Increasing evidence points to monocytes and macrophages as key players in the maladaptive immune response to SARS-CoV-2 and the disease it causes, COVID-19. A thread with emphasis on key mechanisms of mononuclear phagocytic (MNP) activation and potential therapies.
What is the evidence that MNP cells, which includes monocytes and macrophages, are involved in COVID-19 pathogenesis? This review in @NatRevImmunol by @MiriamMerad and Jerome Martin from @IcahnMountSinai provides an excellent perspective. https://www.nature.com/articles/s41577-020-0331-4">https://www.nature.com/articles/...
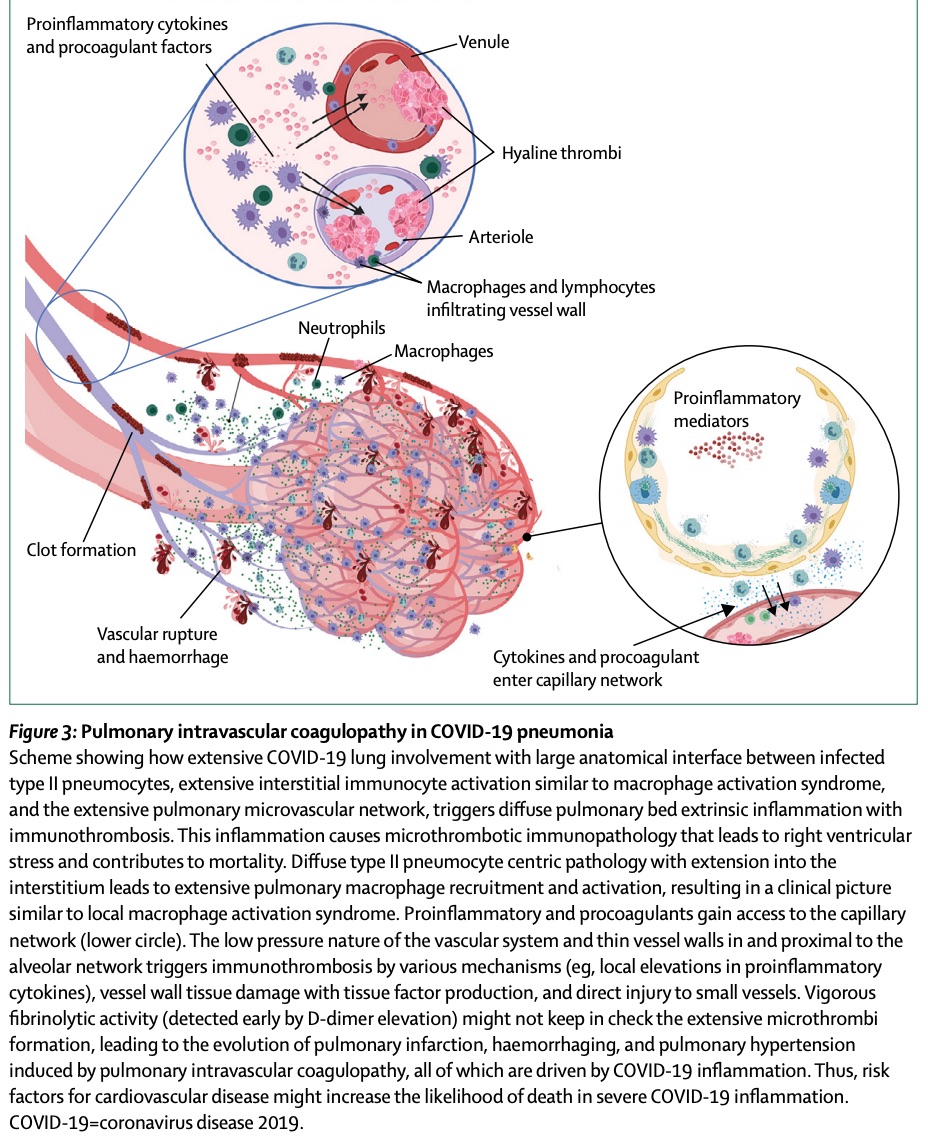
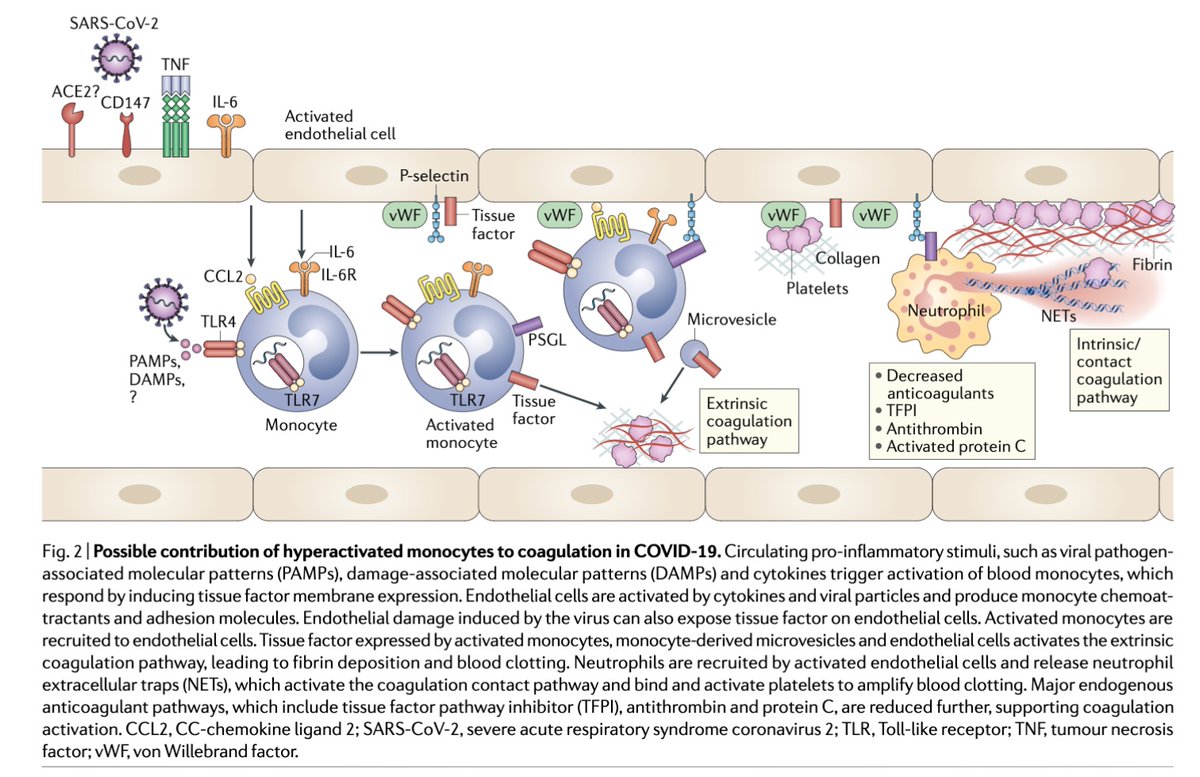
MNPs and are present in inflamed tissue such as the lungs, heart, and blood vessels. Here is a recent example in @TheLancet, which describes immune mechanisms of pulmonary intravascular coagulopathy in COVID-19 pneumonia. (More on clotting later.)
https://www.thelancet.com/journals/lanrhe/article/PIIS2665-9913(20)30121-1/fulltext#.XrbEk9zQTsY.twitter">https://www.thelancet.com/journals/...
https://www.thelancet.com/journals/lanrhe/article/PIIS2665-9913(20)30121-1/fulltext#.XrbEk9zQTsY.twitter">https://www.thelancet.com/journals/...
