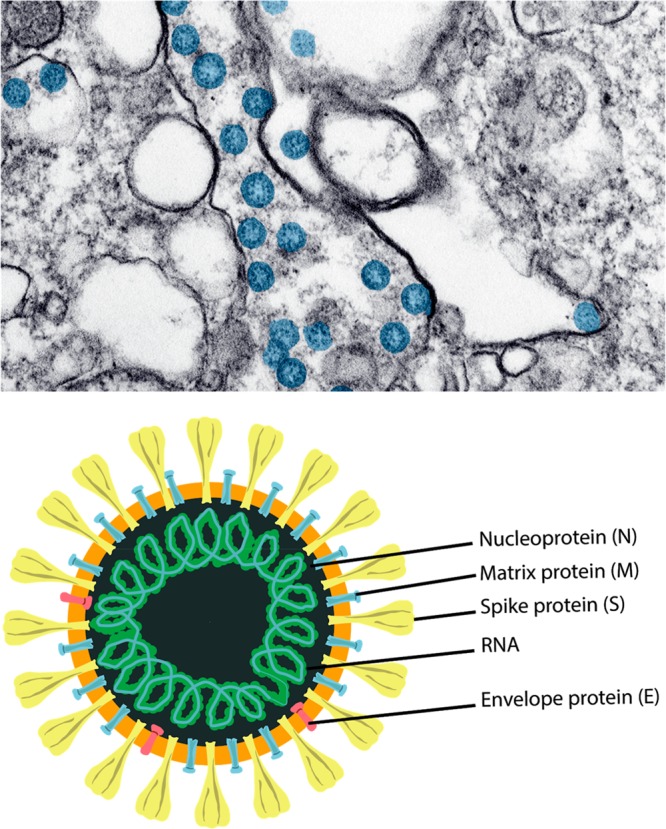
The most accurate of these tests has traditionally been the Reverse Transcription -- Polymerase Chain Reaction, or RT-PCR, test. These tests identify the presence of viral genes in your body through a process called amplification. (8/24)
RT-PCR detects whether or not viral RNA is present in samples from a patient. It does this by capturing and amplifying regions of the virus’ genetic material, usually the spike protein region. (9/24)
More specifically -- because this is an RNA virus, it must first be converted (or copied) to DNA. That’s what the RT part is of the test. The enzyme responsible for this is called reverse transcriptase. (10/24)
The PCR -- polymerase chain reaction -- then exposes the DNA to repeated temperature or thermal cycles to amplify the DNA into many copies, making it more easily detectable. (11/24)
Dr. Gary Procop, chief of virology at the Cleveland Clinic, recently checked out a batch of these tests used to diagnose Covid-19 patients. Most were 85-98% sensitive -- meaning that they picked up around 9 of 10 positive coronavirus samples. (12/24)
To understand what this means, it’s important to understand two technical terms: sensitivity and specificity. For this thread, I will focus on sensitivity. (13/24)
Read this next sentence a couple times. Sensitivity is the ability of a test to correctly generate a positive result for people who have the condition that’s being tested. In this case, being infected with the coronavirus. (14/24)
It is critical to know. Here’s why. If we take a test that is 90% sensitive and test 100 people who are infected, only 90 of the 100 will get a positive result. This means that an additional 10 people with the virus will think they are negative, even though they are not. (15/24)
This has enormous consequences. Missing 10% of positive coronavirus patients in a hospital means that infected patients may accidentally be placed in a COVID negative part of the hospital, potentially creating a cluster. (16/24)
The same could happen in nursing homes, and even in the general public, as states start to reopen. (17/24)
By now you know asymptomatic people can spread this virus. And, if those same people also incorrectly believe they are negative, they may greatly amplify that spread, even if unintentionally. (18/24)
In general, RT-PCR tests tend to be more accurate than other types of tests, but they typically have to be sent to a lab for processing. That is why many hospitals, clinics and other locations have started using POC or point-of-care tests to obtain more rapid results.(19/24)
You have probably heard of the Abbott ID NOW Covid-19 test. It is a RT-PCR POC test. That is a Reverse Transcription Polymerase Chain Reaction, Point of Care test. Lots of terms, but now you know all of them! It can deliver results in minutes. (20/24)
But the test is far from perfect. Dr. Gary Procop, chief of virology at the Cleveland Clinic, evaluated the test and found that it had a sensitivity rate of 85%. That means a false negative rate of 15%. (21/24)
Abbott has warned the sensitivity of its test is impacted by the chemical used to hold the virus sample – known as viral transport media. (22/24)
In a statement, Abbott said “This method can reduce the sensitivity of the test through dilution, which can potentially lead to false negative results.” (23/24)
There are two other types of tests as well -- see my next thread for information on those. (24/24)

 Read on Twitter
Read on Twitter