Which of these patients has a more severe degree of venous congestion? #VExUS Thread  https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧵" title="Thread" aria-label="Emoji: Thread"> about the Portal Vein (1/17)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧵" title="Thread" aria-label="Emoji: Thread"> about the Portal Vein (1/17)
Video above shows IVC in short axis, long axis and diameter (from left to right)
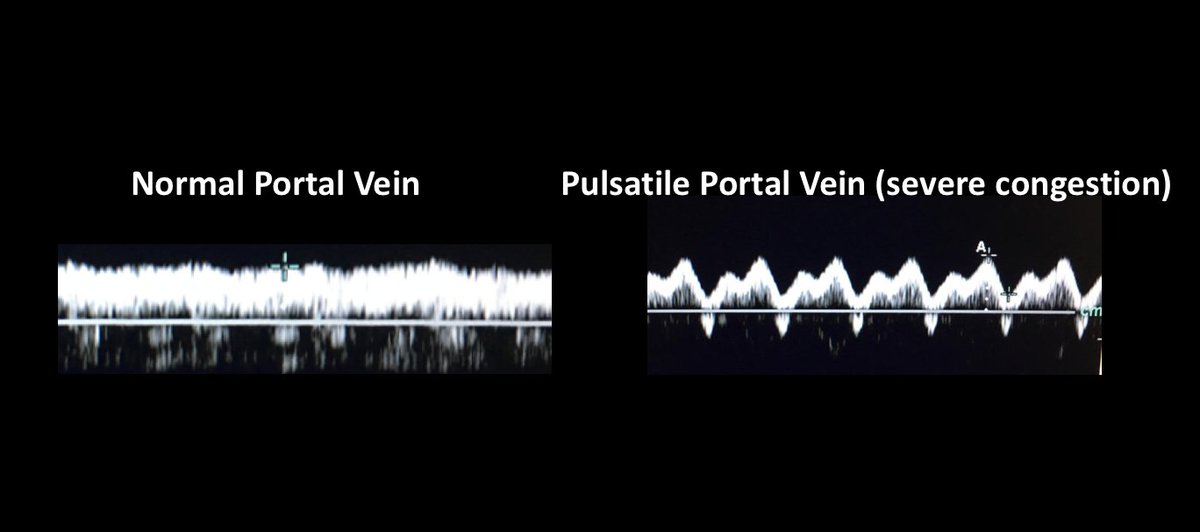
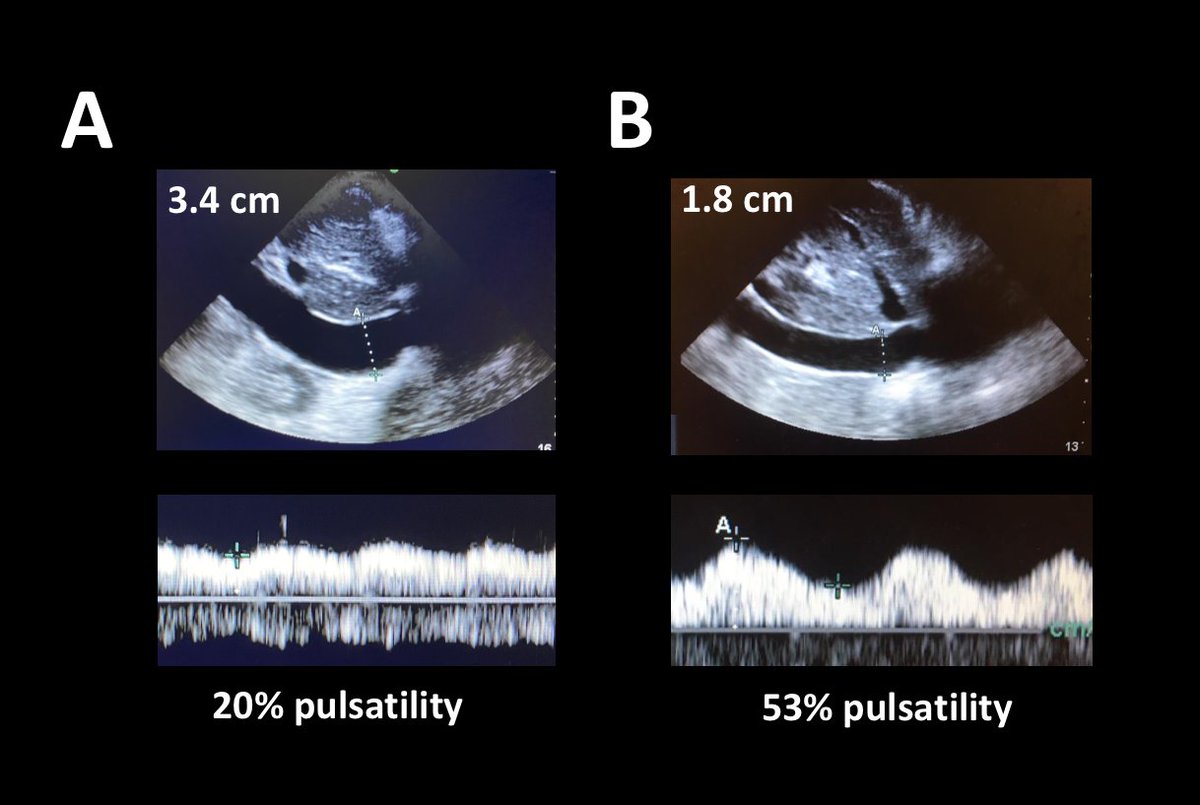
Which of these patients has a more severe degree of venous congestion? (2/17)
Which of these patients has a more severe degree of venous congestion? (2/17)
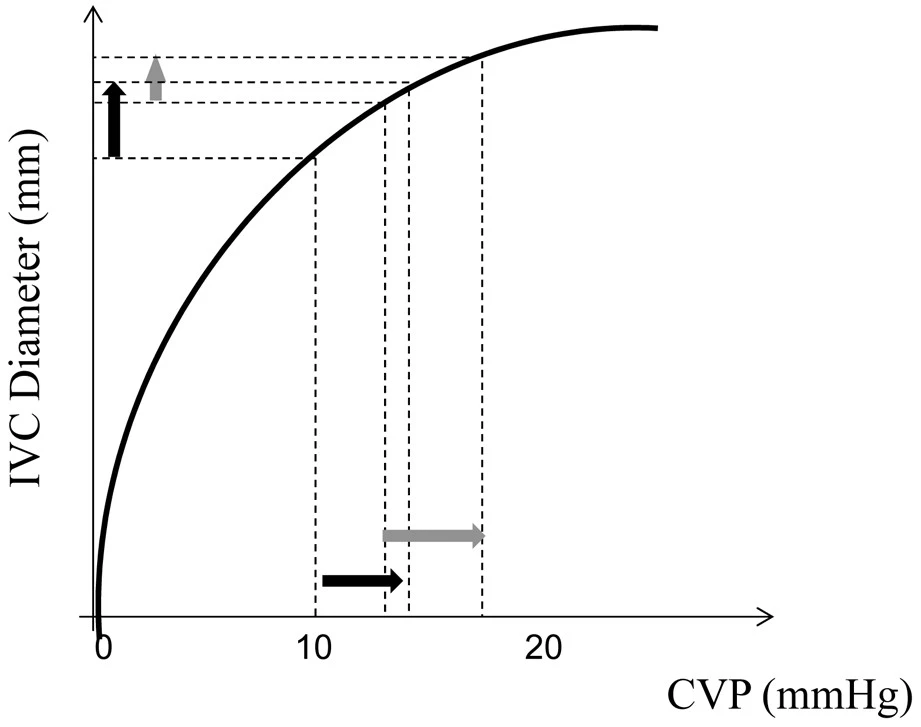
Abdominal IVC size depends on the difference between CVP and IAP. At a constant IAP, IVC size will increase proportionally to CVP until it reaches the flat part of it& #39;s compliance curve. (Great thread by @Thind888 here: https://twitter.com/Thind888/status/1249591199624769540?s=20)">https://twitter.com/Thind888/... (3/17)
A "stiff" IVC will reach it& #39;s max volume at a lower CVP. IVC remodelling can occur in patients with chronic RV failure and this pts can have a much larger IVC diameter without an equally large increase in CVP. So size isn& #39;t a really good indicator of severe congestion. (4/17)
Once IVC is fully distended, respiratory variations in size can be seen 2/2 acute changes in IAP and ITP. Increased inspiratory effort can lower ITP (or increase IAP) enough to collapse an IVC even at really high CVP (5/17) https://twitter.com/load_dependent/status/1126959142751690754?s=20">https://twitter.com/load_depe...