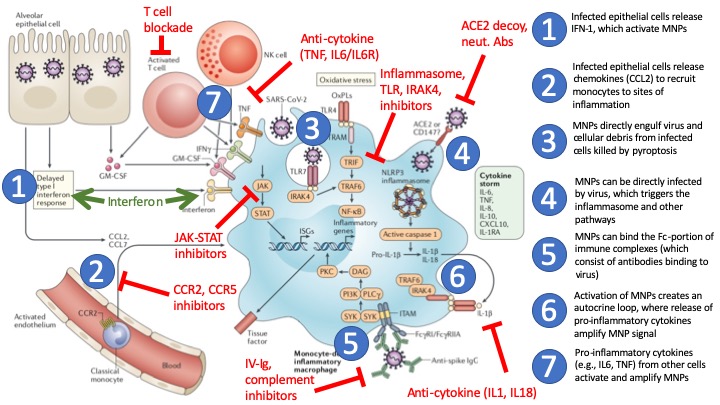
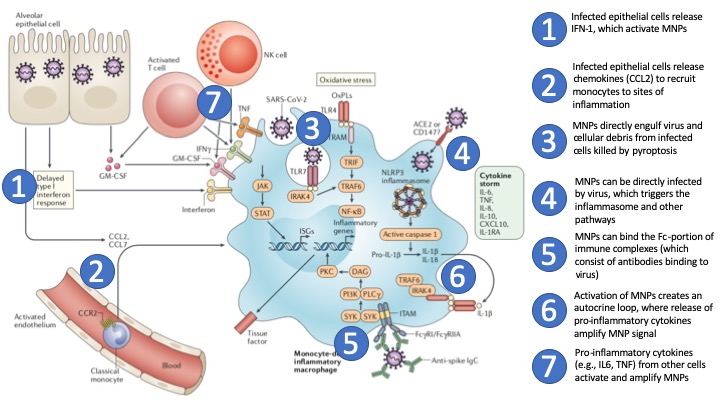
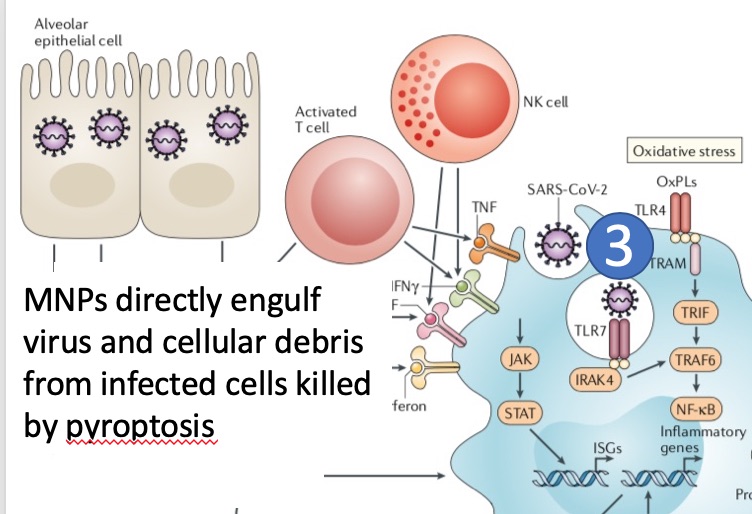
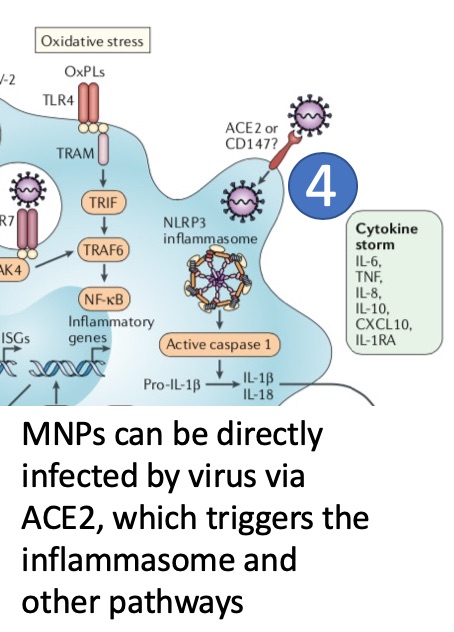
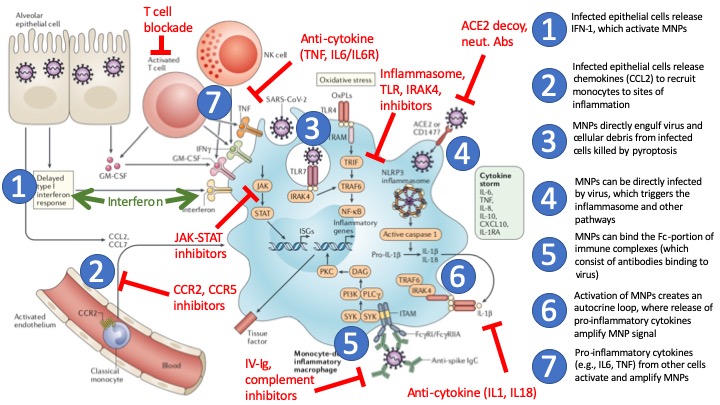
How might activation of MNPs occur in COVID-19? Here is where it gets tricky, as there are many mechanisms. I highlight seven mechanisms based on the @NatRevImmunol @MiriamMerad review. Let& #39;s go through each of them 1-by-1 with examples and potential therapies...
