1/ I haven’t written a #periopmedicine #tweetorial in a while, but last night @etsshow tapped me on the shoulder w a request for a #Medthread re preop evals via #telehealth
The specific https://abs.twimg.com/emoji/v2/... draggable="false" alt="❓" title="Red question mark ornament" aria-label="Emoji: Red question mark ornament">was re assuaging surgeon (& I’ll add anesthesiologist) concerns re the lack of an exam
https://abs.twimg.com/emoji/v2/... draggable="false" alt="❓" title="Red question mark ornament" aria-label="Emoji: Red question mark ornament">was re assuaging surgeon (& I’ll add anesthesiologist) concerns re the lack of an exam
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧵" title="Thread" aria-label="Emoji: Thread">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧵" title="Thread" aria-label="Emoji: Thread">
The specific
2/ Background  https://abs.twimg.com/emoji/v2/... draggable="false" alt="1️⃣" title="Keycap digit one" aria-label="Emoji: Keycap digit one">–telehealth across the board has rapidly expanded given the challenges of providing care while keeping safe distances due to #covid19
https://abs.twimg.com/emoji/v2/... draggable="false" alt="1️⃣" title="Keycap digit one" aria-label="Emoji: Keycap digit one">–telehealth across the board has rapidly expanded given the challenges of providing care while keeping safe distances due to #covid19
We’ve had an incredible amount of institution level support for this at @OHSUnews @OHSUSOM! https://news.ohsu.edu/2020/04/13/ohsu-telehealth-rockets-into-new-era-of-medicine">https://news.ohsu.edu/2020/04/1...
We’ve had an incredible amount of institution level support for this at @OHSUnews @OHSUSOM! https://news.ohsu.edu/2020/04/13/ohsu-telehealth-rockets-into-new-era-of-medicine">https://news.ohsu.edu/2020/04/1...
3/ Background  https://abs.twimg.com/emoji/v2/... draggable="false" alt="2️⃣" title="Keycap digit two" aria-label="Emoji: Keycap digit two">–telehealth for PREOP has been a goal for years w go-live in June.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="2️⃣" title="Keycap digit two" aria-label="Emoji: Keycap digit two">–telehealth for PREOP has been a goal for years w go-live in June.
Why?
To meet the care needs in a large, rural state—many of our sicker/older patients lived very far away & w limited socioeconomic means to get to preop clinic before surgery
Why?
To meet the care needs in a large, rural state—many of our sicker/older patients lived very far away & w limited socioeconomic means to get to preop clinic before surgery
4/ Background  https://abs.twimg.com/emoji/v2/... draggable="false" alt="3️⃣" title="Keycap digit three" aria-label="Emoji: Keycap digit three">—there’s precedence for telehealth for preop visits, esp the work @DrNVKamdar at UCLA
https://abs.twimg.com/emoji/v2/... draggable="false" alt="3️⃣" title="Keycap digit three" aria-label="Emoji: Keycap digit three">—there’s precedence for telehealth for preop visits, esp the work @DrNVKamdar at UCLA
Although there are concerns for rural/socioeconomic disparities with telehealth, the data I’ve seen for preop is encouraging
https://bit.ly/2VTLfSp
https://bit.ly/2VTLfSp&q... href=" https://pdfs.semanticscholar.org/74c1/d0e22df97dd114f92c7f02bd9451169ace24.pdf">https://pdfs.semanticscholar.org/74c1/d0e2...