Looking at initial video it seems that both IVCs show very little inspiratory collapse. This suggests in both cases IVC has reached the flat part of its compliance, and CVP is always higher that IAP. However, this does not allow us to quantify the severity of congestion (6/17)
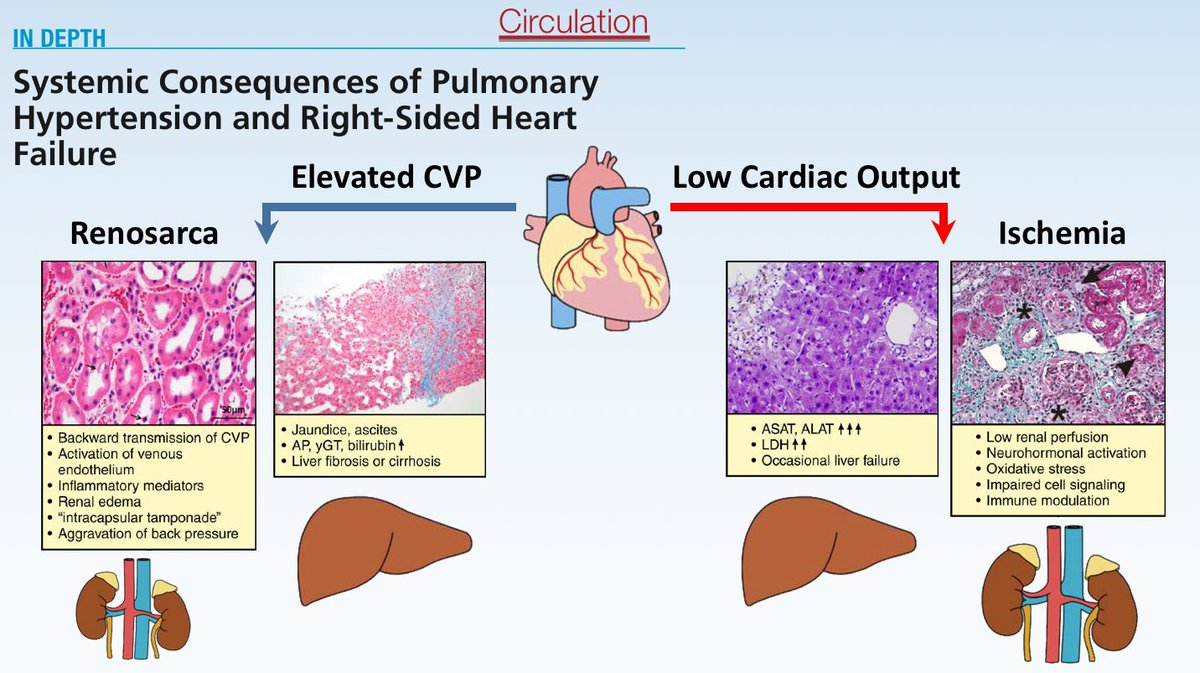
What we should really care about is the effect of congestion on tissues (Renosarca). So what you really want to do is estimate