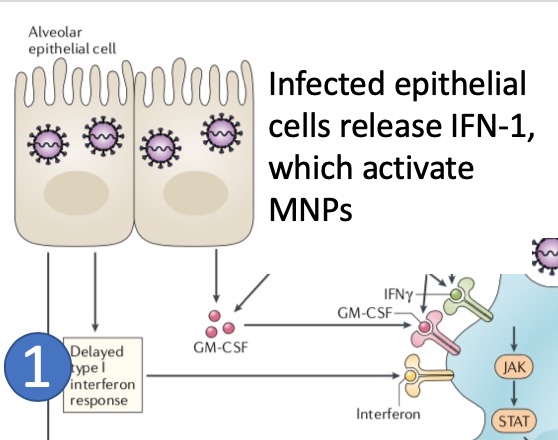
(1) Direct infection of lung cells by SARS-CoV-2 via ACE2 activates innate immune sensors and the release of type 1 interferons (IFNa, INFb), which can activate MNPs by binding to the IFN receptor.
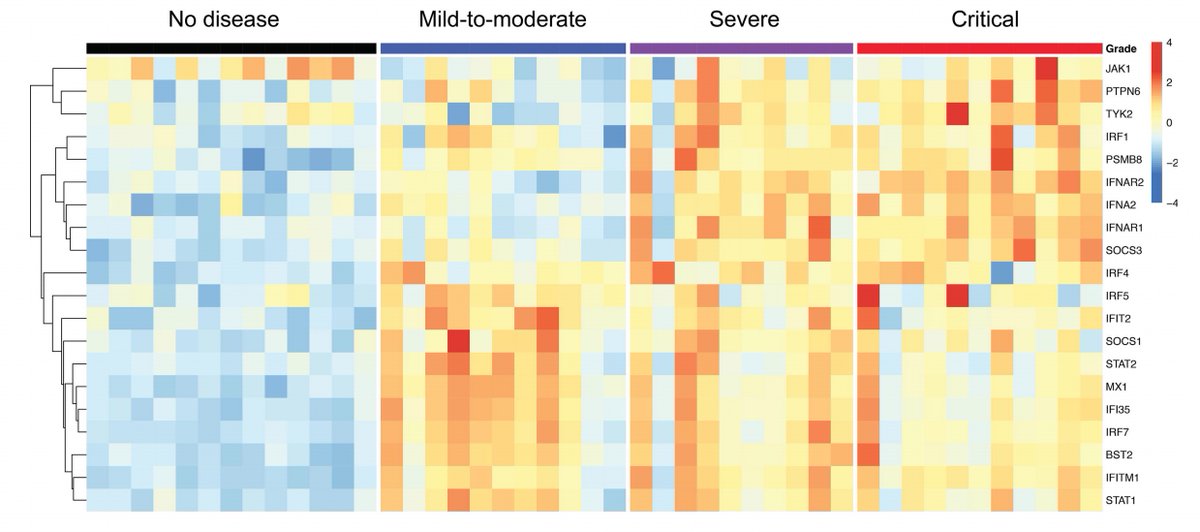
It is interesting to note that severe COVID-19 demonstrates impaired IFN-1 signatures as compared to mild or moderate cases, suggesting that IFN treatment may be beneficial.
https://www.medrxiv.org/content/10.1101/2020.04.19.20068015v1">https://www.medrxiv.org/content/1...
https://www.medrxiv.org/content/10.1101/2020.04.19.20068015v1">https://www.medrxiv.org/content/1...