Although there are concerns for rural/socioeconomic disparities with telehealth, the data I’ve seen for preop is encouraging
https://bit.ly/2VTLfSp
5/ Background  https://abs.twimg.com/emoji/v2/... draggable="false" alt="4️⃣" title="Keycap digit four" aria-label="Emoji: Keycap digit four">–we jumped into PHONE visits in mid-March as soon as OHSU started very proactively rising to the challenge of #covid19—video visits have slowly but ultimately followed
https://abs.twimg.com/emoji/v2/... draggable="false" alt="4️⃣" title="Keycap digit four" aria-label="Emoji: Keycap digit four">–we jumped into PHONE visits in mid-March as soon as OHSU started very proactively rising to the challenge of #covid19—video visits have slowly but ultimately followed
Huge HT to our lead NP @KristenAshNP who has spearheaded this workflow for our clinic
Huge HT to our lead NP @KristenAshNP who has spearheaded this workflow for our clinic
6/ background  https://abs.twimg.com/emoji/v2/... draggable="false" alt="5️⃣" title="Keycap digit five" aria-label="Emoji: Keycap digit five">–this thread won’t focus on regulatory/billing issues, though that’s another conversation (HT the active Down Under convos about this! @GongGasGirl)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="5️⃣" title="Keycap digit five" aria-label="Emoji: Keycap digit five">–this thread won’t focus on regulatory/billing issues, though that’s another conversation (HT the active Down Under convos about this! @GongGasGirl)
It’s a discussion-generating thread re how this type of eval doesn’t substract value from preop care
It’s a discussion-generating thread re how this type of eval doesn’t substract value from preop care
7/ so remember, a preoperative visit is not for “clearance”
It’s to perform a patient-centered ASSESSMENT by learning about the patient in ways that EMPOWER their intraop & postop care—including RISK STRATIFICATION and PREDICTION
It’s to perform a patient-centered ASSESSMENT by learning about the patient in ways that EMPOWER their intraop & postop care—including RISK STRATIFICATION and PREDICTION
8/ most periop experts say that the most important step of a preop evaluation is the HISTORY & PHYSICAL
the 2007 ACC/AHA periop guidelines also emphasize HISTORY....and physical
What is the relative weight we put on history v physical?
the 2007 ACC/AHA periop guidelines also emphasize HISTORY....and physical
What is the relative weight we put on history v physical?
9/ let’s take a step back!
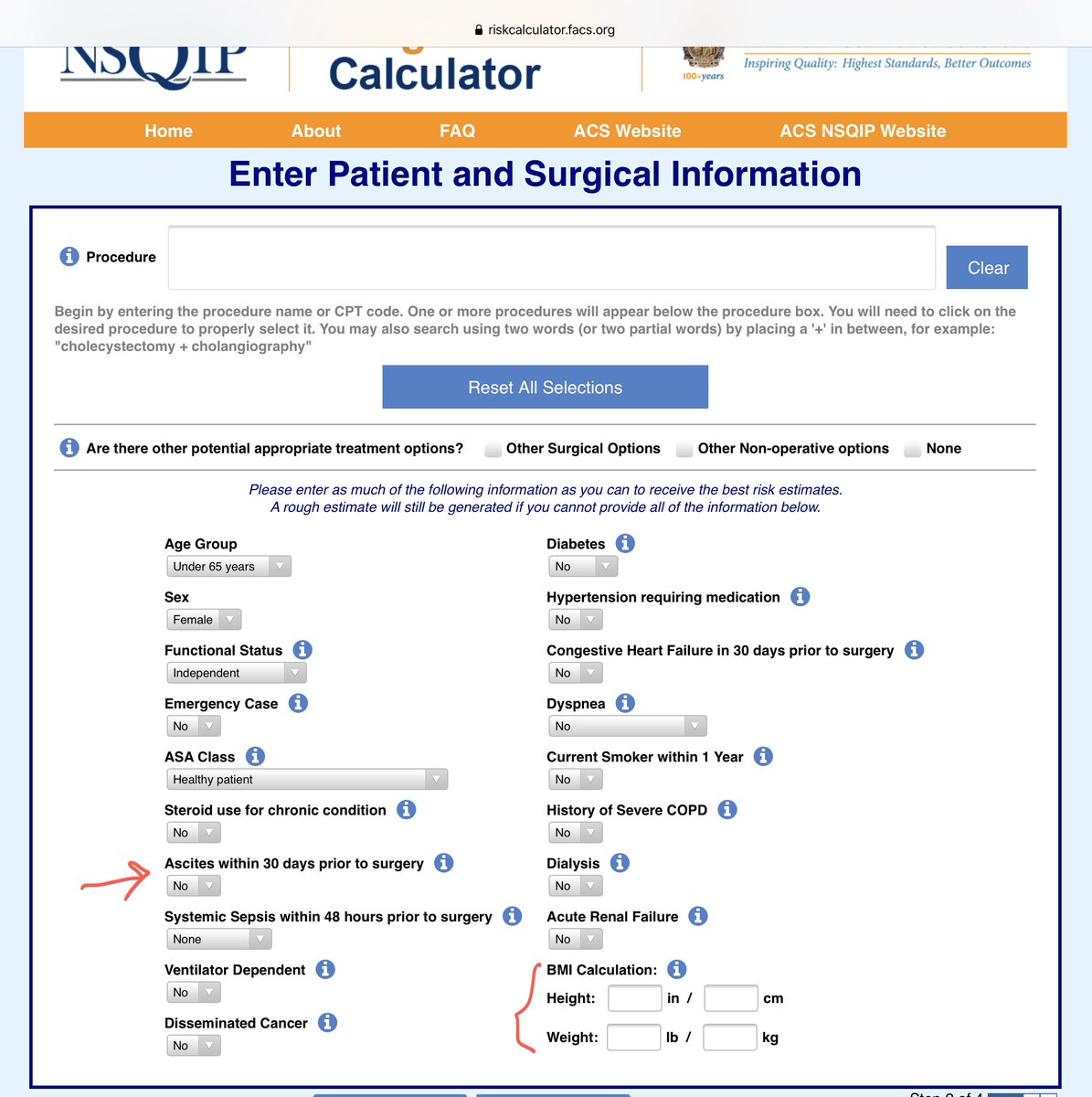
Which of the risk calculators pull in elements of the exam??
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">MICA (Gupta) Cardiac doesn’t
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">MICA (Gupta) Cardiac doesn’t