the degree of backwards transmission pressure from the CVP to the organs! (7/17)
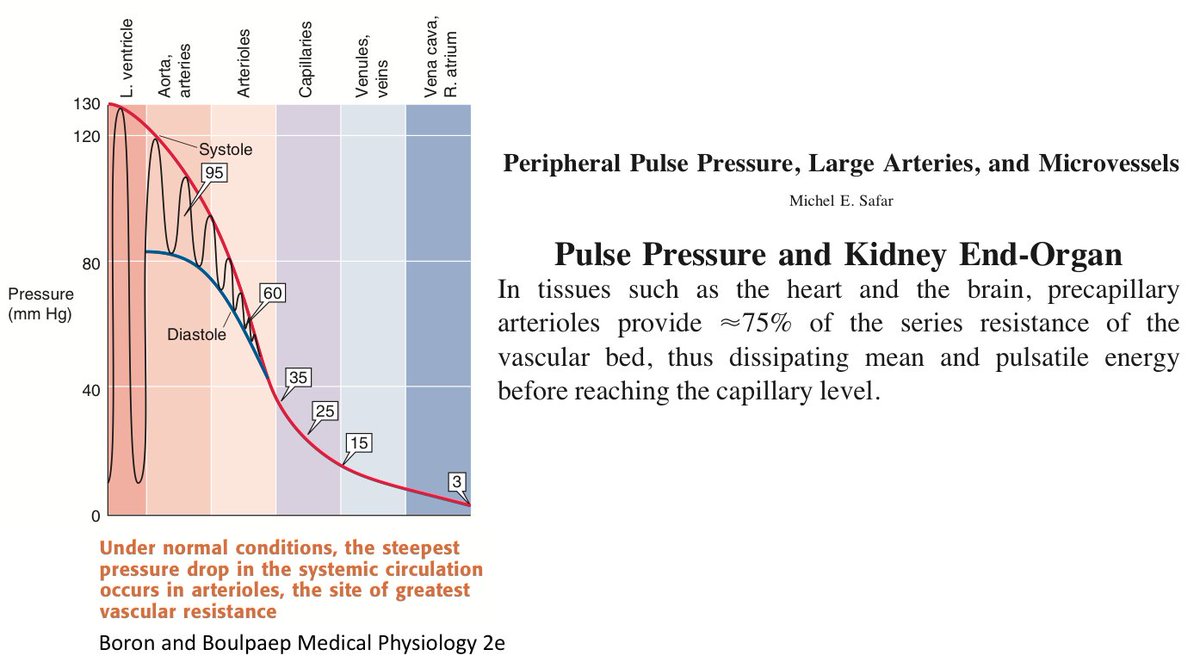
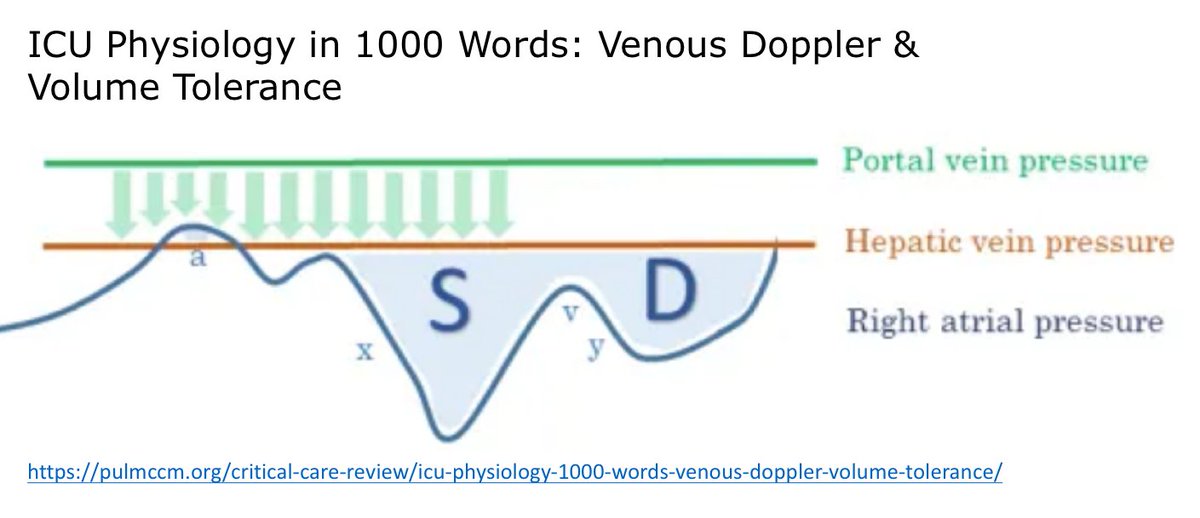
Blood vessel compliance serves a "pressure-buffering function". This is clearly the case of the aorta, buffering the highly pulsatile pressure generated by the beating heart. (8/17) https://twitter.com/thaiscoutinhoCV/status/1203393574609526786?s=20">https://twitter.com/thaiscout...