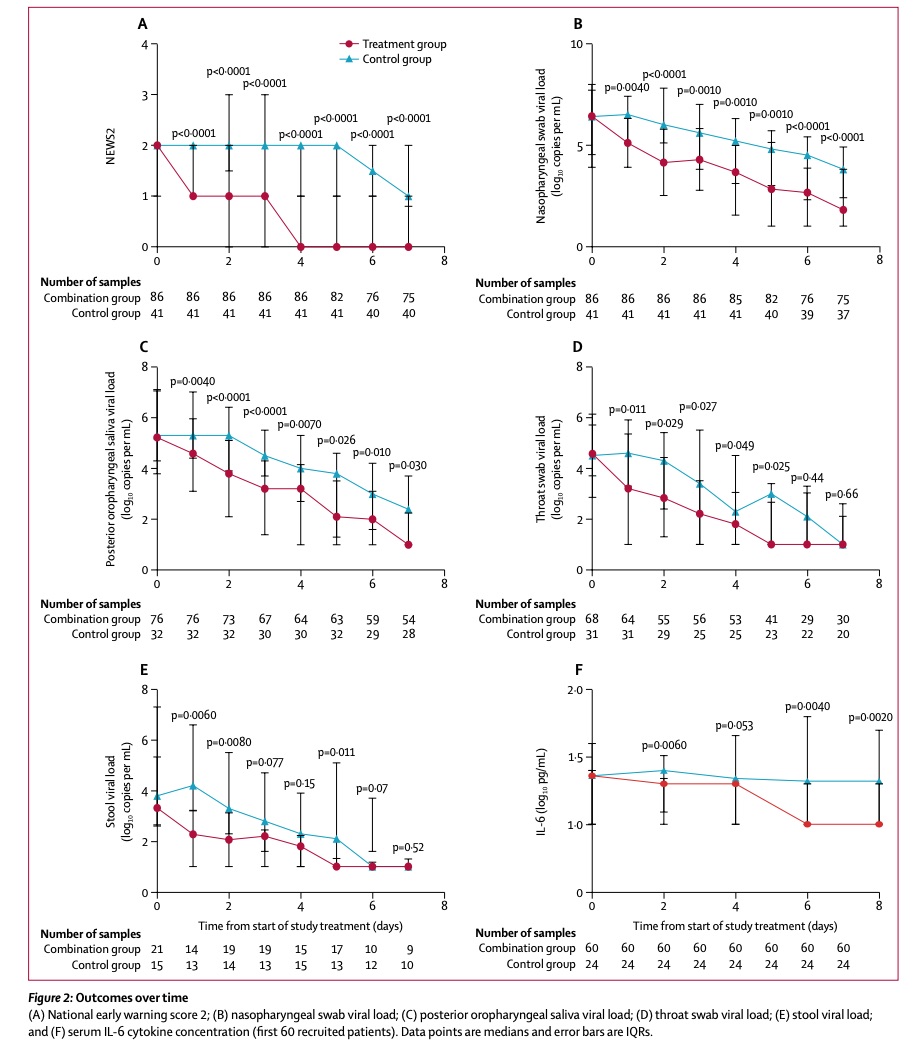
In an open-label, randomized Ph2 trial of n=127 COVID-19 patients, IFN-beta-1b (as part of triple therapy) was found to alleviate symptoms, shortening duration of viral shedding, and shorten hospital stay in mild/mod COVID-19 @TheLancet
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)31042-4/fulltext">https://www.thelancet.com/journals/...
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)31042-4/fulltext">https://www.thelancet.com/journals/...
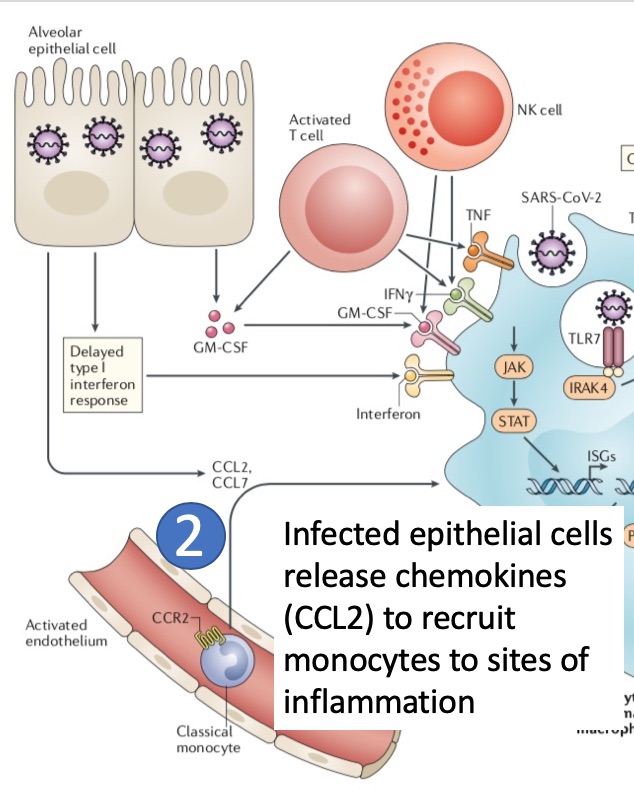
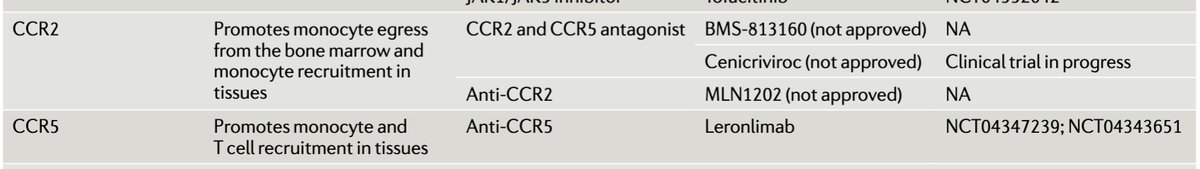
(2) Infected lung cells (eg., type 2 pneumocytes) release chemokines (e.g., CCL2) that bind to CCR2 on the surface of monocytes in blood and recruit these cells to sites of inflammation, where monocytes differentiate into macrophages.
