COVID-19 literature updates covering two weeks 4/23-5/5 by @EricMeyerowitz and me
Recording: https://www.youtube.com/watch?v=PdofJOp_WAU
Slides:">https://www.youtube.com/watch... https://docs.google.com/presentation/d/1WkUarCvBOWq4k372fRr1cetC4qICjthHfRkNaGJqkW0/edit?usp=sharing
Key">https://docs.google.com/presentat... points and links to papers below
Recording: https://www.youtube.com/watch?v=PdofJOp_WAU
Slides:">https://www.youtube.com/watch... https://docs.google.com/presentation/d/1WkUarCvBOWq4k372fRr1cetC4qICjthHfRkNaGJqkW0/edit?usp=sharing
Key">https://docs.google.com/presentat... points and links to papers below
The Lancet published a blinded, placebo controlled RCT of remdesivir (RDV) from 10 hospitals in Wuhan. Patients were hypoxemic and within 12 days of symptom onset. Inclusion criteria were similar to NIH RDV trial
https://doi.org/10.1016/S0140-6736(20)31022-9">https://doi.org/10.1016/S...
https://doi.org/10.1016/S0140-6736(20)31022-9">https://doi.org/10.1016/S...
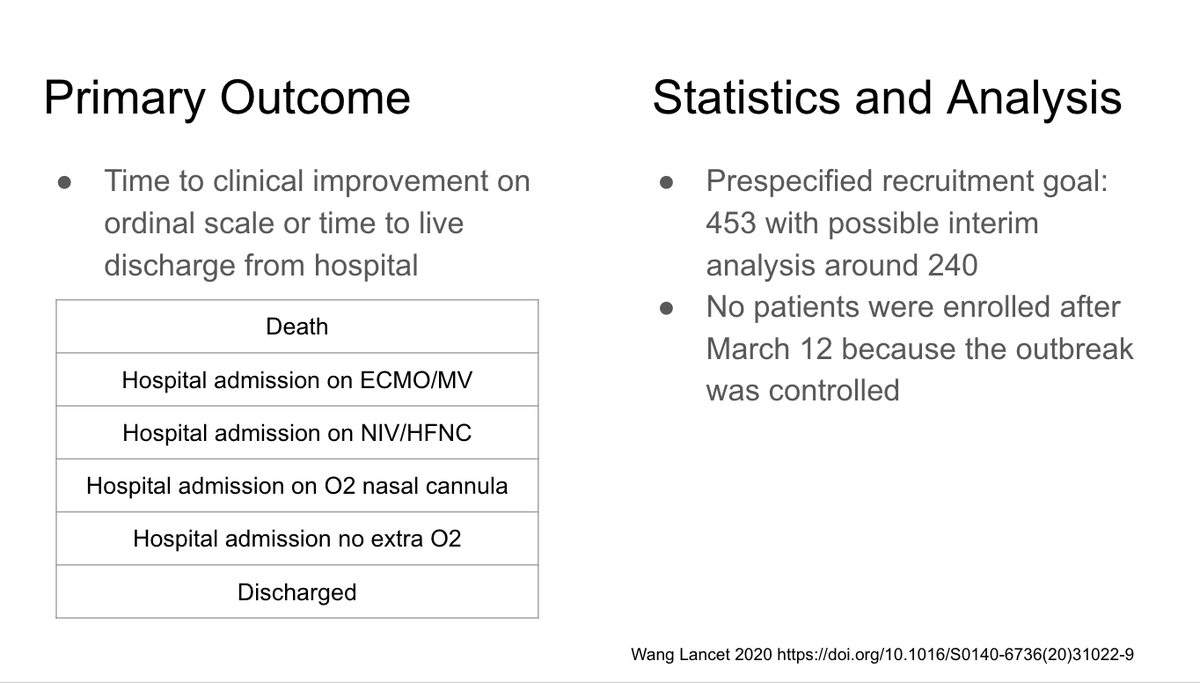
Primary outcome was time to clinical improvement (moving down 2 rungs on ladder of ordinal scale shown in this slide) or time to discharge. They had a prespecified recruitment goal of 453 but outbreak was controlled by March 12
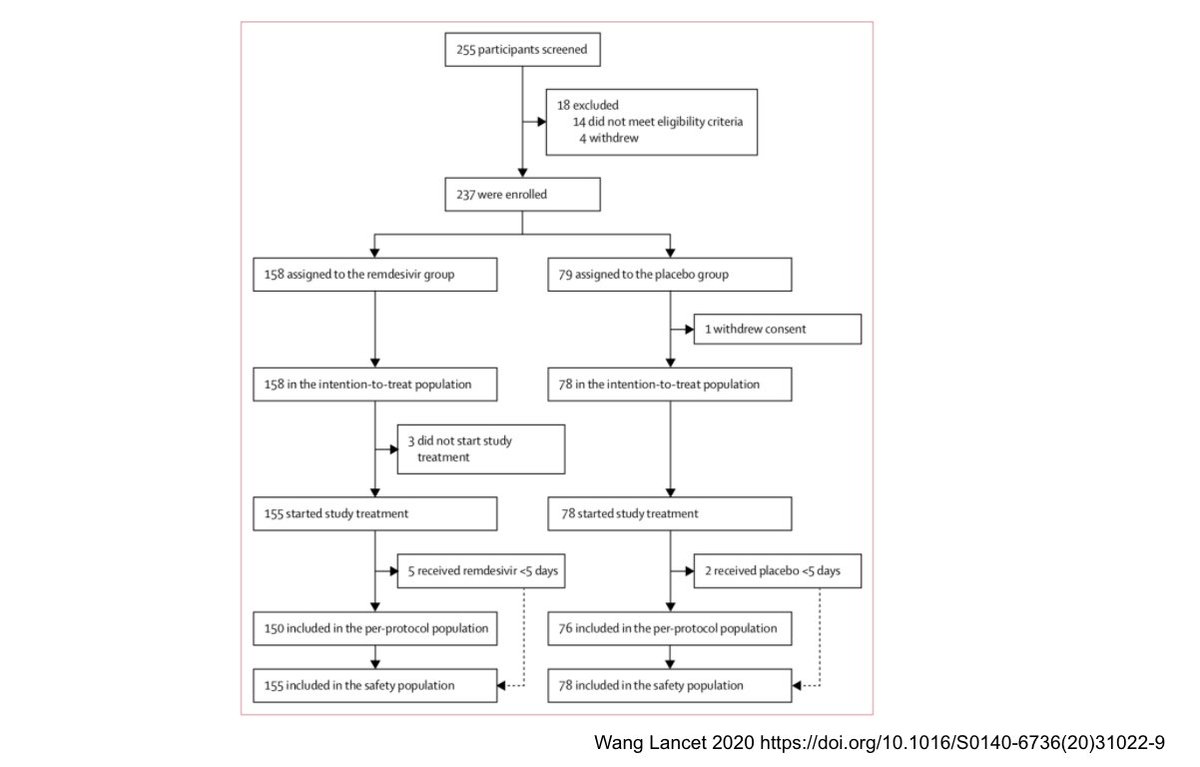
Enrollment scheme shown here. They ended up with 158 in the RDV arm and 78 in the placebo arm. They couldn’t enroll more because they had no more cases in Wuhan after March 12
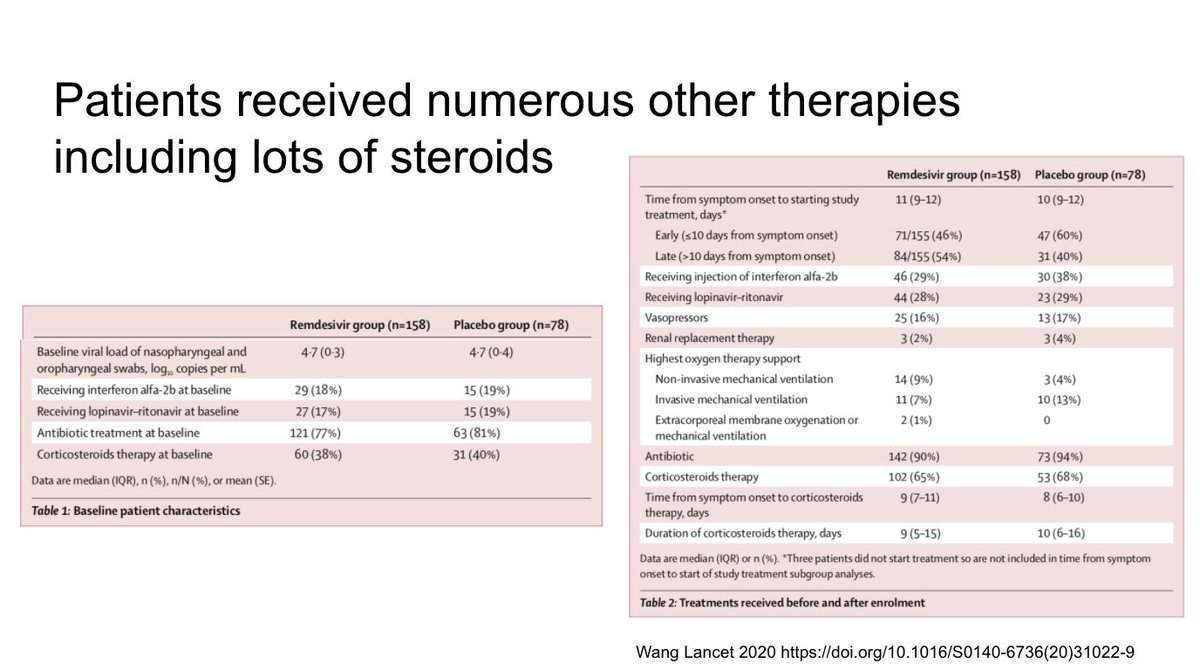
Left- baseline rx for each group: around 20% received interferon alpha and lopinavir/ritonavir and around 40% steroids. Right - more than 65% ended up receiving steroids. You can also see the percentages in each group who were “early” ie enrolled within 10 days of symptom onset
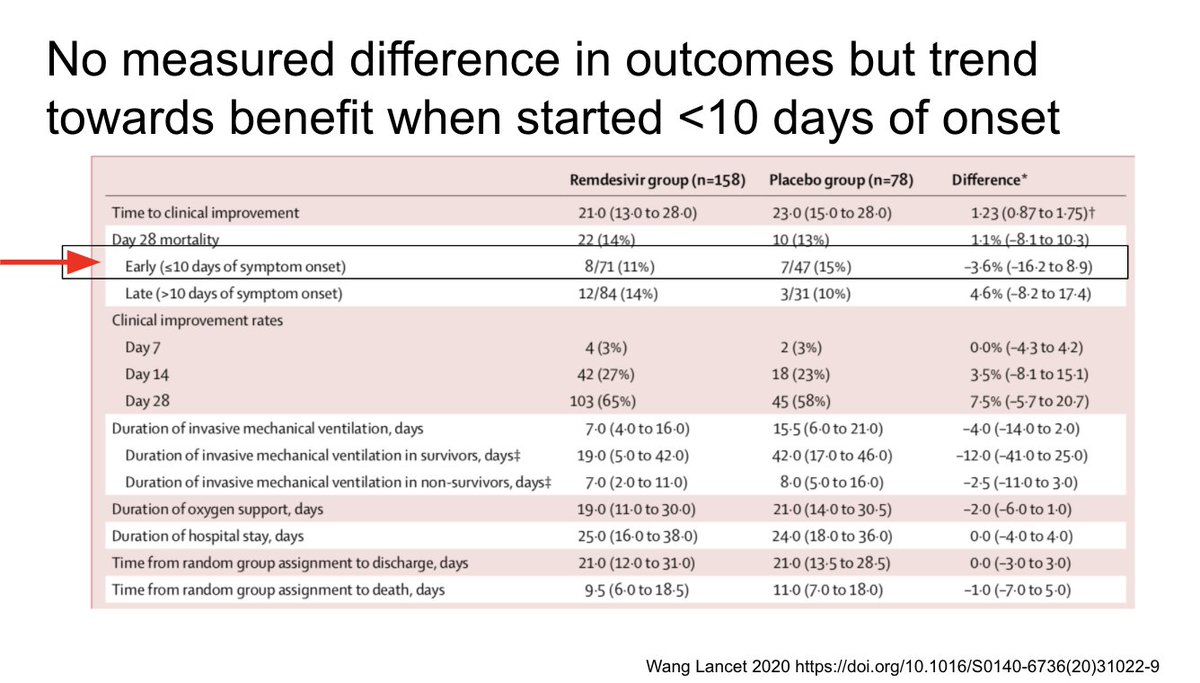
Overall they found no benefit to remdesivir. However in the early subgroup (ie enrolled within 10 days of symptom onset) there was a trend towards improved mortality 11 versus 15%. This was underpowered study so this needs to be investigated further
On the left KM curves of time to improvement (no difference). On the right you see viral load from upper (A) and lower (B) respiratory tracts: no difference in clearance for RDV compared with placebo.
