I’m excited to share a project I’ve been working on to facilitate #helmet interface non-invasive ventilation for people with respiratory failure due to #COVID19. This thread is a brief #tweetorial on helmet interface ventilation.
1/
1/
Projections show that in a severe/continuing pandemic, the # of people requiring MV may exceed available vents. It’s not just the vents but a shortage of medications used to keep pts comfortable on the vent and personnel who know how to safely use them. https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(20)30315-7/fulltext
2/">https://www.thelancet.com/journals/...
2/">https://www.thelancet.com/journals/...
So what can be done? One thought is to build more vents, but that’s easier said than done: vents are complex, highly regulated devices. Despite lots of enthusiasm it& #39;s not easy/quick to ramp up vent production. It also doesn& #39;t fix medication shortages.
https://www.npr.org/2020/03/31/824886286/episode-987-the-race-to-make-ventilators
3/">https://www.npr.org/2020/03/3...
https://www.npr.org/2020/03/31/824886286/episode-987-the-race-to-make-ventilators
3/">https://www.npr.org/2020/03/3...
Not only are ventilators resource intensive, but patients with #COVID19 who are sick enough to require invasive ventilation often do poorly. This is more a correlation w/ disease severity rather caused by IMV per se. That said, what if we could avoid intubating COVID pts?
4/
4/
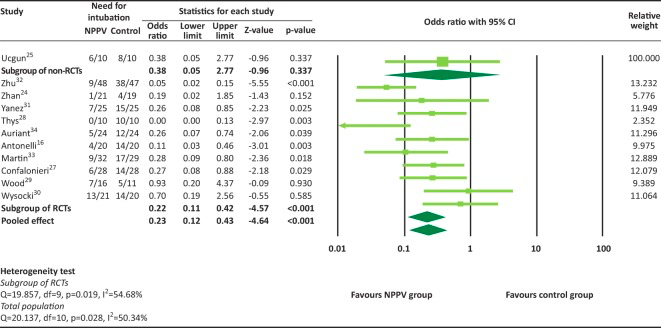
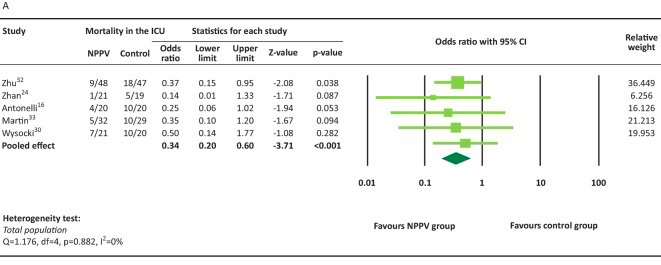
Several studies (and meta-analyses) have shown that in patients with hypoxemic respiratory failure we can avoid intubation by using non-invasive positive pressure ventilation (NIPPV). This can also potentially reduce ICU mortality.  https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Rightwards arrow" aria-label="Emoji: Rightwards arrow"> https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6297344/
https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Rightwards arrow" aria-label="Emoji: Rightwards arrow"> https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6297344/
5/">https://www.ncbi.nlm.nih.gov/pmc/artic...
5/">https://www.ncbi.nlm.nih.gov/pmc/artic...
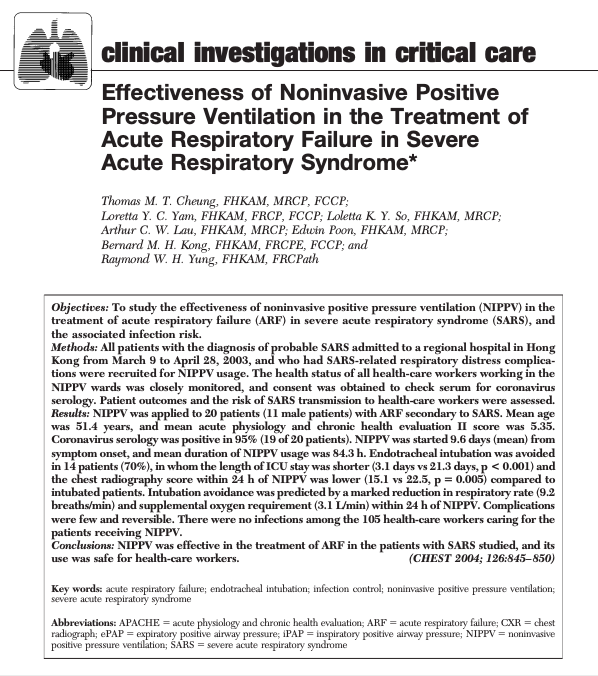
We also know NIPPV works for coronavirus: In the 2004 SARS outbreak, one group used NIPPV to avoid intubation in 70% of cases (n=14) and pts treated with NIPPV had shorter ICU LOS (3.1 vs 21.3 days). Importantly, none of the 105 HCWs exposed got SARS. https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Rightwards arrow" aria-label="Emoji: Rightwards arrow"> https://journal.chestnet.org/article/S0012-3692(15)31228-9/pdf">https://journal.chestnet.org/article/S...
