1/ A case and tweetorial as a reminder that even in the age of #covid-19 general internal and critical care medicine is important!
A 60s man was dx with Covid and sent. 3 days later he developed nausea, vomiting, lethargy, and confusion and his wife called EMS.
A 60s man was dx with Covid and sent. 3 days later he developed nausea, vomiting, lethargy, and confusion and his wife called EMS.
2/ In the ED, he was tachypneic, diaphoretic and altered with increased work of breathing. T 37.4 HR 115 BP 149/99 RR 30, O2 sat 98% on RA.
Exam: confabulating, diaphoretic, pupils dilated and reactive, labored breathing with accessory muscles, extremities cool with no edema.
Exam: confabulating, diaphoretic, pupils dilated and reactive, labored breathing with accessory muscles, extremities cool with no edema.
3/
CXR had mild bilateral alveolar opacities consistent with covid.
He was put on supplemental O2 6L NC for WOB and an ABG was obtained:
7.46/18/223. What do you want to do next?
CXR had mild bilateral alveolar opacities consistent with covid.
He was put on supplemental O2 6L NC for WOB and an ABG was obtained:
7.46/18/223. What do you want to do next?
4/ His ABG shows resp alkalosis. He is oxygenating well with a PO2 of 223. On 6L NC, FiO2 is roughly 44%. With rapid breathing there is more mixing of ambient air which decreases the FiO2 so let& #39;s assume the patient is recieving approximately 40% FiO2.
5/ Calculating PAO2 = (FiO2 x [Atm Pressure – H2O pressure] – PaCo2/Resp quotient) --> AA gradient of 40. This is mildly elevated but overall there is not significant hypoxemia or impaired gas exchange.
6/ In Covid we’ve often been seeing primarily significant hypoxemia, so what is happening here? Let’s take a look at some more labs:
Na 137
K 5.5
Cl 96
HCO3- 14
BUN 26
Cr 0.65
Glucose 255
WBC 9.30
Hgb 16.3
Platelet 676
Based on this and the ABG, what is his acid/base status?
Na 137
K 5.5
Cl 96
HCO3- 14
BUN 26
Cr 0.65
Glucose 255
WBC 9.30
Hgb 16.3
Platelet 676
Based on this and the ABG, what is his acid/base status?
7/ AG = 27. Anion-gap acidosis
Winter’s Formula expected PCo2 = 27-31. Actual pCO2 18 so respiratory alkalosis
Delta AG= 15. Expected bicarb= (24-15) = 9. Actual bicarb is 14. 14>9 = metabolic alkalosis
Triple acid-base disorder.
The next question is: why is there a gap?
Winter’s Formula expected PCo2 = 27-31. Actual pCO2 18 so respiratory alkalosis
Delta AG= 15. Expected bicarb= (24-15) = 9. Actual bicarb is 14. 14>9 = metabolic alkalosis
Triple acid-base disorder.
The next question is: why is there a gap?
8/ To address the most common causes of anion-gap acidosis: Lactate 2.3, trace urine ketones.
With this information a diagnostic test was performed and a diagnosis was made!
What was the diagnostic test?
With this information a diagnostic test was performed and a diagnosis was made!
What was the diagnostic test?
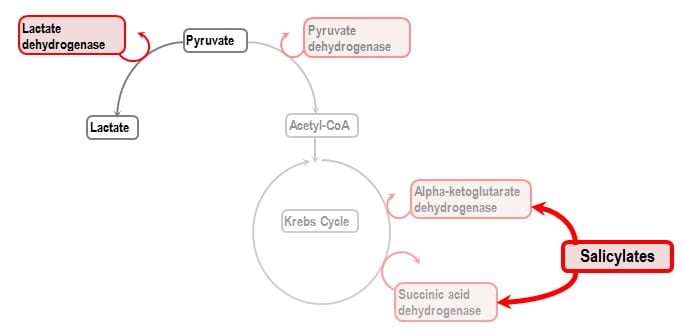
9/ A salicylate level was sent and returned at 53 mg/dL (therapeutic levels are between 10 -30, and toxicity begins at levels > 40). The patient had been taking aspirin and Tylenol in high doses for fevers and headaches at home ultimately leading to Salicylate (aspirin) toxicity.
10/ Salicylate poisoning causes:
-Tachypnea, hyperthermia, tachycardia (due to hypovolemia)
- Tinnitus
- N/V
- AMS
Lab testing shows anion gap acidosis and respiratory alkalosis. Direct RR stimulation, and gap from salicylate (weak acid), organic acids, lactate, ketones
-Tachypnea, hyperthermia, tachycardia (due to hypovolemia)
- Tinnitus
- N/V
- AMS
Lab testing shows anion gap acidosis and respiratory alkalosis. Direct RR stimulation, and gap from salicylate (weak acid), organic acids, lactate, ketones
11/ Treatment of salicylate toxicity:
-ABCs. Intubation + pressors may be needed
-Correct hypovolemia with IVFs
-Alkalinization of serum and urine using a bicarbonate gtt. Target serum pH > 7.5, urine pH >8.
-Maintain serum glucose > 100. ASA leads to decreased CNS glucose
-ABCs. Intubation + pressors may be needed
-Correct hypovolemia with IVFs
-Alkalinization of serum and urine using a bicarbonate gtt. Target serum pH > 7.5, urine pH >8.
-Maintain serum glucose > 100. ASA leads to decreased CNS glucose
12/ Treatment continued:
-Monitor UOP and Cr closely. Have a low threshold for hemodialysis to remove salicylate. Start iHD if significantly altered mental status, pulmonary edema / fluid overload, AKI or poor UOP, significant acidosis, or cerebral edema
-Monitor UOP and Cr closely. Have a low threshold for hemodialysis to remove salicylate. Start iHD if significantly altered mental status, pulmonary edema / fluid overload, AKI or poor UOP, significant acidosis, or cerebral edema
13/ The patient was hydrated and started on a bicarbonate drip. Despite this he had AKI and declining UOP. He required dialysis temporarily which was stopped after salicylate level cleared, and he had renal recovery. His mental status improved and he never required intubation.
14/ Moral of the story is keep your differential broad even when everyone has Covid. I have had multiple patients with “Covid + blank” ranging from GI bleed to aspirin toxicity to adrenal insufficiency.
@DxRxEdu @AmitGoyalMD @Dr_DanMD @thecurbsiders @CPSolvers @BBroderickMD
@DxRxEdu @AmitGoyalMD @Dr_DanMD @thecurbsiders @CPSolvers @BBroderickMD

 Read on Twitter
Read on Twitter