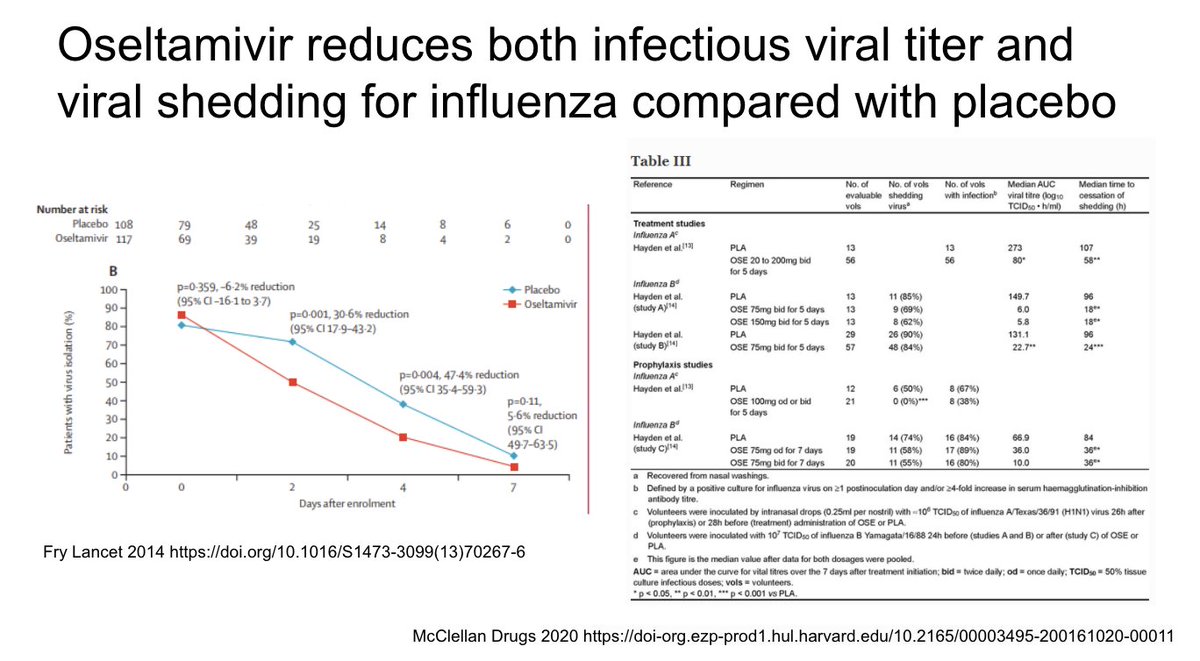
Lack of difference in viral shedding confusing for many. For influenza, baloxavir is associated with decreased viral shedding, as shown here
Oseltamivir reduces infectious viral titer (shown on the left) and viral shedding, shown in the table on the right from a meta analysis
SARS-CoV-2 may be diff, however. See this rhesus macaque study where RDV showed a clinical benefit and change in infectious viral titer (right) but not a significant change in viral load from lower respiratory tract, possibly consistent with Lancet study
https://doi.org/10.1101/2020.04.15.043166">https://doi.org/10.1101/2...
https://doi.org/10.1101/2020.04.15.043166">https://doi.org/10.1101/2...
On April 29, NIH release preliminary results from RDV versus placebo study. RDV group had 31% faster time to clinical recovery (11 versus 15 days) and a trend towards mortality benefit. More results soon in the expected peer reviewed article
NIH study results led to FDA emergency use authorization (EUA) for RDV. Details of distribution plan expected imminently
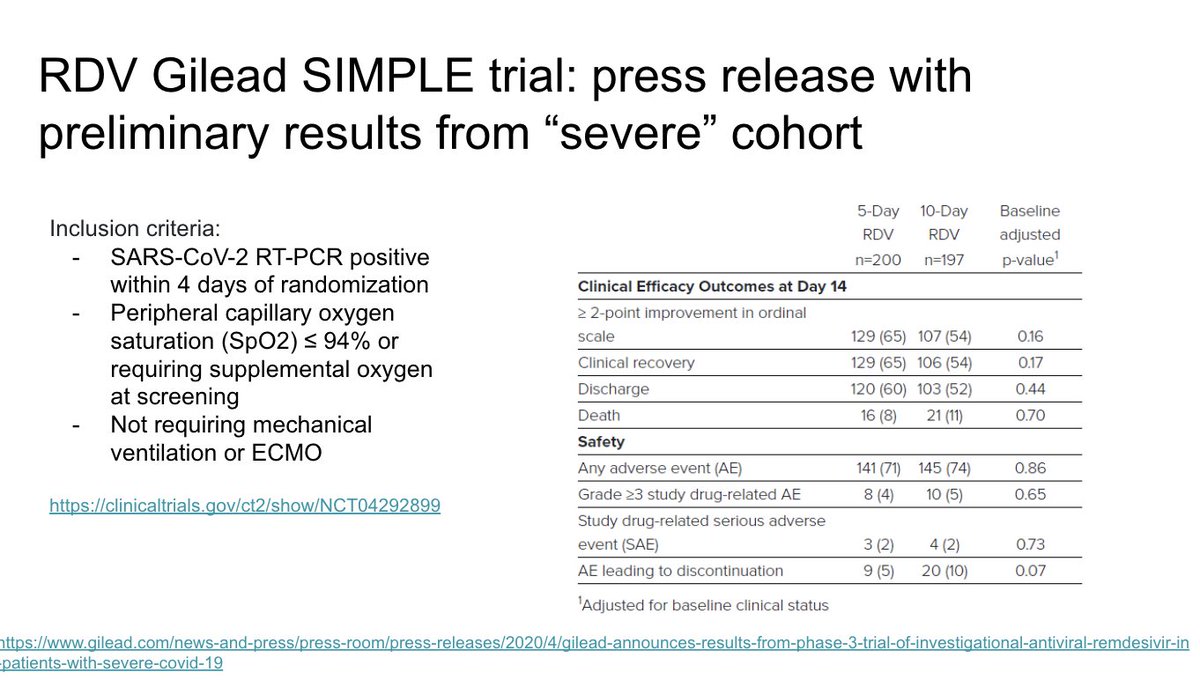
Gilead also released data from their “severe” study of RDV (in patients not on mechanical ventilation or ECMO) showing no difference between 5 or 10 days of RDV
We’ve reviewed multiple studies before that have shown evidence of a hyperinflammatory state and that worse hyperinflammation (including higher IL-6 levels) are associated with more severe disease
We reviewed this study last time that suggested that high IL-6 levels on admission were associated with need for mechanical ventilation
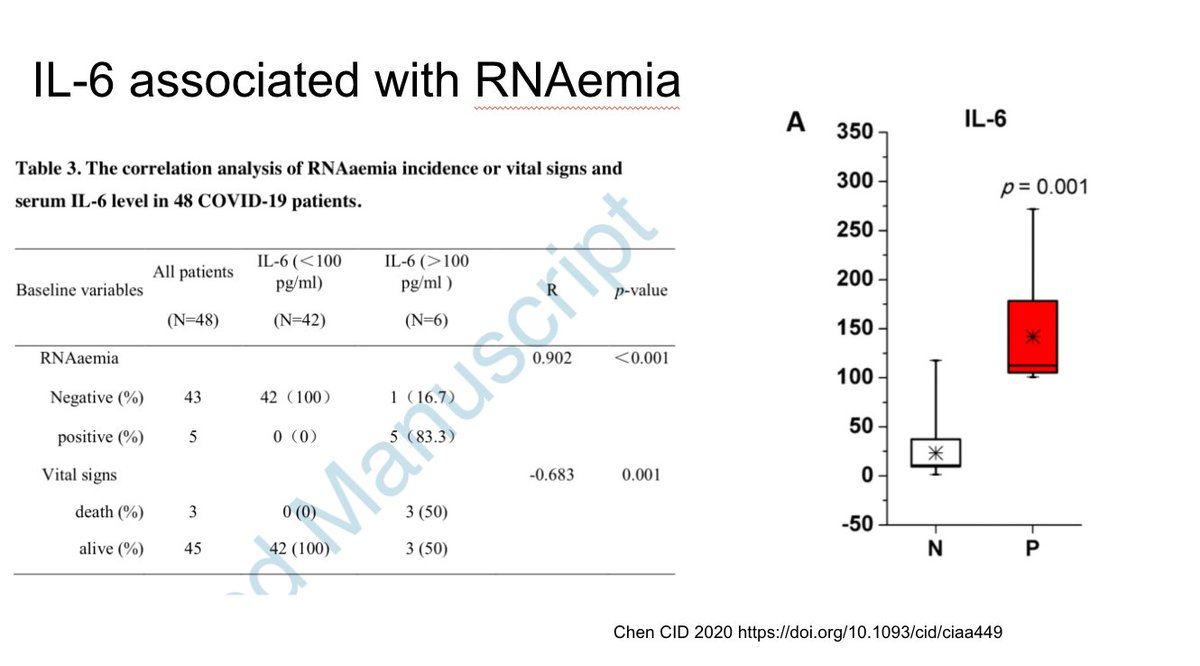
This study showed the viremia was associated with high IL-6 levels.
https://doi.org/10.1093/cid/ciaa449">https://doi.org/10.1093/c...
https://doi.org/10.1093/cid/ciaa449">https://doi.org/10.1093/c...
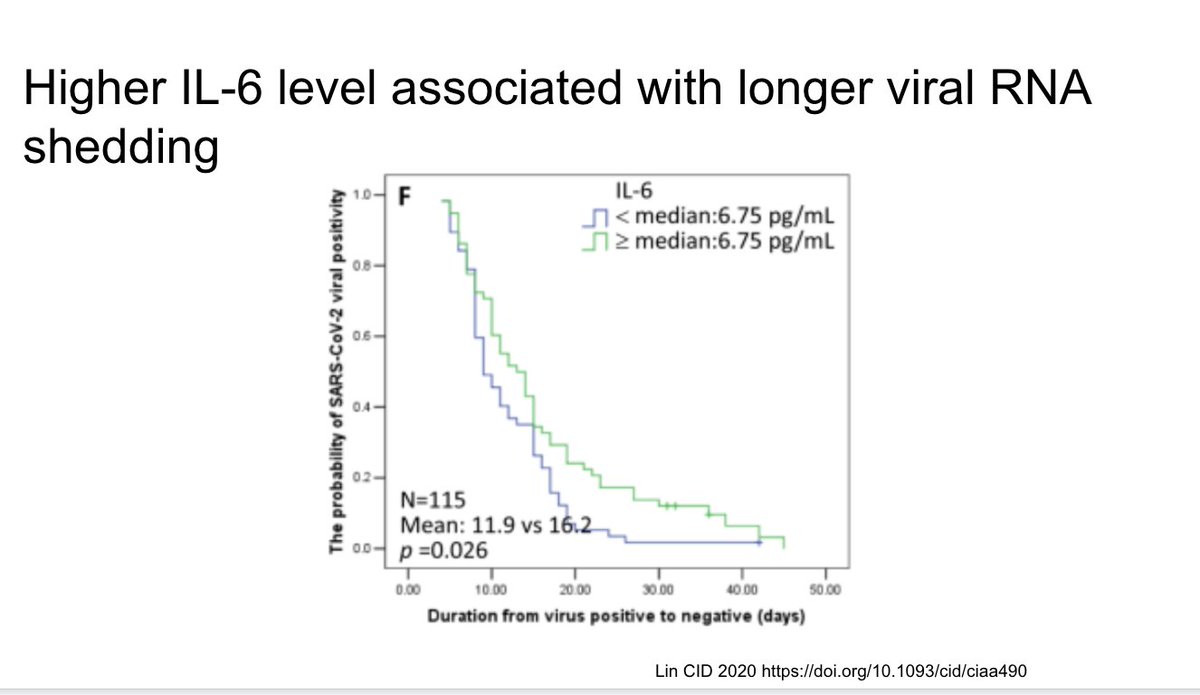
This new study in CID reviewed factors associated with prolonged viral shedding and found higher IL-6 levels were associated with longer shedding
https://doi.org/10.1093/cid/ciaa490">https://doi.org/10.1093/c...
https://doi.org/10.1093/cid/ciaa490">https://doi.org/10.1093/c...