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">RCRI maybe does? But that’s also history...
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">RCRI maybe does? But that’s also history...
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">NSQIP barely does—you can learn about ascites from history, and BMI can be calculated from prior data
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">NSQIP barely does—you can learn about ascites from history, and BMI can be calculated from prior data
Which of the risk calculators pull in elements of the exam??
10/ the pulmonary calculators don’t include components you can only get from a in-person exam (you can get O2 sat from available prior vitals or patients’ home monitors)
HT @KurtPfeifer for these screen grabs from his prior lecture slides @PeriopSummit
HT @KurtPfeifer for these screen grabs from his prior lecture slides @PeriopSummit
11/ let’s say history >> exam
( @AndreMansoor don’t throw your book at me...)
I believe in the power of the exam—BUT, I also believe in the power of the HISTORY, esp:
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="💠" title="Diamond shape with a dot inside" aria-label="Emoji: Diamond shape with a dot inside">HPI
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💠" title="Diamond shape with a dot inside" aria-label="Emoji: Diamond shape with a dot inside">HPI
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="💠" title="Diamond shape with a dot inside" aria-label="Emoji: Diamond shape with a dot inside">PMHx
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💠" title="Diamond shape with a dot inside" aria-label="Emoji: Diamond shape with a dot inside">PMHx
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="💠" title="Diamond shape with a dot inside" aria-label="Emoji: Diamond shape with a dot inside">med rec
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💠" title="Diamond shape with a dot inside" aria-label="Emoji: Diamond shape with a dot inside">med rec
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="💠" title="Diamond shape with a dot inside" aria-label="Emoji: Diamond shape with a dot inside">ROS
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💠" title="Diamond shape with a dot inside" aria-label="Emoji: Diamond shape with a dot inside">ROS
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="💠" title="Diamond shape with a dot inside" aria-label="Emoji: Diamond shape with a dot inside">Social history—habits AND living situation, esp for older/frailer patients
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💠" title="Diamond shape with a dot inside" aria-label="Emoji: Diamond shape with a dot inside">Social history—habits AND living situation, esp for older/frailer patients
( @AndreMansoor don’t throw your book at me...)