Pressure dissipation along the vascular tree is not only a function of compliance ("pressure cushion") but also of resistance. Aortic pulsatile pressure does not reach the capillaries mainly because of vascular resistance at the level of arterioles. (9/17)
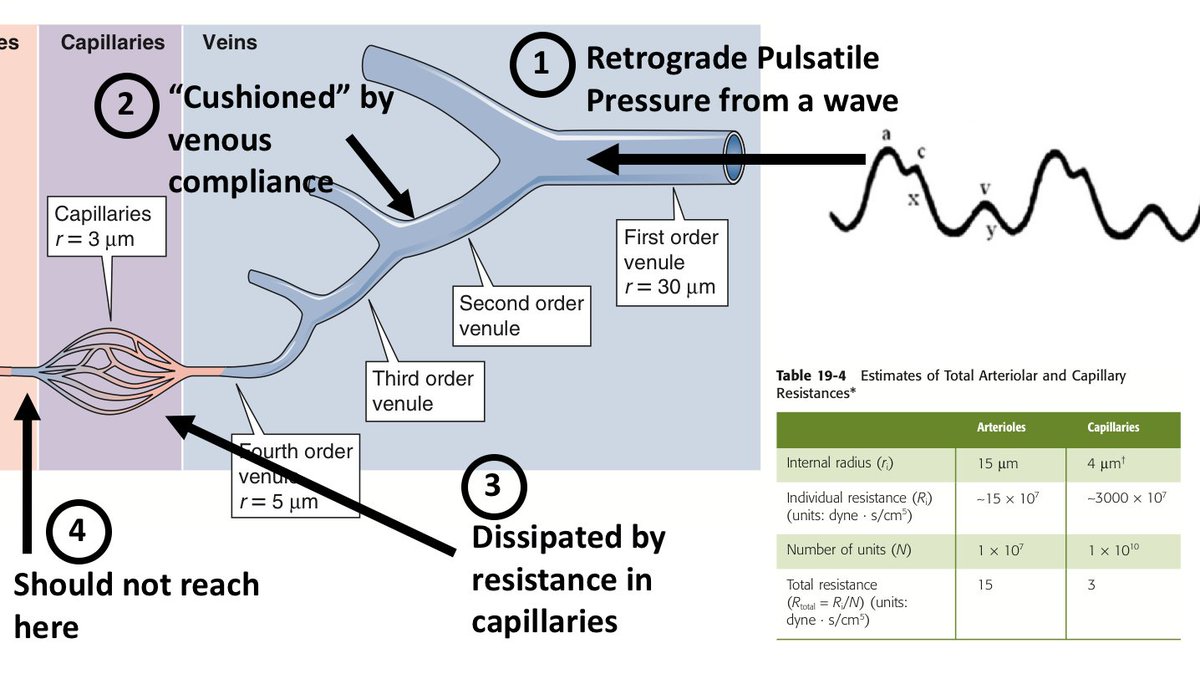
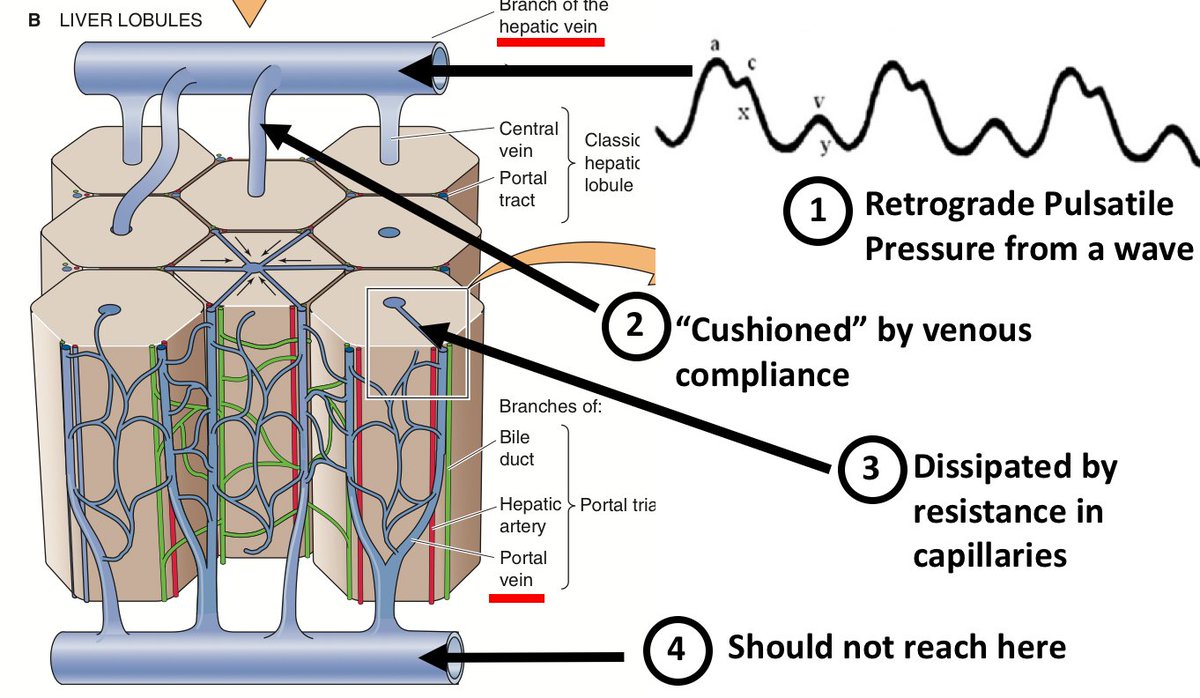
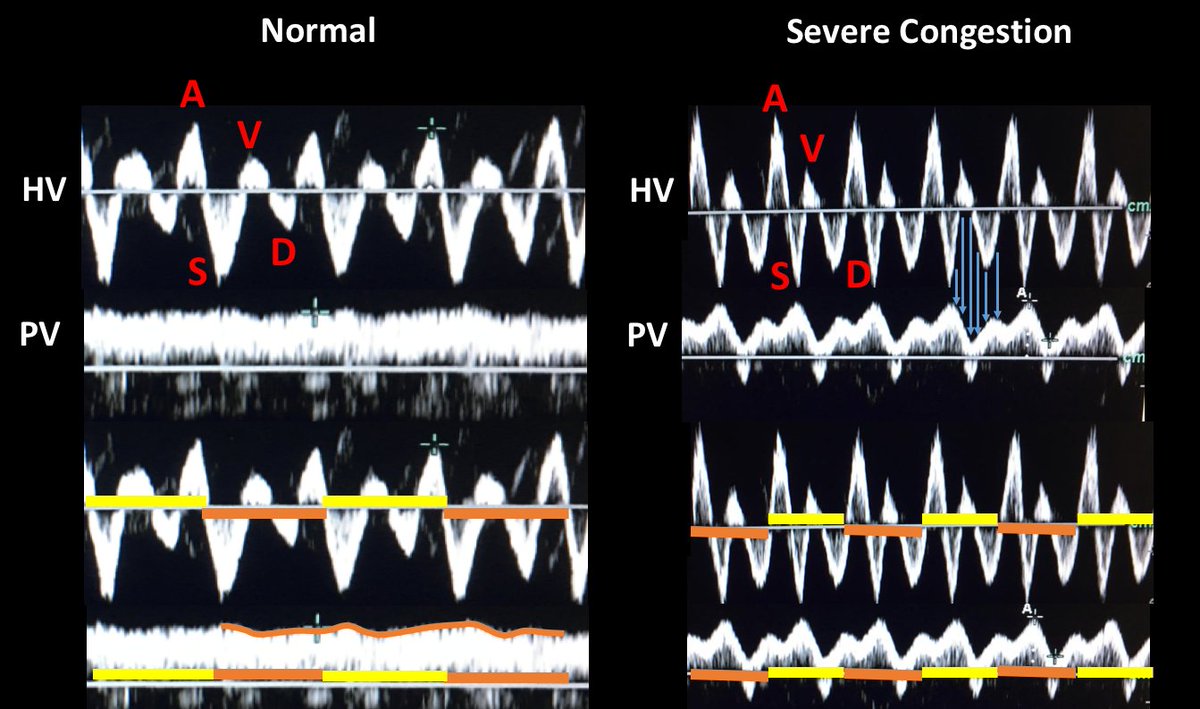
THE VENUS SIDE: During the normal cardiac cycle there are episodes of retrograde flow. In normal individuals this occurs during atrial systole (a wave). However, pathology including non-compliant RA can increase the amplitude of the V wave. TR can create a large cv wave (10/17)
By the same token, retrograde flow from the right atrium should be "cushioned" by the compliance of IVC and large veins. Also, resistance at the level of capillaries should dissipate the pulsatile energy. (Capillaries offer about 1/3 the resistance of arterioles) (11/17)