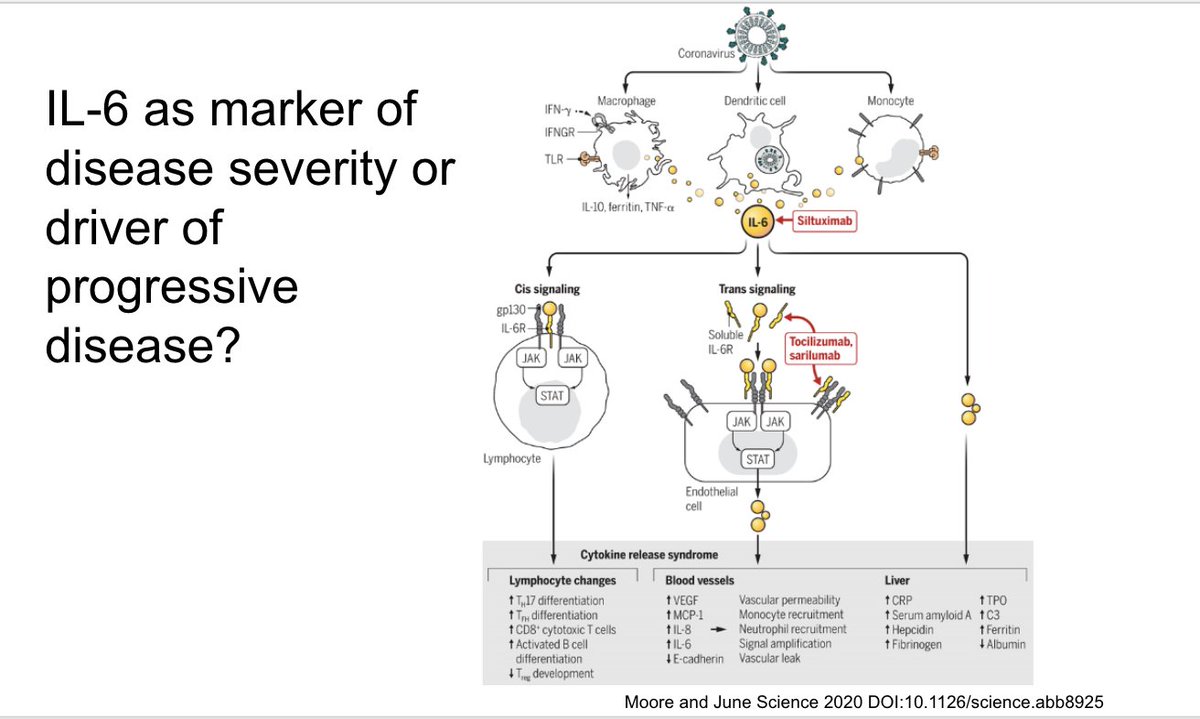
A critical question is whether IL-6 is a marker of disease severity or an actual driver of progressive disease. This nice review from Science compares the pathophysiology of cytokine release syndrome seen after CAR-T cell therapy to the hyperinflammatory state in COVID-19
There was early interest in targeting the IL6 pathway to see if it would help improve outcomes. This preprint describing a series of 21 patients from China treated with tocilizumab (an IL6 receptor blocker) created a lot of excitement about this
This is another non-randomized series (without a control group) from China describing 15 patients with COVID treated with toci. There were 3 deaths and 10/12 others improved
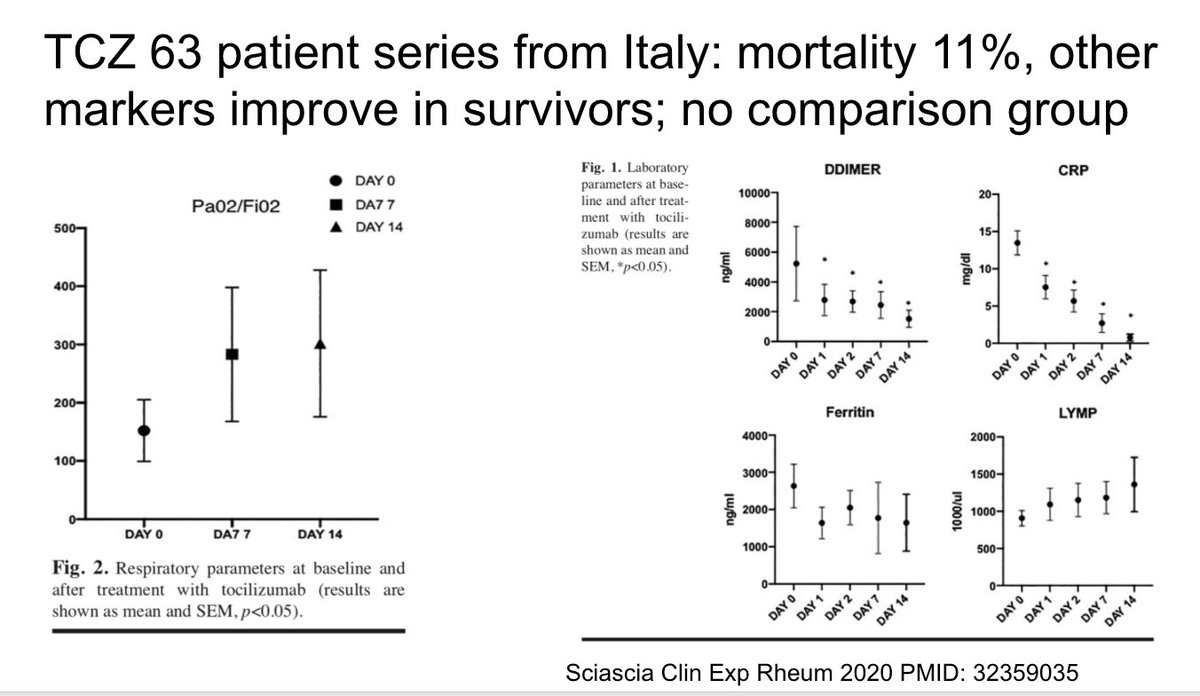
On May 1 the largest toci series to date was published from Italy including 63 patients. They had an 11% mortality rate and improved markers and oxygenation otherwise as shown here
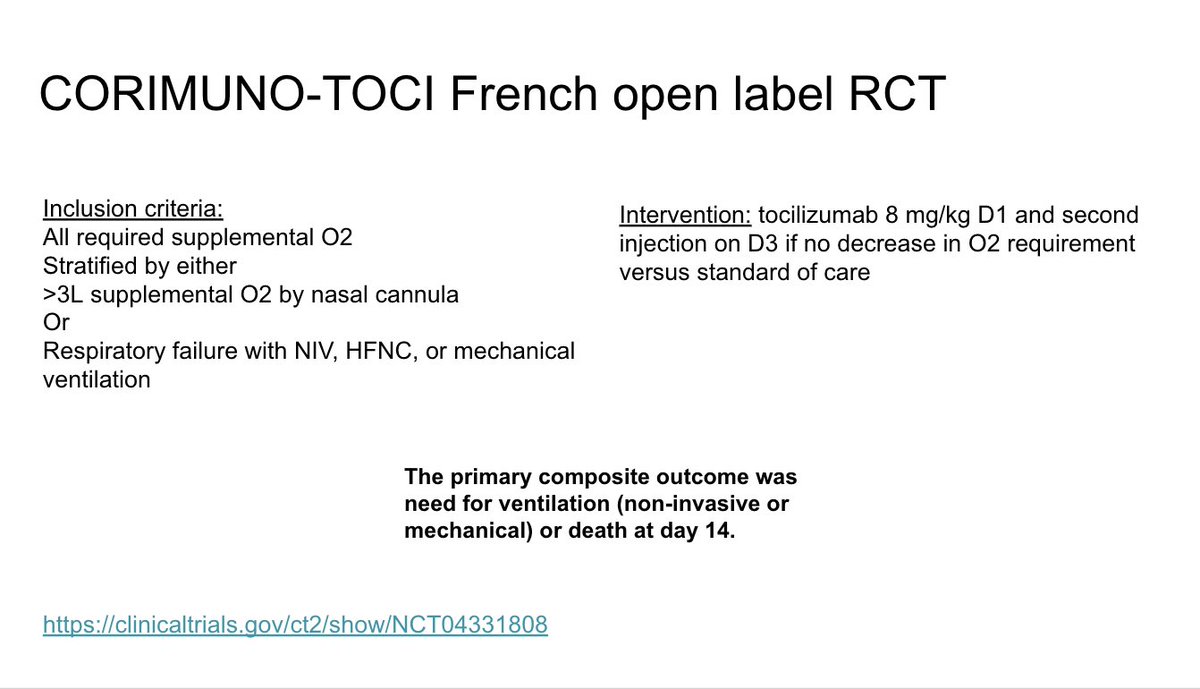
There are multiple other case reports and series describing use of toci or other IL6 blockers some of which are shown on this slide. What we need are randomized controlled trials to understand efficacy
On April 27 a press release gave an update on the sarilumab trial. The phase 3 trial with continue with sarilumab 400 mg versus placebo in critical patients only
They reported “negative trends” in severe group of phase 2 trial that were not seen in the phase 3 trial without other details. They reported positive trends in the critical group as shown marked by the orange star here.