I believe in the power of the exam—BUT, I also believe in the power of the HISTORY, esp:
12/ from the above, I can learn about
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌀" title="Cyclone" aria-label="Emoji: Cyclone">Chest pain
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌀" title="Cyclone" aria-label="Emoji: Cyclone">Chest pain
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌀" title="Cyclone" aria-label="Emoji: Cyclone">Dyspnea
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌀" title="Cyclone" aria-label="Emoji: Cyclone">Dyspnea
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌀" title="Cyclone" aria-label="Emoji: Cyclone">Orthpnea/PND
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌀" title="Cyclone" aria-label="Emoji: Cyclone">Orthpnea/PND
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌀" title="Cyclone" aria-label="Emoji: Cyclone">Edema
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌀" title="Cyclone" aria-label="Emoji: Cyclone">Edema
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌀" title="Cyclone" aria-label="Emoji: Cyclone">Palpitations
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌀" title="Cyclone" aria-label="Emoji: Cyclone">Palpitations
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌀" title="Cyclone" aria-label="Emoji: Cyclone">Exercise capacity
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌀" title="Cyclone" aria-label="Emoji: Cyclone">Exercise capacity
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌀" title="Cyclone" aria-label="Emoji: Cyclone">Use of EtOH/marijuana/tobacco/illegal drugs
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌀" title="Cyclone" aria-label="Emoji: Cyclone">Use of EtOH/marijuana/tobacco/illegal drugs
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌀" title="Cyclone" aria-label="Emoji: Cyclone">ADLs, IADLs
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌀" title="Cyclone" aria-label="Emoji: Cyclone">ADLs, IADLs
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌀" title="Cyclone" aria-label="Emoji: Cyclone">STOP-BANG score (gestimate neck circ from video, or ask collar size!)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌀" title="Cyclone" aria-label="Emoji: Cyclone">STOP-BANG score (gestimate neck circ from video, or ask collar size!)
13/ stay curious
Utilize the power of observation
get exam info via video
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌀" title="Cyclone" aria-label="Emoji: Cyclone">Self-measured vitals (BP cuff, HR monitor, scale)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌀" title="Cyclone" aria-label="Emoji: Cyclone">Self-measured vitals (BP cuff, HR monitor, scale)
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌀" title="Cyclone" aria-label="Emoji: Cyclone">Work of breathing
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌀" title="Cyclone" aria-label="Emoji: Cyclone">Work of breathing
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌀" title="Cyclone" aria-label="Emoji: Cyclone">Hearing
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌀" title="Cyclone" aria-label="Emoji: Cyclone">Hearing
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌀" title="Cyclone" aria-label="Emoji: Cyclone">Head/neck/airway assessment
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌀" title="Cyclone" aria-label="Emoji: Cyclone">Head/neck/airway assessment
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌀" title="Cyclone" aria-label="Emoji: Cyclone">cognitive status
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌀" title="Cyclone" aria-label="Emoji: Cyclone">cognitive status
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌀" title="Cyclone" aria-label="Emoji: Cyclone">edema
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🌀" title="Cyclone" aria-label="Emoji: Cyclone">edema
Bonus points to @AndreMansoor if he can see JVP via telehealth!
Utilize the power of observation
get exam info via video
Bonus points to @AndreMansoor if he can see JVP via telehealth!
14/ how else can you get creative?
is this potentially a WIN?
I woke up to THIS tweet by @adamcifu
Yes—helping med recs
Yes—see people at home
PS— @londyloo tweet re rug assessment in geriatric telehealth visit!
https://twitter.com/londyloo/status/1248237970613841921?s=20
https://twitter.com/londyloo/... href=" https://twitter.com/adamcifu/status/1253674868165525504?s=20">https://twitter.com/adamcifu/... https://twitter.com/adamcifu/status/1253674868165525504">https://twitter.com/adamcifu/...
is this potentially a WIN?