Normally retrograde pulsatile pressure from the heart should not get past capillaries.  https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔑" title="Key" aria-label="Emoji: Key"> Pathologically increased retrograde pulsatile pressure may very well reach beyond.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔑" title="Key" aria-label="Emoji: Key"> Pathologically increased retrograde pulsatile pressure may very well reach beyond.  https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔑" title="Key" aria-label="Emoji: Key">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔑" title="Key" aria-label="Emoji: Key">
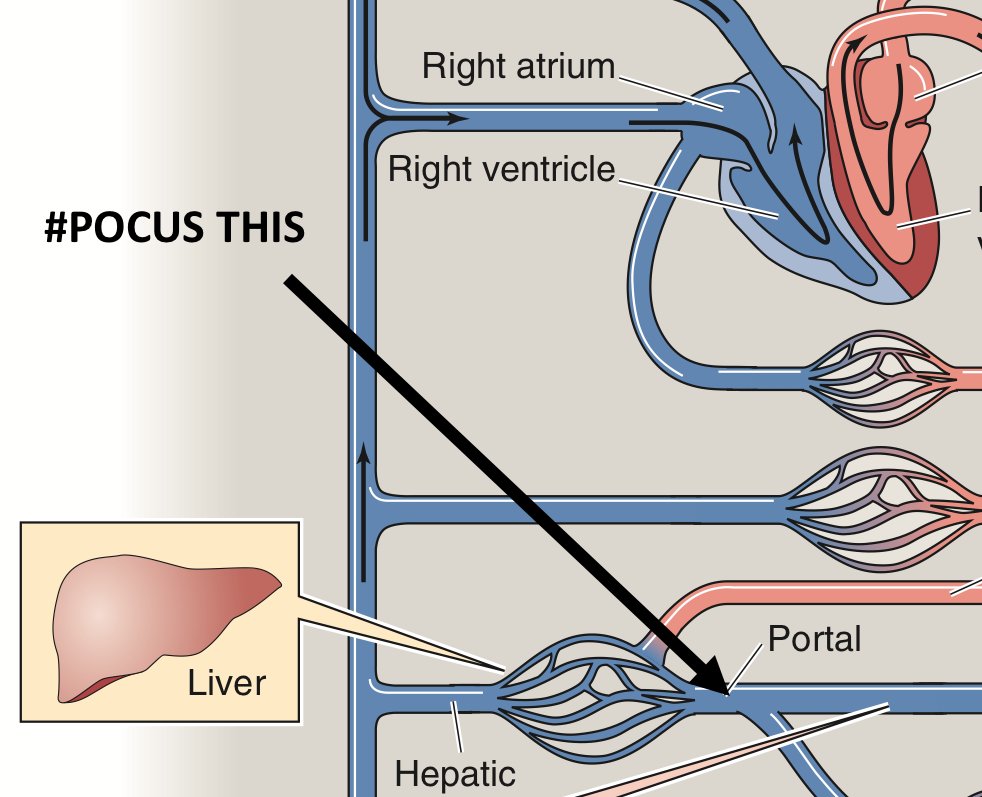
If we could only #POCUS some part of the body to know if this is happening.. (12/17)
If we could only #POCUS some part of the body to know if this is happening.. (12/17)