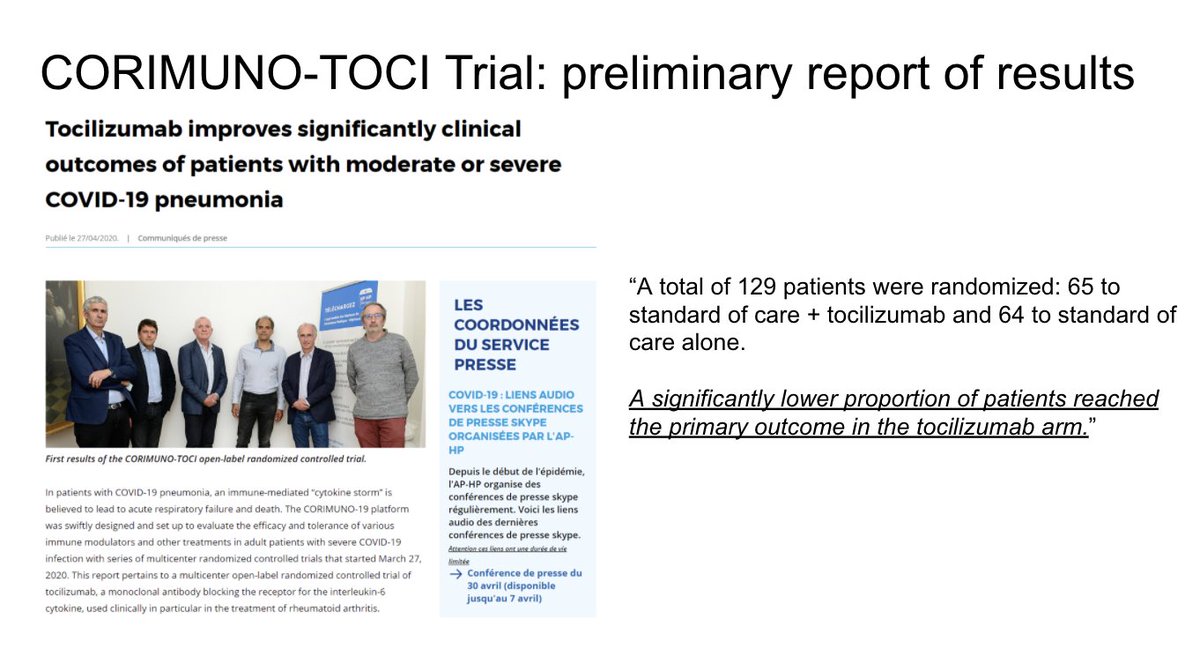
They reported a benefit with tocilizumab. More details are hopefully to come soon. We need more placebo controlled data on this topic to learn more
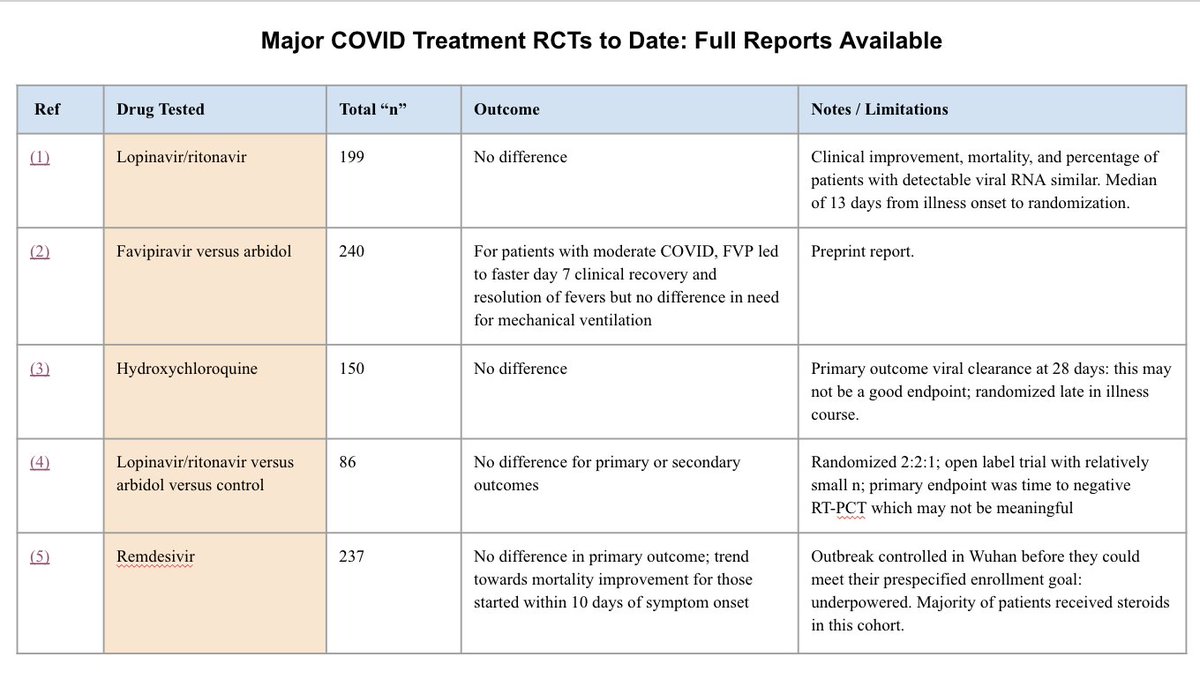
This slide has other major COVID treatment RCTs with preliminary data with hyperlinks to press releases
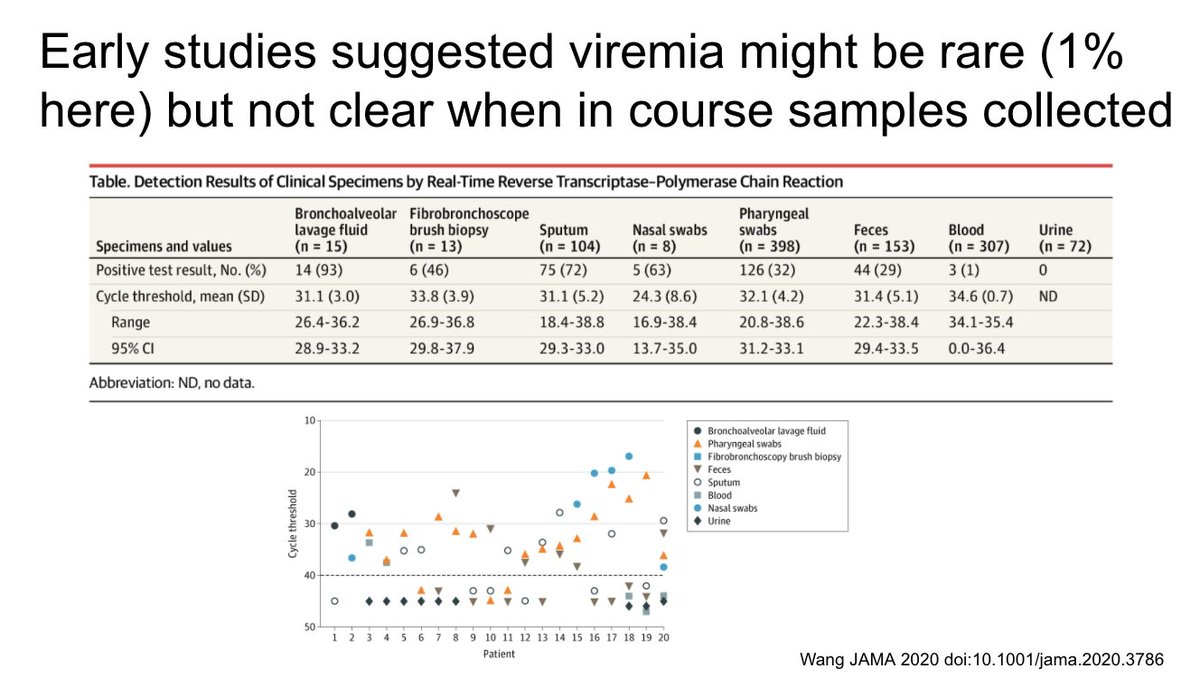
This study found viremia in 33% of cases, including 22/28 who needed hospital admission. In longitudinal samples viremia was seen for up to 10 days, including in many patients in the ICU (as shown on the left in this slide)
https://doi.org/10.1101/2020.04.26.20080101">https://doi.org/10.1101/2...
https://doi.org/10.1101/2020.04.26.20080101">https://doi.org/10.1101/2...
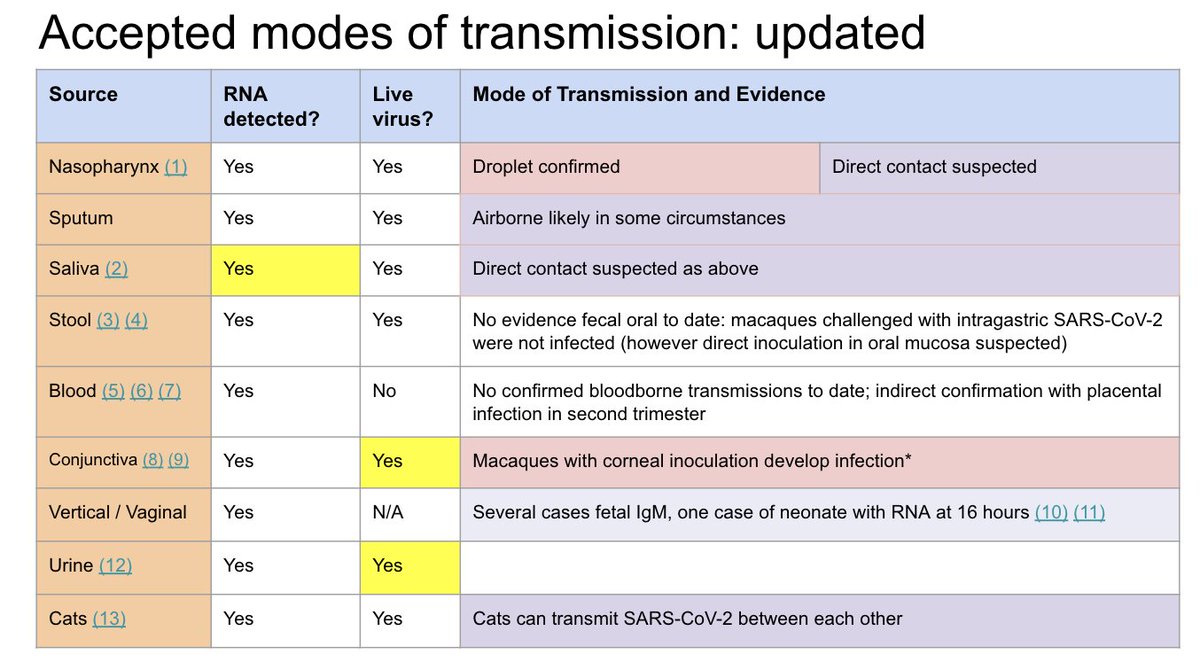
Important question is whether measuring viral RNA in the blood reflects systemic infection with infectious virus or not?
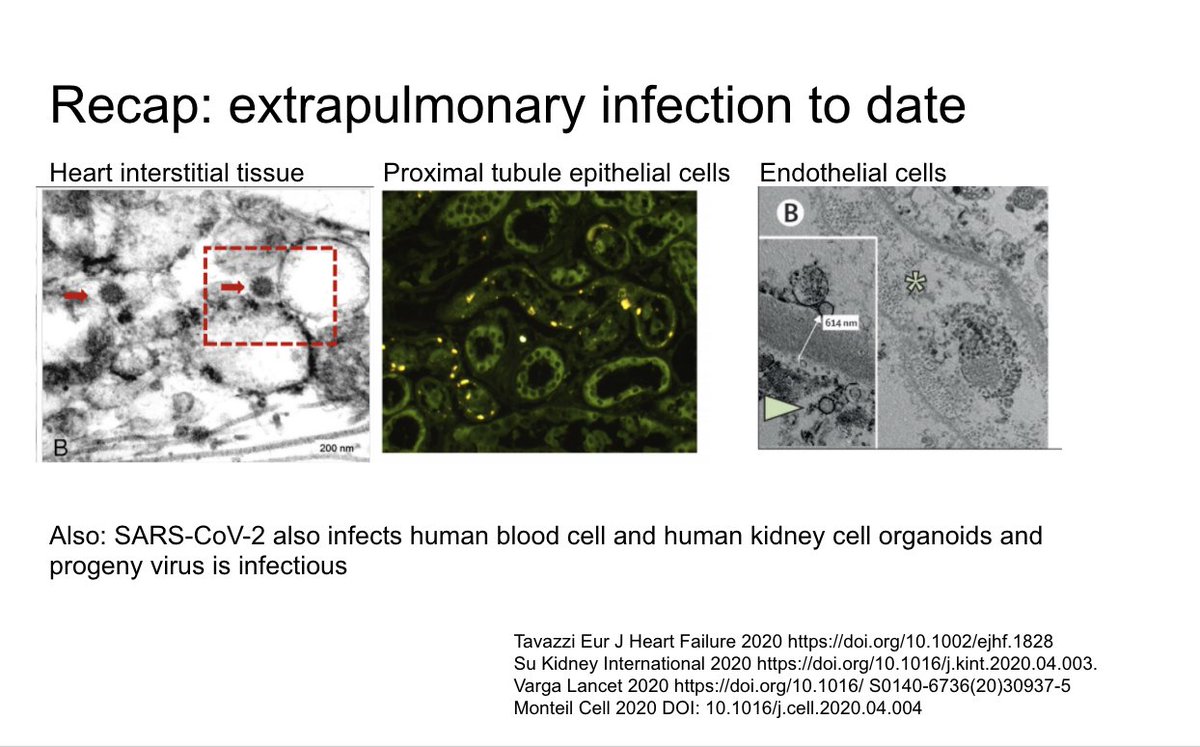