Blockade of CCR2 (and CCR5) may block monocyte egress from the bone marrow and monocyte recruitment to inflammed tissues such as the lung. Trials are underway.
(3) MNPs can directly engulf virus and infected lung cells undergo pyroptosis (inflammatory cell death), leading to activation of MNPs.
Inflammasome/NLRP3 inhibitors may be effective in treating the maladaptive immune response in COVID-19, as suggested by @VirusesImmunity in this tweet https://twitter.com/VirusesImmunity/status/1246778158290014214">https://twitter.com/VirusesIm...
A recent study reported ACE2 and SARS-CoV-2 nucleocapsid protein is expressed in lymph nodes and spleen-associated CD169+ macrophages of COVID-19 patients producing IL-6.
https://www.medrxiv.org/content/10.1101/2020.03.27.20045427v1.full.pdf">https://www.medrxiv.org/content/1...
https://www.medrxiv.org/content/10.1101/2020.03.27.20045427v1.full.pdf">https://www.medrxiv.org/content/1...
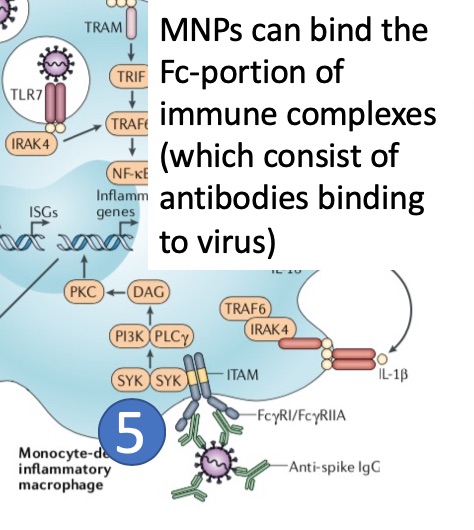
(5) Immune complexes form when antibodies bind SARS-CoV-2. The Fc portion of antibodies bind to receptors (FcR) on the surface of MNPs leading to activation of MNPs.
Antibody-dependent enhancement (ADE) is a concern when non-neutralizing antibodies bind to the virus and activate MNPs. See this informative thread by @angie_rasmussen https://twitter.com/angie_rasmussen/status/1234081358017966080">https://twitter.com/angie_ras...
Clinical trials are underway with intravenous immunoglobulin, or IVIG, in COVID-19. https://www.wsj.com/articles/researchers-explore-using-common-blood-plasma-treatment-to-fight-coronavirus-11588525200">https://www.wsj.com/articles/...
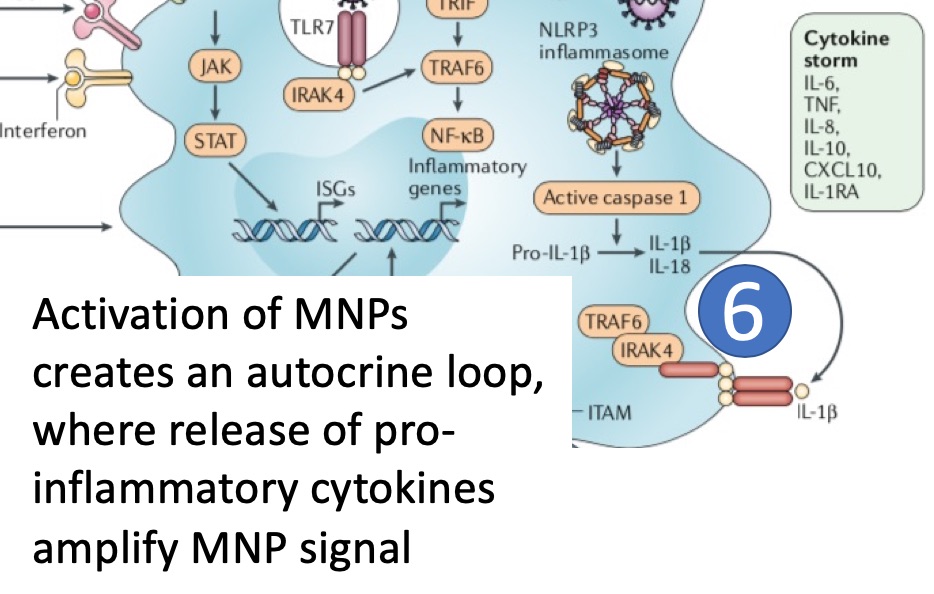
(6) Activated MNPs secrete pro-inflammatory cytokines, including IL-1b generated via the inflammasome pathway, which can create an autocrine loop amplifying MNP activation.