Enter the Portal Vein. Portal circulation allows us to interrogate flow in an easily scannable pre-capilary vein. Portal Vein Doppler is easy. Here is a video from @ThinkingCC on how to do it: https://thinkingcriticalcare.com/2020/02/28/a-vexus-mini-tutorial-foamed-pocus/">https://thinkingcriticalcare.com/2020/02/2... (13/17)
Normal portal vein flow is non pulsatile (monophasic). This in stark contrast with hepatic vein flow which basically reflects CVP pressure waveforms (pulsatile pressure in HV is not dissipated by capillary resistance, though vein and atrial compliance may "cushion" it) (14/17)
So back to the original question. These are the Portal Vein Dopplers from both patients. Patient B actually presented with congestive kidney injury that improved with diuretics. Patient A had WRF and hypotension, we lowered diuretic dose and Cr improved. (15/17)
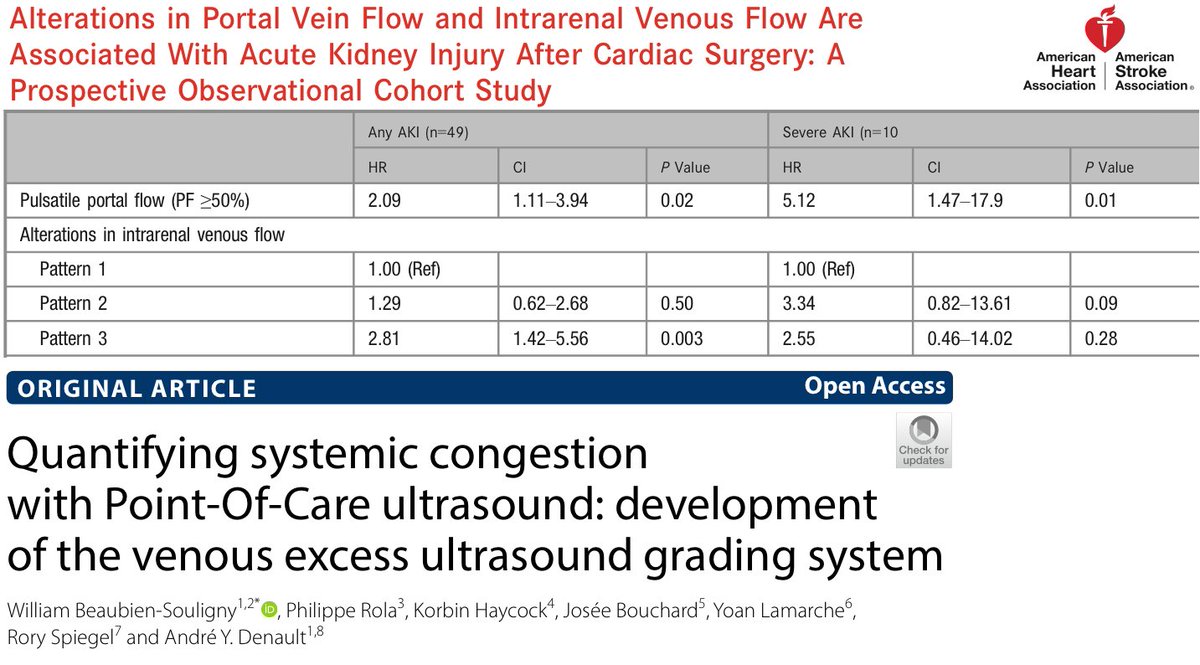