I woke up to THIS tweet by @adamcifu
Yes—helping med recs
Yes—see people at home
PS— @londyloo tweet re rug assessment in geriatric telehealth visit!
https://twitter.com/londyloo/status/1248237970613841921?s=20
15/ speaking of which, there’s a lot of attention right now on preop frailty and geriatric assessments
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">the Edmonton Fraity includes timed get up and go—can you do that with patient in their home??
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">the Edmonton Fraity includes timed get up and go—can you do that with patient in their home??
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">NSQIP has geriatric questions you can answer w/o exam
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">NSQIP has geriatric questions you can answer w/o exam
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">DASI can get asked
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">DASI can get asked
16/ the Minicog has a clock draw which you can do that with patients via video (the Edmonton also includes a clock draw)
HT @Jeanna_BlitzMD for recommending the Blind MoCA
Our clinic team is also using the 5 minute/mini MOCA
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4373962/
https://www.ncbi.nlm.nih.gov/pmc/artic... href=" https://www.mocatest.org/wp-content/uploads/2015/tests-instructions/MoCA-Test-BLIND.pdf">https://www.mocatest.org/wp-conten...
HT @Jeanna_BlitzMD for recommending the Blind MoCA
Our clinic team is also using the 5 minute/mini MOCA
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4373962/
17/ @Jeanna_BlitzMD @Duke_Anesthesia & I have also chatted
about using the AD8, # of animals you can name in a minute, and
30 second chair sit stands (with that, I would watch/listen for dyspnea, too!)
https://www.cdc.gov/steadi/pdf/STEADI-Assessment-30Sec-508.pdf
https://www.cdc.gov/steadi/pd... href=" https://www.alz.org/media/Documents/ad8-dementia-screening.pdf">https://www.alz.org/media/Doc...
about using the AD8, # of animals you can name in a minute, and
30 second chair sit stands (with that, I would watch/listen for dyspnea, too!)
https://www.cdc.gov/steadi/pdf/STEADI-Assessment-30Sec-508.pdf
18/ typically, if I’m leaning towards preop cardiac testing, I’m nearly at that decision before I start my exam
When does the exam really surprise me?
Murmurs—could they have incidental moderate or asymptomatic severe valve disease?
Even the LV assessment recs go by symptoms
When does the exam really surprise me?
Murmurs—could they have incidental moderate or asymptomatic severe valve disease?
Even the LV assessment recs go by symptoms
19/ but what about EKG?
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="1️⃣" title="Keycap digit one" aria-label="Emoji: Keycap digit one">we obtain too many preop EKGs that don’t change management
https://abs.twimg.com/emoji/v2/... draggable="false" alt="1️⃣" title="Keycap digit one" aria-label="Emoji: Keycap digit one">we obtain too many preop EKGs that don’t change management
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="2️⃣" title="Keycap digit two" aria-label="Emoji: Keycap digit two">better EHR interoperability may provide access to prior
https://abs.twimg.com/emoji/v2/... draggable="false" alt="2️⃣" title="Keycap digit two" aria-label="Emoji: Keycap digit two">better EHR interoperability may provide access to prior
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="3️⃣" title="Keycap digit three" aria-label="Emoji: Keycap digit three">obtain on surgery day
https://abs.twimg.com/emoji/v2/... draggable="false" alt="3️⃣" title="Keycap digit three" aria-label="Emoji: Keycap digit three">obtain on surgery day
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="4️⃣" title="Keycap digit four" aria-label="Emoji: Keycap digit four">banter already happening re the role of apple watches and other wearables w telehealth
https://abs.twimg.com/emoji/v2/... draggable="false" alt="4️⃣" title="Keycap digit four" aria-label="Emoji: Keycap digit four">banter already happening re the role of apple watches and other wearables w telehealth
https://twitter.com/nickkotch/status/1251201342070312960?s=20">https://twitter.com/nickkotch... https://twitter.com/nickkotch/status/1251201342070312960">https://twitter.com/nickkotch...
https://twitter.com/nickkotch/status/1251201342070312960?s=20">https://twitter.com/nickkotch... https://twitter.com/nickkotch/status/1251201342070312960">https://twitter.com/nickkotch...