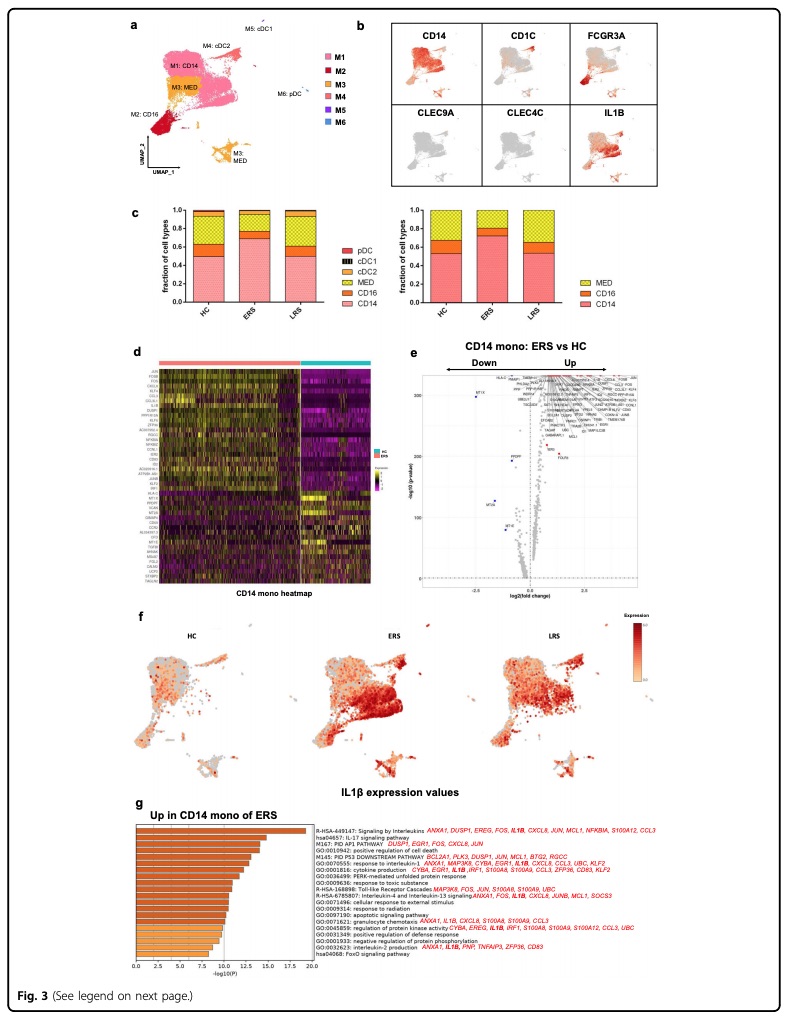
Single cell RNA-seq from peripheral blood in the early recovery stage of COVID-19 demonstrated an increased ratio of classical CD14++ monocytes with high inflammatory gene expression as well as a greater abundance of CD14++IL1β+ monocytes.
https://www.nature.com/articles/s41421-020-0168-9">https://www.nature.com/articles/...
https://www.nature.com/articles/s41421-020-0168-9">https://www.nature.com/articles/...