There is accumulating evidence of extrapulmonary infection including papers we have reviewed before summarized in this slide
This is a new study showing enterocyte organoids can be infected and that progeny virus is infectious
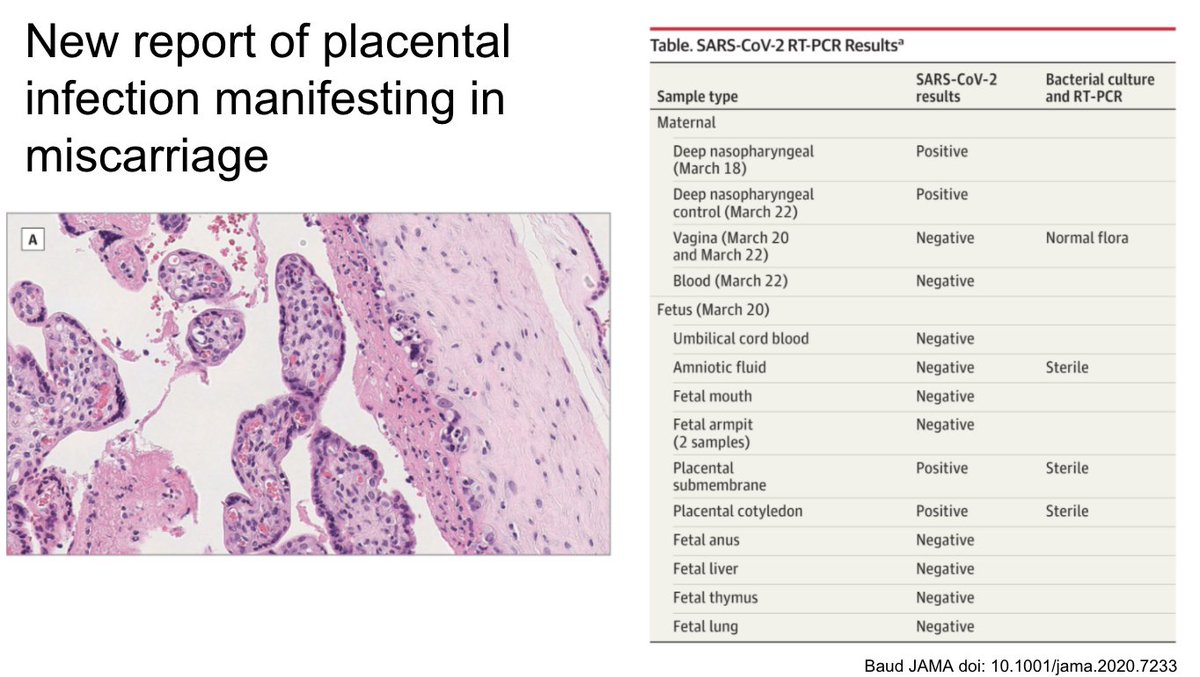
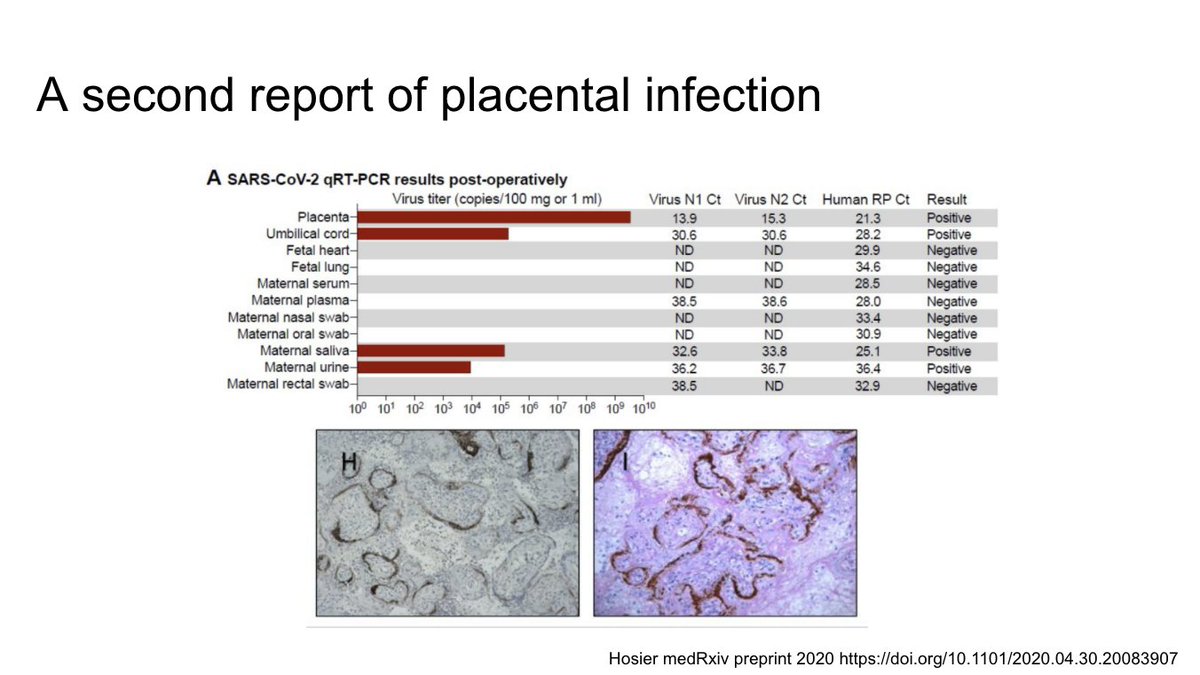
This is a second similar case. You can see the immunohistochemical staining for SARS-CoV-2 in the placenta
See: https://twitter.com/EricMeyerowitz/status/1254438680590192640">https://twitter.com/EricMeyer...
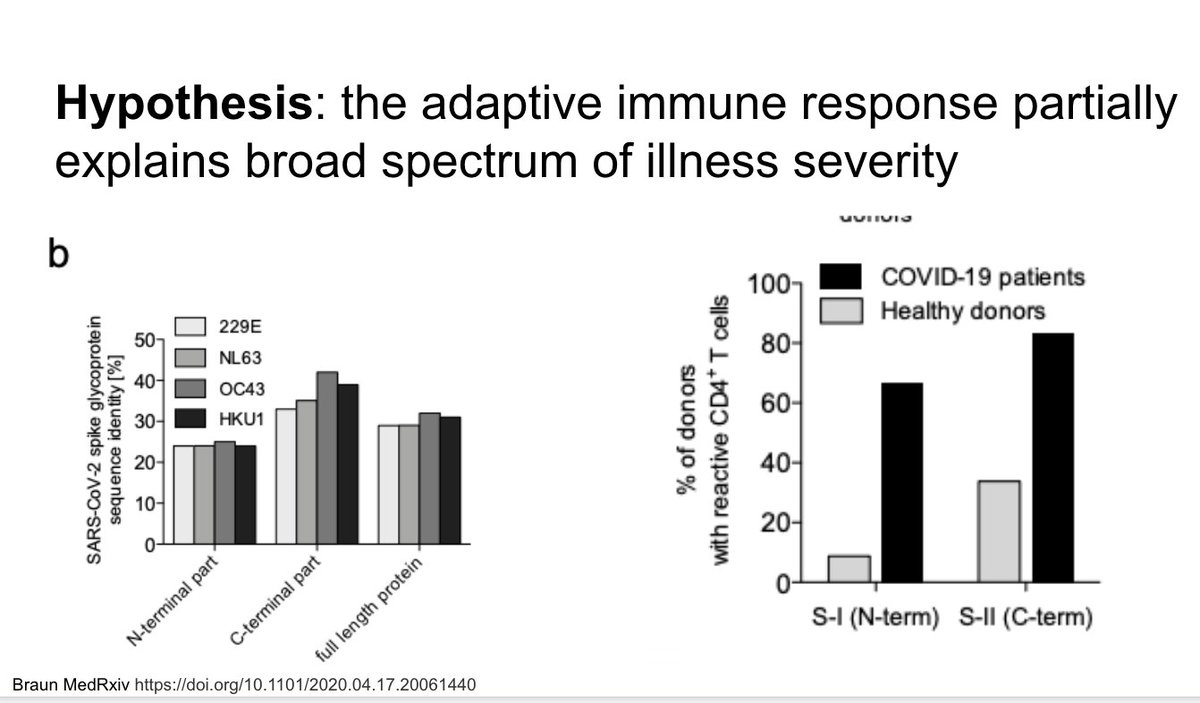
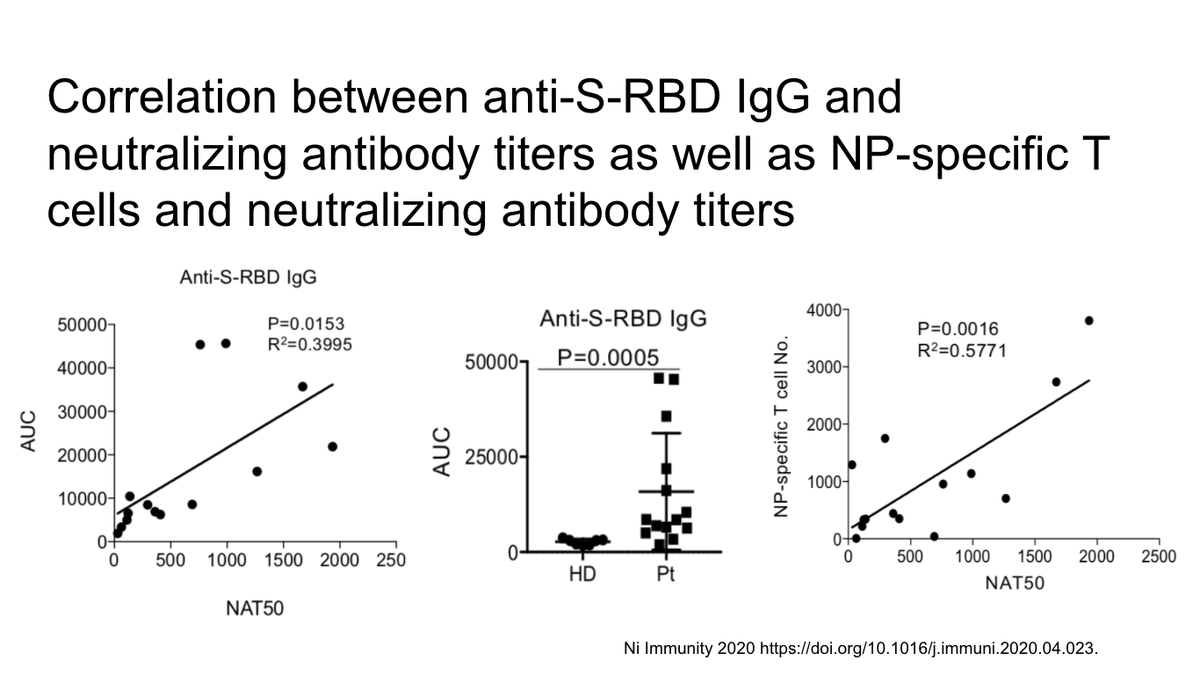
New study showing correlation between strong neutralizing antibodies and anti-S RBD IgG as well as N-protein specific reactive T-cells, suggesting immunity is both humoral and cellular
https://doi.org/10.1016/j.immuni.2020.04.023.">https://doi.org/10.1016/j...
https://doi.org/10.1016/j.immuni.2020.04.023.">https://doi.org/10.1016/j...