20/ btw, this is a really cool share by @EricTopol about how to obtain a 12 lead via Apple Watch (note the date—pre covid)
https://twitter.com/EricTopol/status/1199088326633914368?s=20">https://twitter.com/EricTopol... https://twitter.com/erictopol/status/1199088326633914368">https://twitter.com/erictopol...
https://twitter.com/EricTopol/status/1199088326633914368?s=20">https://twitter.com/EricTopol... https://twitter.com/erictopol/status/1199088326633914368">https://twitter.com/erictopol...
21/ what about Labs?
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="1️⃣" title="Keycap digit one" aria-label="Emoji: Keycap digit one">we probably obtain too many preop labs that don’t change management
https://abs.twimg.com/emoji/v2/... draggable="false" alt="1️⃣" title="Keycap digit one" aria-label="Emoji: Keycap digit one">we probably obtain too many preop labs that don’t change management
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="2️⃣" title="Keycap digit two" aria-label="Emoji: Keycap digit two">better EHR interoperability may provide access to prior & recent one
https://abs.twimg.com/emoji/v2/... draggable="false" alt="2️⃣" title="Keycap digit two" aria-label="Emoji: Keycap digit two">better EHR interoperability may provide access to prior & recent one
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="3️⃣" title="Keycap digit three" aria-label="Emoji: Keycap digit three">work with your team to create a pathway for labs on the morning of surgery esp ones with restrictions on age (T&S)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="3️⃣" title="Keycap digit three" aria-label="Emoji: Keycap digit three">work with your team to create a pathway for labs on the morning of surgery esp ones with restrictions on age (T&S)
22/ but does all this still risk day-of-surgery cancellation?
Yes...but...resource utilization is dramatically different now & the risk of COVID19 spread is real
The risk/benefit equation regarding DOS cancellations seems to have shifted if patients (& clinicians) stayed home
Yes...but...resource utilization is dramatically different now & the risk of COVID19 spread is real
The risk/benefit equation regarding DOS cancellations seems to have shifted if patients (& clinicians) stayed home
23/ remember also, the surgeries that are proceeding right now are likely the ones that are least elective such that delay/postponement for cardiac testing or other optimization may not additionally change management
24/ create a triage system to escalate to an occasional inperson visit based on the through HISTORY and assessment/observations during televisit...
Create processes to check in frequently with local stakeholders—how’s it going? Have there been surgery cancellations in the PACU?
Create processes to check in frequently with local stakeholders—how’s it going? Have there been surgery cancellations in the PACU?
FIN
this is a rapidly expanding practice area...
is it the same? No
Is it worth the innovative? Yes
Turn to #medtwitter to share experiences—And I anticipate a lot of discussion & reflections re this in the next year as we move into the new “normal” state of covid
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧶" title="Yarn" aria-label="Emoji: Yarn">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧶" title="Yarn" aria-label="Emoji: Yarn">
this is a rapidly expanding practice area...