https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Rightwards arrow" aria-label="Emoji: Rightwards arrow"> https://journal.chestnet.org/article/S0012-3692(15)31228-9/pdf">https://journal.chestnet.org/article/S...
6/
6/

 Read on Twitter
Read on Twitter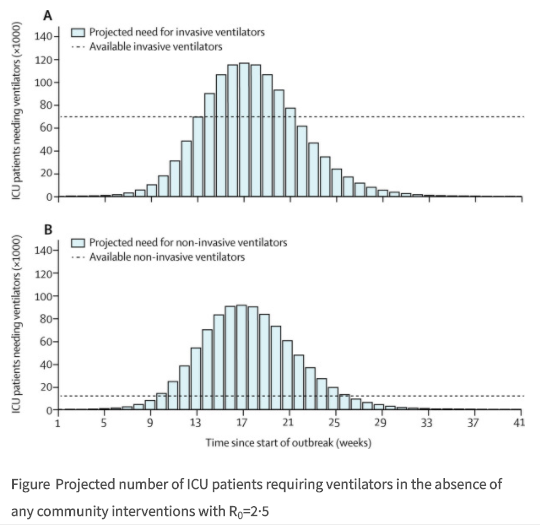
 https://www.ncbi.nlm.nih.gov/pmc/artic..." title="Several studies (and meta-analyses) have shown that in patients with hypoxemic respiratory failure we can avoid intubation by using non-invasive positive pressure ventilation (NIPPV). This can also potentially reduce ICU mortality. https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Rightwards arrow" aria-label="Emoji: Rightwards arrow"> https://www.ncbi.nlm.nih.gov/pmc/artic...">
https://www.ncbi.nlm.nih.gov/pmc/artic..." title="Several studies (and meta-analyses) have shown that in patients with hypoxemic respiratory failure we can avoid intubation by using non-invasive positive pressure ventilation (NIPPV). This can also potentially reduce ICU mortality. https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Rightwards arrow" aria-label="Emoji: Rightwards arrow"> https://www.ncbi.nlm.nih.gov/pmc/artic...">
 https://www.ncbi.nlm.nih.gov/pmc/artic..." title="Several studies (and meta-analyses) have shown that in patients with hypoxemic respiratory failure we can avoid intubation by using non-invasive positive pressure ventilation (NIPPV). This can also potentially reduce ICU mortality. https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Rightwards arrow" aria-label="Emoji: Rightwards arrow"> https://www.ncbi.nlm.nih.gov/pmc/artic...">
https://www.ncbi.nlm.nih.gov/pmc/artic..." title="Several studies (and meta-analyses) have shown that in patients with hypoxemic respiratory failure we can avoid intubation by using non-invasive positive pressure ventilation (NIPPV). This can also potentially reduce ICU mortality. https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Rightwards arrow" aria-label="Emoji: Rightwards arrow"> https://www.ncbi.nlm.nih.gov/pmc/artic...">
 https://journal.chestnet.org/article/S... 6/" title="We also know NIPPV works for coronavirus: In the 2004 SARS outbreak, one group used NIPPV to avoid intubation in 70% of cases (n=14) and pts treated with NIPPV had shorter ICU LOS (3.1 vs 21.3 days). Importantly, none of the 105 HCWs exposed got SARS.https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Rightwards arrow" aria-label="Emoji: Rightwards arrow"> https://journal.chestnet.org/article/S... 6/" class="img-responsive" style="max-width:100%;"/>
https://journal.chestnet.org/article/S... 6/" title="We also know NIPPV works for coronavirus: In the 2004 SARS outbreak, one group used NIPPV to avoid intubation in 70% of cases (n=14) and pts treated with NIPPV had shorter ICU LOS (3.1 vs 21.3 days). Importantly, none of the 105 HCWs exposed got SARS.https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Rightwards arrow" aria-label="Emoji: Rightwards arrow"> https://journal.chestnet.org/article/S... 6/" class="img-responsive" style="max-width:100%;"/>