paper using dual-energy CT to suggest an interesting pattern of lung perfusion in COVID patients who were suspected to have PE but did not
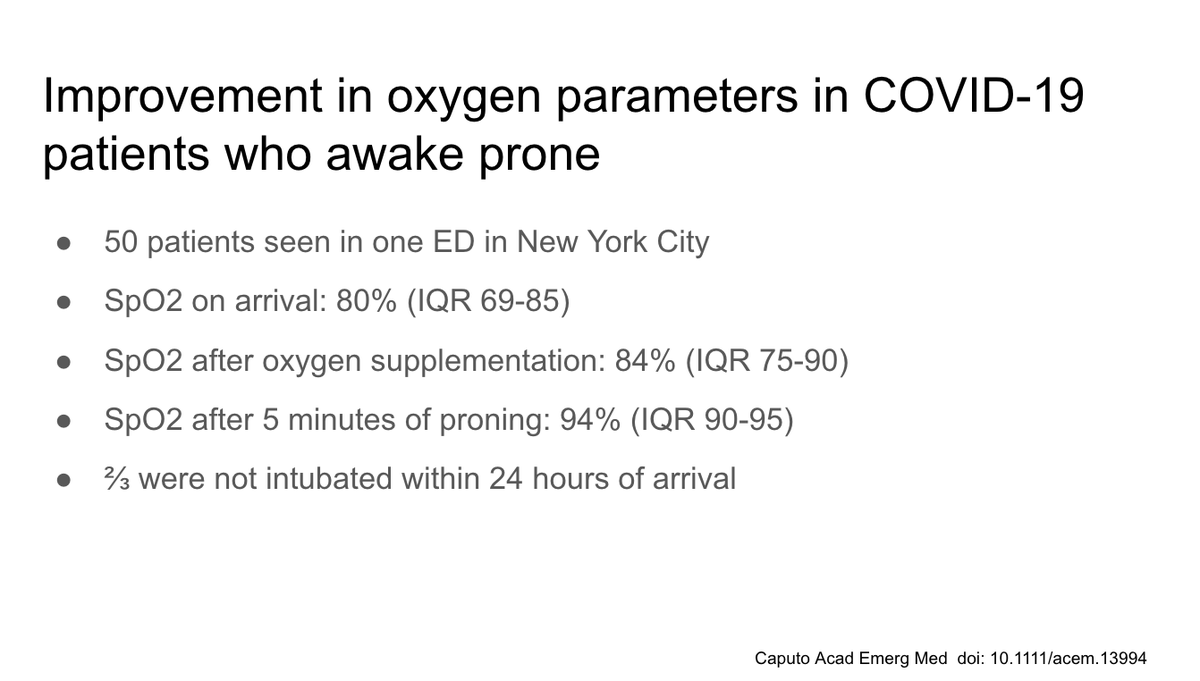
ED paper suggesting the benefits of awake proning, something we have all seen help anecdotally. Impact on long term outcomes unknown
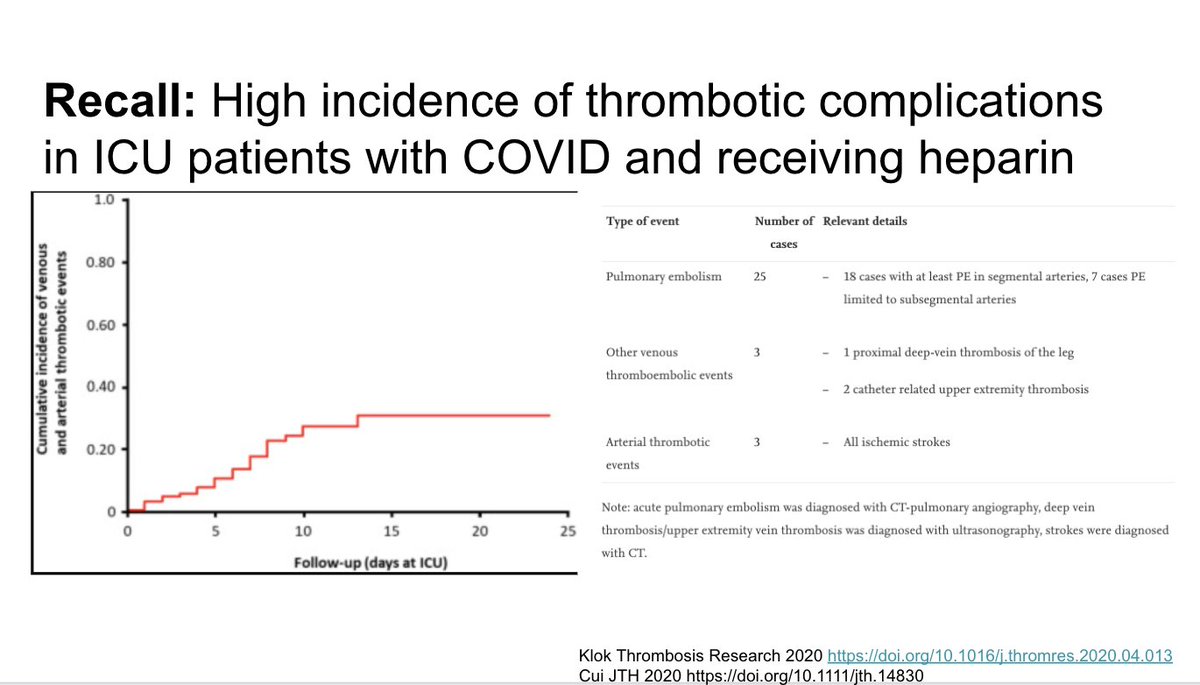
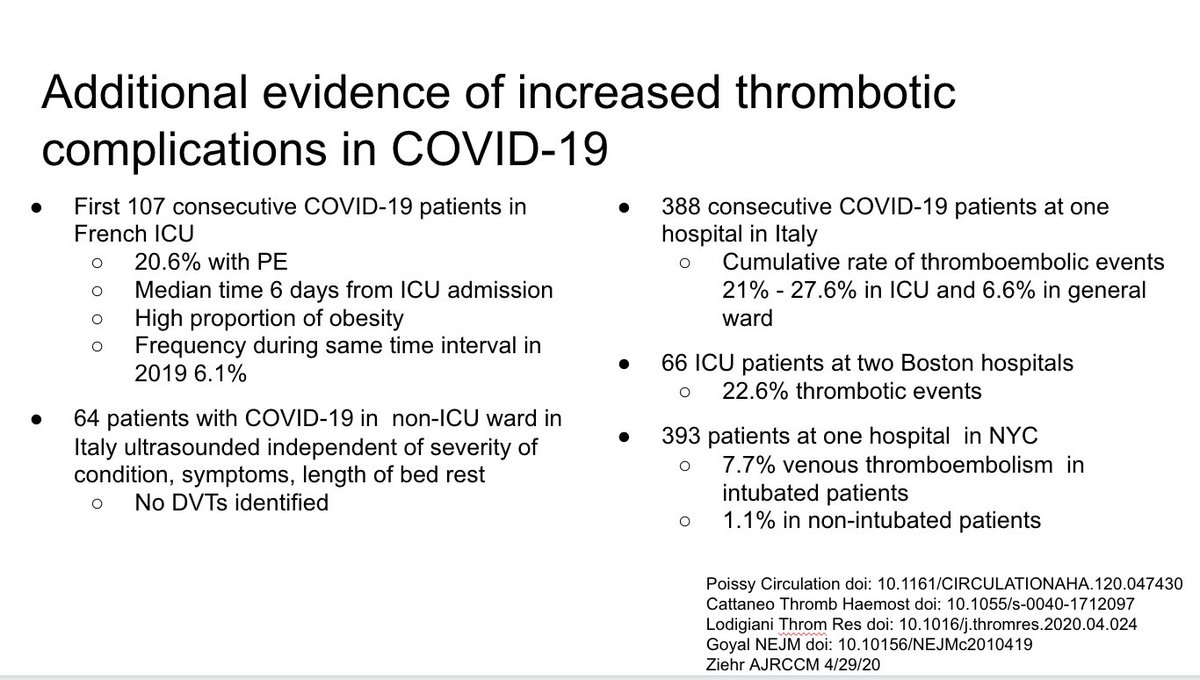
There have been a number of additional papers in the last two weeks better characterizing the thrombotic risk in COVID-19
There was also this concerning case series of 5 young people presenting with large-vessel stroke. Two had no co-morbidities. Two delayed ambulance because of concern for the pandemic.
However, the story isn& #39;t so simple as outlined in this commentary by @connors_md. Worth a read, she recommends regular thromboprophylaxis unless a specific indication for full dose anti-coag.
The connection between racism and COVID-19 has been long-suspected, and data on this subject has sadly been in short supply.
Despite this, a number of experts in critical race theory and public health have put out some great analyses that are worth going through.
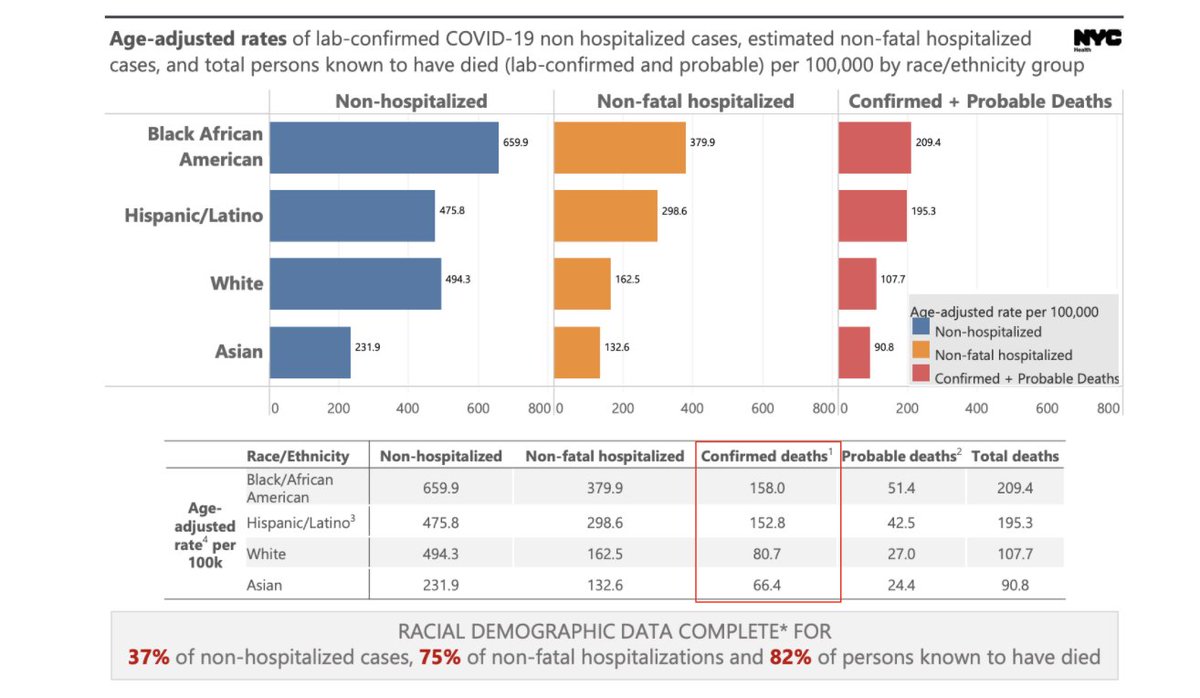
The NYC DPH has put out reasonably good data showing the differences in rates of COVID-19 and deaths from COVID-19 by race.