is it the same? No
Is it worth the innovative? Yes
Turn to #medtwitter to share experiences—And I anticipate a lot of discussion & reflections re this in the next year as we move into the new “normal” state of covid

 Read on Twitter
Read on Twitter —there’s precedence for telehealth for preop visits, esp the work @DrNVKamdar at UCLA Although there are concerns for rural/socioeconomic disparities with telehealth, the data I’ve seen for preop is encouraging https://bit.ly/2VTLfSp&q... href=" https://pdfs.semanticscholar.org/74c1/d0e22df97dd114f92c7f02bd9451169ace24.pdf">https://pdfs.semanticscholar.org/74c1/d0e2..." title="4/ Background https://abs.twimg.com/emoji/v2/... draggable="false" alt="3️⃣" title="Keycap digit three" aria-label="Emoji: Keycap digit three">—there’s precedence for telehealth for preop visits, esp the work @DrNVKamdar at UCLA Although there are concerns for rural/socioeconomic disparities with telehealth, the data I’ve seen for preop is encouraging https://bit.ly/2VTLfSp&q... href=" https://pdfs.semanticscholar.org/74c1/d0e22df97dd114f92c7f02bd9451169ace24.pdf">https://pdfs.semanticscholar.org/74c1/d0e2..." class="img-responsive" style="max-width:100%;"/>
—there’s precedence for telehealth for preop visits, esp the work @DrNVKamdar at UCLA Although there are concerns for rural/socioeconomic disparities with telehealth, the data I’ve seen for preop is encouraging https://bit.ly/2VTLfSp&q... href=" https://pdfs.semanticscholar.org/74c1/d0e22df97dd114f92c7f02bd9451169ace24.pdf">https://pdfs.semanticscholar.org/74c1/d0e2..." title="4/ Background https://abs.twimg.com/emoji/v2/... draggable="false" alt="3️⃣" title="Keycap digit three" aria-label="Emoji: Keycap digit three">—there’s precedence for telehealth for preop visits, esp the work @DrNVKamdar at UCLA Although there are concerns for rural/socioeconomic disparities with telehealth, the data I’ve seen for preop is encouraging https://bit.ly/2VTLfSp&q... href=" https://pdfs.semanticscholar.org/74c1/d0e22df97dd114f92c7f02bd9451169ace24.pdf">https://pdfs.semanticscholar.org/74c1/d0e2..." class="img-responsive" style="max-width:100%;"/>



 MICA (Gupta) Cardiac doesn’thttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">RCRI maybe does? But that’s also history...https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">NSQIP barely does—you can learn about ascites from history, and BMI can be calculated from prior data" title="9/ let’s take a step back!Which of the risk calculators pull in elements of the exam??https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">MICA (Gupta) Cardiac doesn’thttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">RCRI maybe does? But that’s also history...https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">NSQIP barely does—you can learn about ascites from history, and BMI can be calculated from prior data">
MICA (Gupta) Cardiac doesn’thttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">RCRI maybe does? But that’s also history...https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">NSQIP barely does—you can learn about ascites from history, and BMI can be calculated from prior data" title="9/ let’s take a step back!Which of the risk calculators pull in elements of the exam??https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">MICA (Gupta) Cardiac doesn’thttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">RCRI maybe does? But that’s also history...https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">NSQIP barely does—you can learn about ascites from history, and BMI can be calculated from prior data">
 MICA (Gupta) Cardiac doesn’thttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">RCRI maybe does? But that’s also history...https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">NSQIP barely does—you can learn about ascites from history, and BMI can be calculated from prior data" title="9/ let’s take a step back!Which of the risk calculators pull in elements of the exam??https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">MICA (Gupta) Cardiac doesn’thttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">RCRI maybe does? But that’s also history...https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">NSQIP barely does—you can learn about ascites from history, and BMI can be calculated from prior data">
MICA (Gupta) Cardiac doesn’thttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">RCRI maybe does? But that’s also history...https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">NSQIP barely does—you can learn about ascites from history, and BMI can be calculated from prior data" title="9/ let’s take a step back!Which of the risk calculators pull in elements of the exam??https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">MICA (Gupta) Cardiac doesn’thttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">RCRI maybe does? But that’s also history...https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">NSQIP barely does—you can learn about ascites from history, and BMI can be calculated from prior data">
 MICA (Gupta) Cardiac doesn’thttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">RCRI maybe does? But that’s also history...https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">NSQIP barely does—you can learn about ascites from history, and BMI can be calculated from prior data" title="9/ let’s take a step back!Which of the risk calculators pull in elements of the exam??https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">MICA (Gupta) Cardiac doesn’thttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">RCRI maybe does? But that’s also history...https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">NSQIP barely does—you can learn about ascites from history, and BMI can be calculated from prior data">