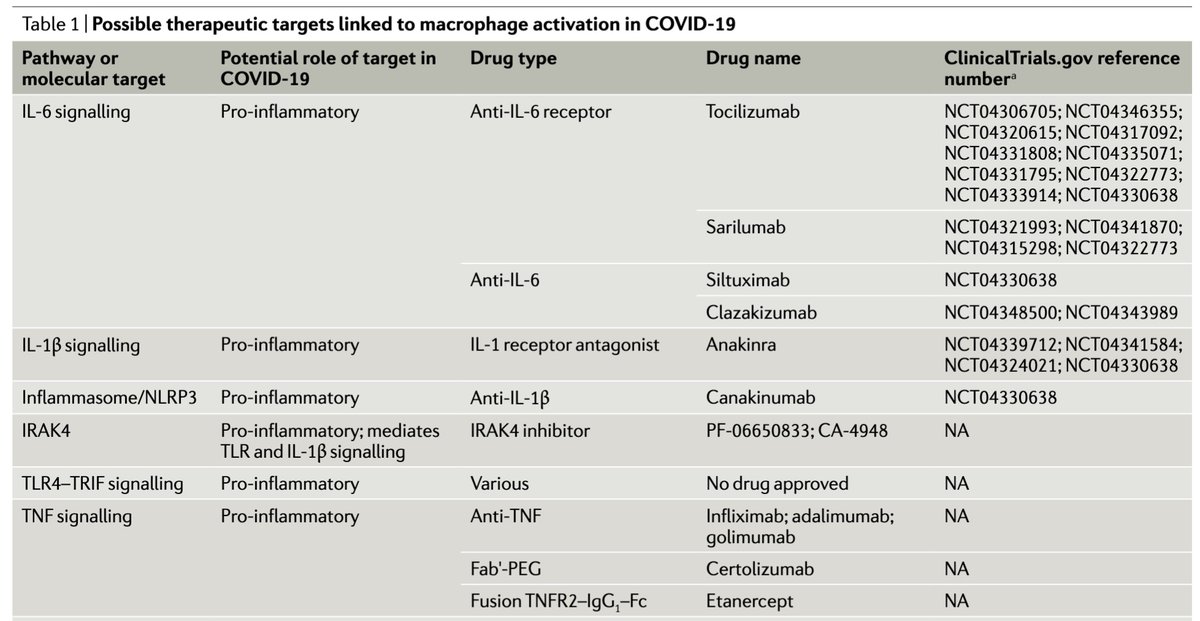
Clinical trials are underway with IL-1 receptor antagonists and antibodies to other inflammatory cytokines.
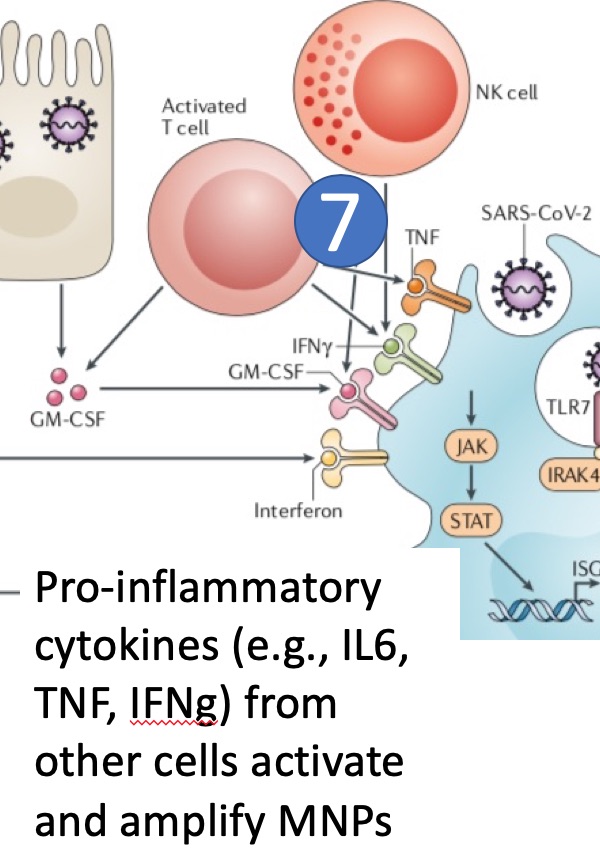
(7) Pro-inflammatory cytokines (e.g., IL-6, TNF-alpha, INF-gamma) from other cells (e.g., T cells, NK cells) activate and amplify MNPs. Anti-cytokine therapy and T cell modulators are being tested in COVID-19.
A recent retrospective study published in @JACCJournals described an association with anticoagulation treatment and survival among hospitalized patients with COVID-19. Randomized controlled trials are needed. http://www.onlinejacc.org/content/early/2020/05/05/j.jacc.2020.05.001">https://www.onlinejacc.org/content/e...

 Read on Twitter
Read on Twitter