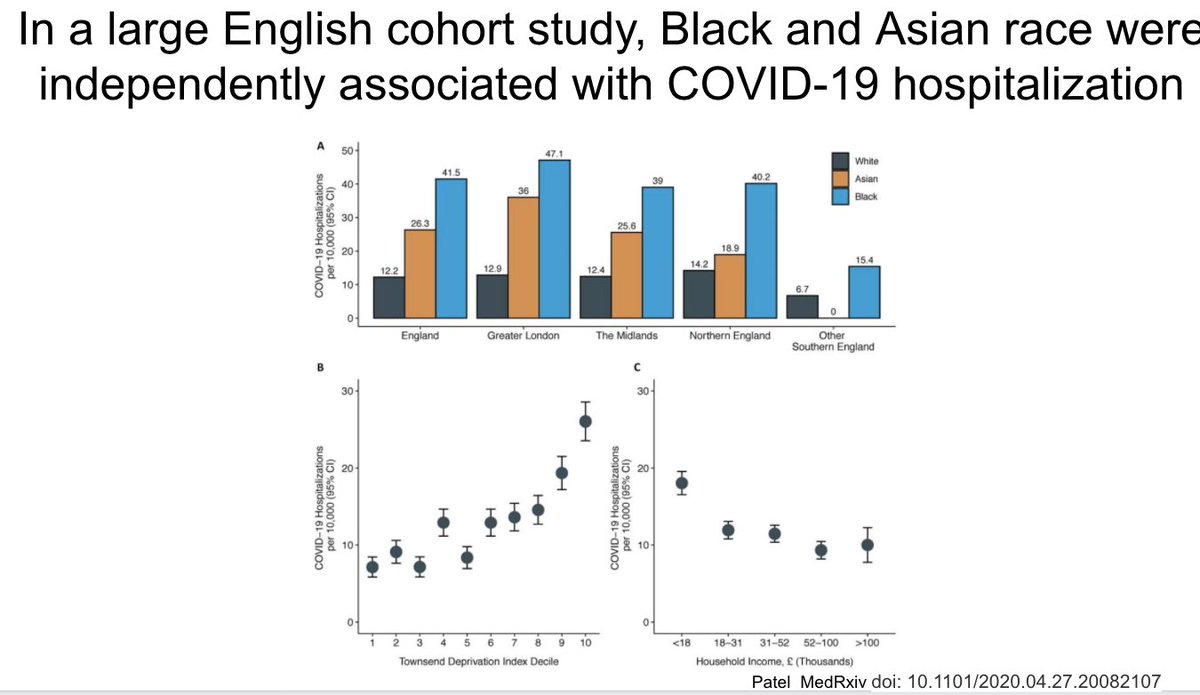
This analysis of a large English cohort study also demonstrated the relationship between racism and COVID-19, independent of socioeconomic status
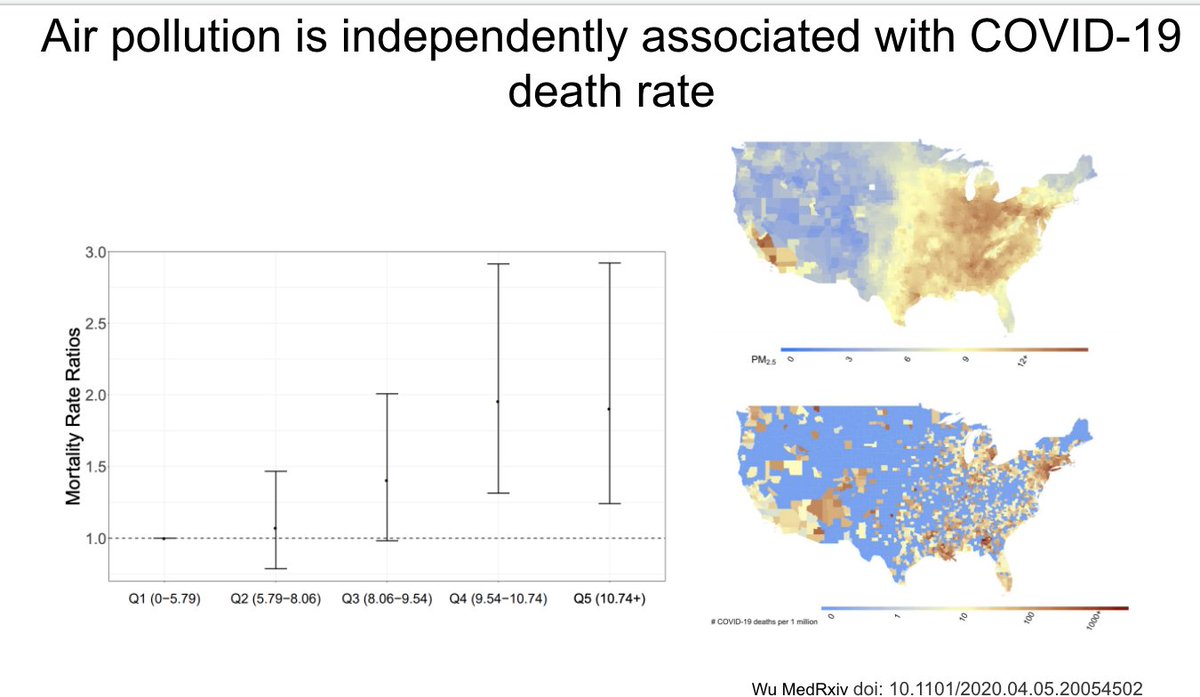
The pathogenesis of differential racial outcomes for COVID-19 are likely to be complex. As one example, this ecologic study suggests a connection between air polution and death from COVID-19
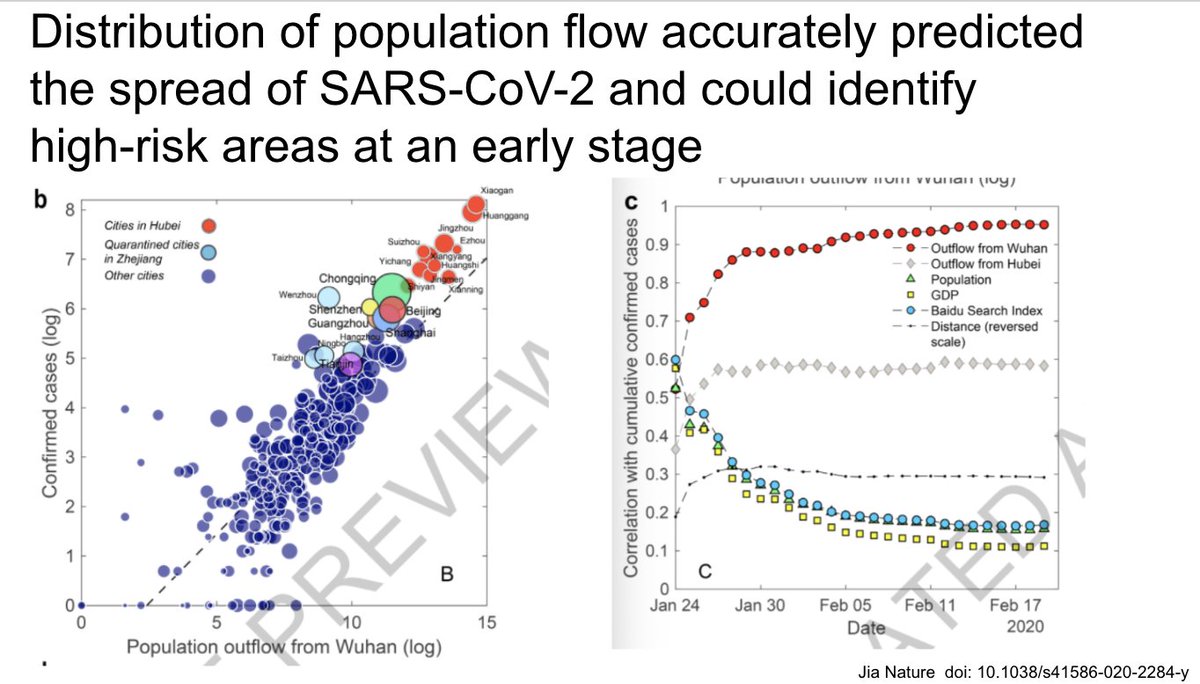
There have been a number of important studies in the last few weeks furthering our understanding of population strategies for epidemic control
This group showed how mobility data can be used to estimate local risk of transmission over time, although the utility now that infection is widespread remains to be seen
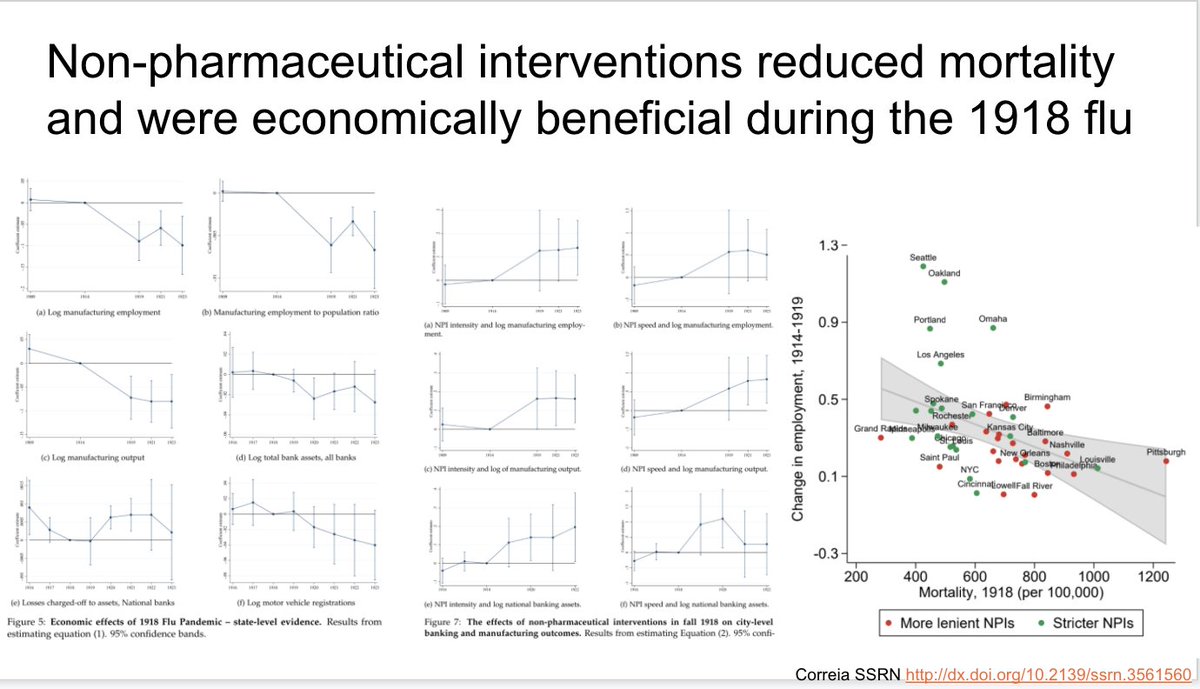
This study of the 1918 influenza pandemic showed that 1) pandemics are bad for the economy 2) NPIs are probably good for the economy
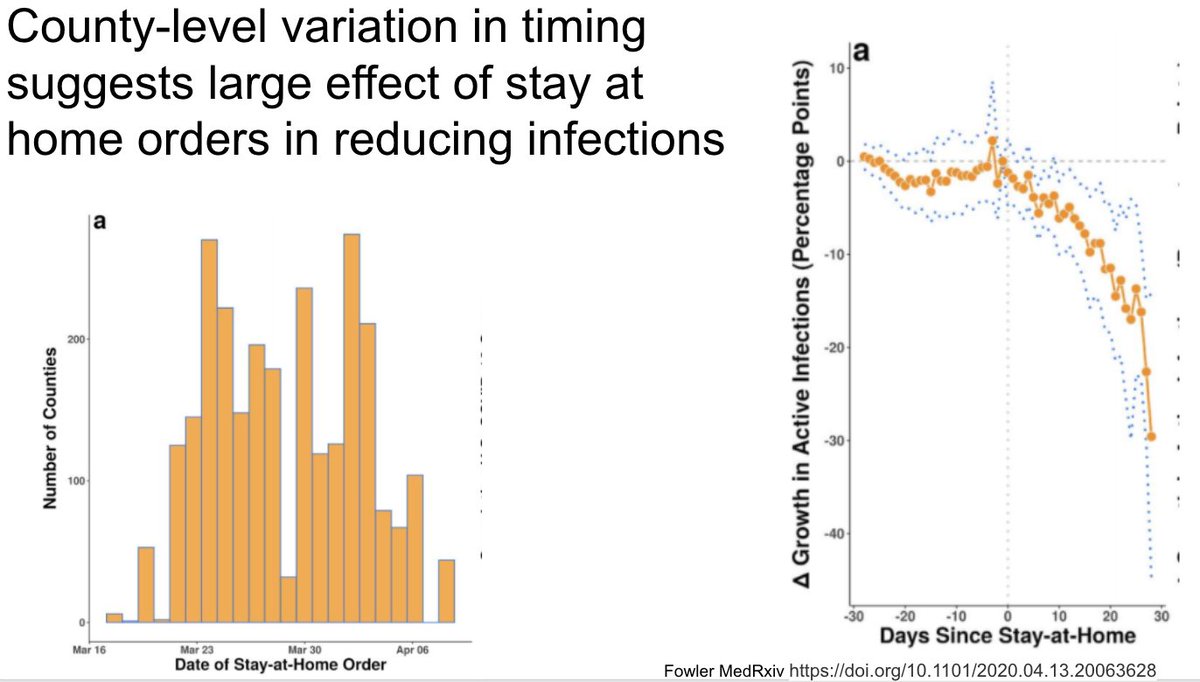
This interesting pre-print used a county-level fixed effects design to estimate the effect of stay-at-home orders in the US epidemic
https://doi.org/10.1101/2020.04.13.20063628">https://doi.org/10.1101/2...
https://doi.org/10.1101/2020.04.13.20063628">https://doi.org/10.1101/2...