MICA (Gupta) Cardiac doesn’thttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">RCRI maybe does? But that’s also history...https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">NSQIP barely does—you can learn about ascites from history, and BMI can be calculated from prior data" title="9/ let’s take a step back!Which of the risk calculators pull in elements of the exam??https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">MICA (Gupta) Cardiac doesn’thttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">RCRI maybe does? But that’s also history...https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">NSQIP barely does—you can learn about ascites from history, and BMI can be calculated from prior data">



 the Edmonton Fraity includes timed get up and go—can you do that with patient in their home?? https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">NSQIP has geriatric questions you can answer w/o examhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">DASI can get asked" title="15/ speaking of which, there’s a lot of attention right now on preop frailty and geriatric assessmentshttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">the Edmonton Fraity includes timed get up and go—can you do that with patient in their home?? https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">NSQIP has geriatric questions you can answer w/o examhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">DASI can get asked">
the Edmonton Fraity includes timed get up and go—can you do that with patient in their home?? https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">NSQIP has geriatric questions you can answer w/o examhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">DASI can get asked" title="15/ speaking of which, there’s a lot of attention right now on preop frailty and geriatric assessmentshttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">the Edmonton Fraity includes timed get up and go—can you do that with patient in their home?? https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">NSQIP has geriatric questions you can answer w/o examhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">DASI can get asked">
 the Edmonton Fraity includes timed get up and go—can you do that with patient in their home?? https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">NSQIP has geriatric questions you can answer w/o examhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">DASI can get asked" title="15/ speaking of which, there’s a lot of attention right now on preop frailty and geriatric assessmentshttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">the Edmonton Fraity includes timed get up and go—can you do that with patient in their home?? https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">NSQIP has geriatric questions you can answer w/o examhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">DASI can get asked">
the Edmonton Fraity includes timed get up and go—can you do that with patient in their home?? https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">NSQIP has geriatric questions you can answer w/o examhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">DASI can get asked" title="15/ speaking of which, there’s a lot of attention right now on preop frailty and geriatric assessmentshttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">the Edmonton Fraity includes timed get up and go—can you do that with patient in their home?? https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">NSQIP has geriatric questions you can answer w/o examhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">DASI can get asked">
 the Edmonton Fraity includes timed get up and go—can you do that with patient in their home?? https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">NSQIP has geriatric questions you can answer w/o examhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">DASI can get asked" title="15/ speaking of which, there’s a lot of attention right now on preop frailty and geriatric assessmentshttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">the Edmonton Fraity includes timed get up and go—can you do that with patient in their home?? https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">NSQIP has geriatric questions you can answer w/o examhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">DASI can get asked">
the Edmonton Fraity includes timed get up and go—can you do that with patient in their home?? https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">NSQIP has geriatric questions you can answer w/o examhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">DASI can get asked" title="15/ speaking of which, there’s a lot of attention right now on preop frailty and geriatric assessmentshttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">the Edmonton Fraity includes timed get up and go—can you do that with patient in their home?? https://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">NSQIP has geriatric questions you can answer w/o examhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✳️" title="Eight spoked asterisk" aria-label="Emoji: Eight spoked asterisk">DASI can get asked">
 https://www.mocatest.org/wp-conten..." title="16/ the Minicog has a clock draw which you can do that with patients via video (the Edmonton also includes a clock draw)HT @Jeanna_BlitzMD for recommending the Blind MoCAOur clinic team is also using the 5 minute/mini MOCA https://www.ncbi.nlm.nih.gov/pmc/artic... href=" https://www.mocatest.org/wp-content/uploads/2015/tests-instructions/MoCA-Test-BLIND.pdf">https://www.mocatest.org/wp-conten..." class="img-responsive" style="max-width:100%;"/>
https://www.mocatest.org/wp-conten..." title="16/ the Minicog has a clock draw which you can do that with patients via video (the Edmonton also includes a clock draw)HT @Jeanna_BlitzMD for recommending the Blind MoCAOur clinic team is also using the 5 minute/mini MOCA https://www.ncbi.nlm.nih.gov/pmc/artic... href=" https://www.mocatest.org/wp-content/uploads/2015/tests-instructions/MoCA-Test-BLIND.pdf">https://www.mocatest.org/wp-conten..." class="img-responsive" style="max-width:100%;"/>