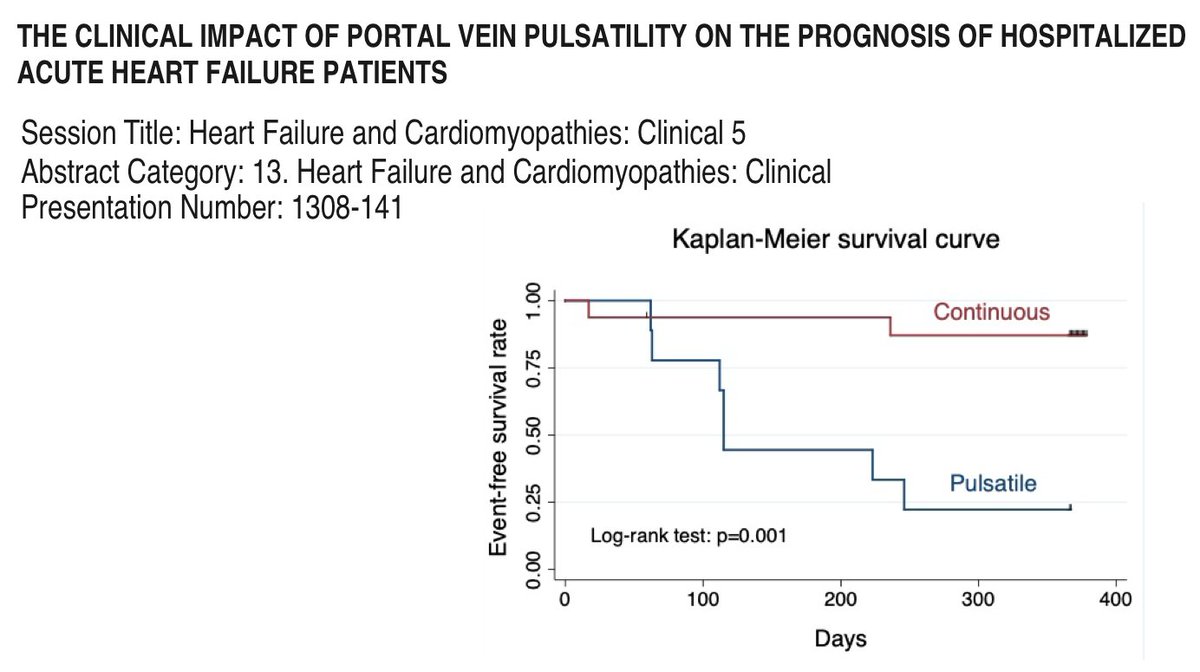
Portal Vein Pulsatility shows strong correlation with AKI in cardiac surgery patients. It has also been validated as a marker of RV disfunction. And it may also be an important prognostic factor in hospitalised heart failure patients. (16/17)
Understanding the origin of Portal Pulsatility also helps understand its mayor caveat: Cirrhosis.
Liver fibrosis increases resistance in capillary beds, so this should dissipate pulsatile pressure from the CVP. Indeed, this has been my experience https://twitter.com/ArgaizR/status/1226295108502511622?s=20">https://twitter.com/ArgaizR/s... (17/17)
Liver fibrosis increases resistance in capillary beds, so this should dissipate pulsatile pressure from the CVP. Indeed, this has been my experience https://twitter.com/ArgaizR/status/1226295108502511622?s=20">https://twitter.com/ArgaizR/s... (17/17)

 Read on Twitter
Read on Twitter