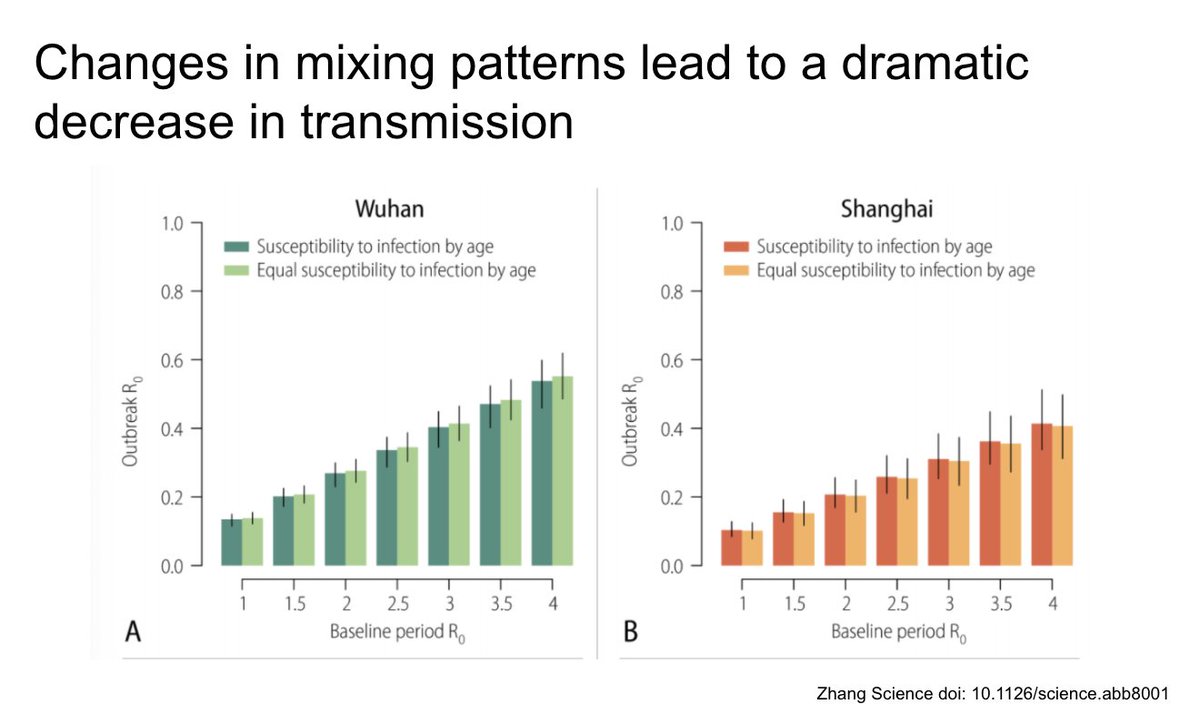
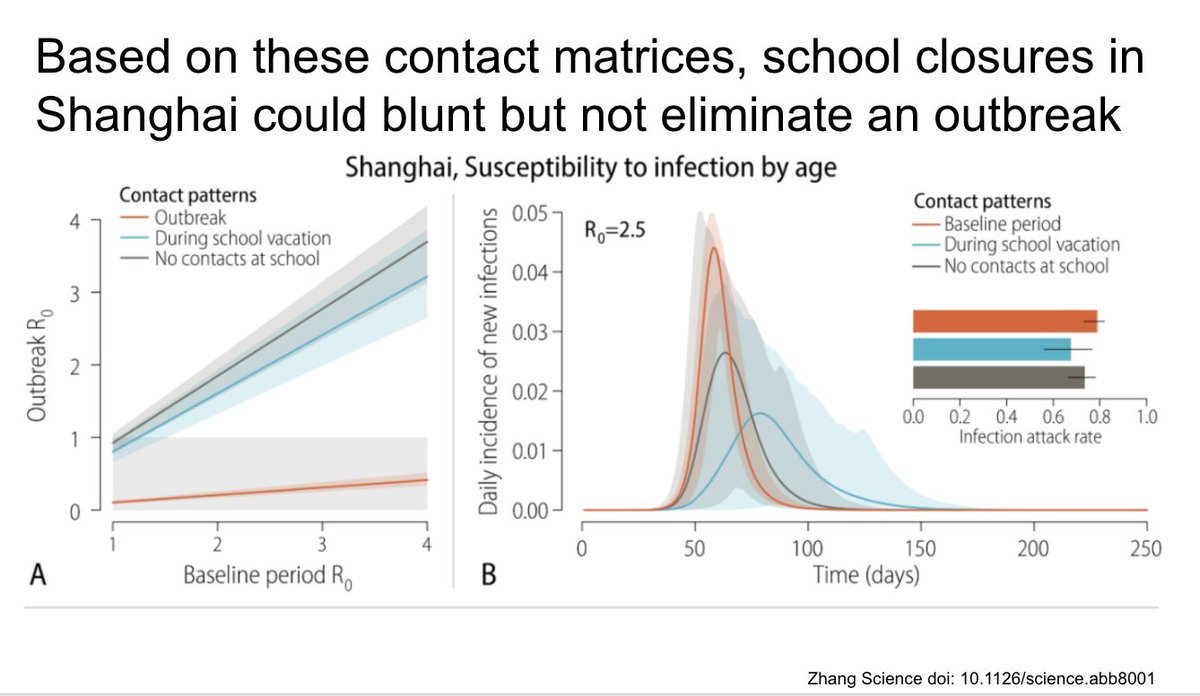
This study in Science shows one of the first detailed evaluation of contact patterns during the epidemic in China
They use these contact surveys to derive a model showing the reduction in the reproductive number based on changes in contacts
They further show how school closures in Shanghai might have blunted but not eliminated the outbreak
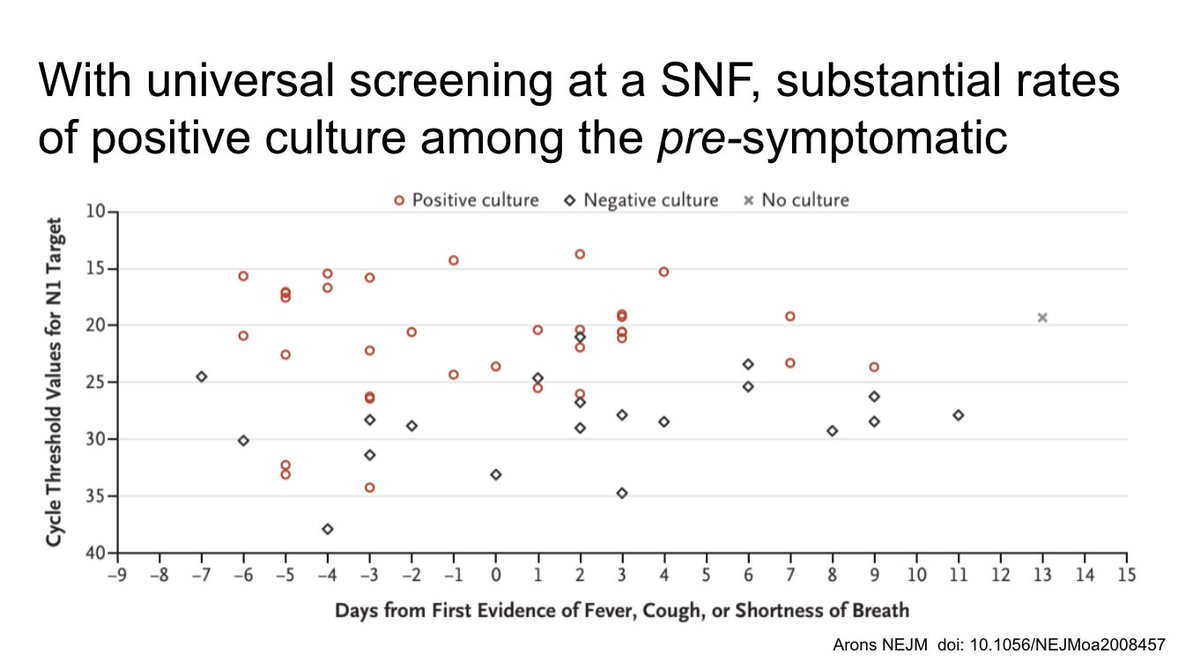
This paper in NEJM showed how much infectious virus can be found in the pre-symptomatic phase (red dots)
This was another detailed paper of viral RNA in aerosols in various parts of two hospitals in China, and the reduction with ventilation and sanitization
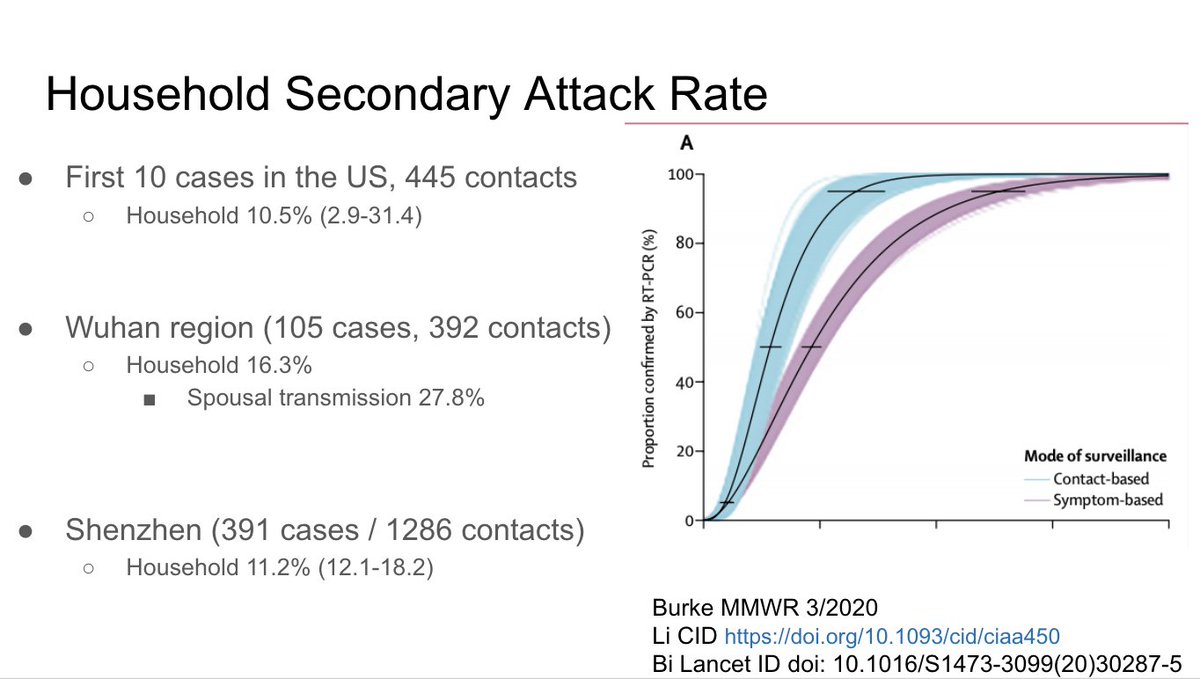
A few new papers demonstrating the importance of household transmission, as well as the reduction in time to isolation with a contact- rather than symptom-based surveillance
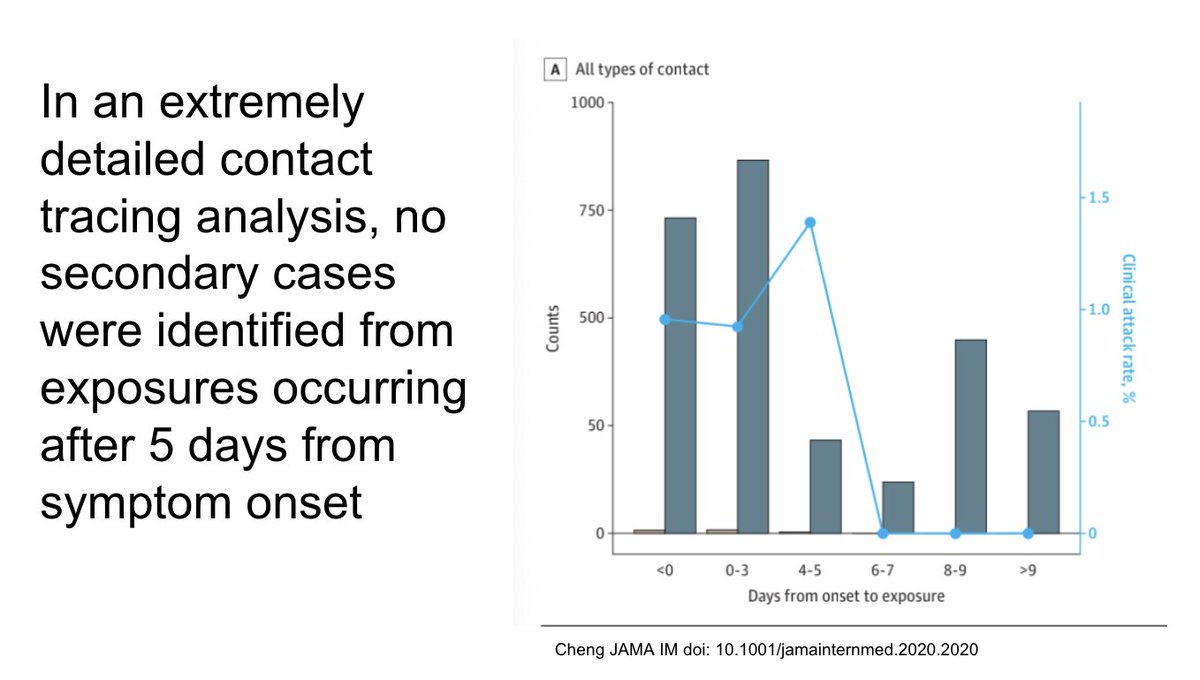
This paper in JAMA IM showed no transmissions from cases after 5 days of symptoms. Big implications for those people waiting a long time to get back to work, recovered but with positive swabs.
Prior updates https://twitter.com/AaronRichterman/status/1248280770973753347?s=20">https://twitter.com/AaronRich...

 Read on Twitter
Read on Twitter