Donna Farber is an immunologist who studies the immune response to respiratory viruses, lung immunity, and human immunology. The COVID-19 and Immunology webinar starts now! Follow along #FarberCOVID19
COVID-19 symptom breakdown (based on 72,314 cases in China)
-1% asymptomatic
-81% acute disease w/out pneumonia
-14% severe disease
-5% critical
Case mortality=2.3% (*23 times more lethal than influenza)
#FarberCOVID19
-1% asymptomatic
-81% acute disease w/out pneumonia
-14% severe disease
-5% critical
Case mortality=2.3% (*23 times more lethal than influenza)
#FarberCOVID19
Risk factors for severe disease: middle to old age; male; comorbidities (heart disease, diabetes, hypertension)
Less than 10% of cases are under 30 years old.
Treatment is supportive care, no anti-viral or vaccine therapies #FarberCOVID19
Less than 10% of cases are under 30 years old.
Treatment is supportive care, no anti-viral or vaccine therapies #FarberCOVID19
SARS-CoV2 belongs to the coronaviridae family. These are enveloped, non-segmented RNA viruses with large genomes. #FarberCOVID19
Other coronaviruses of note:
-HCoV-229E: seasonal, self-limiting respiratory illness (15-20% of common colds)
-SARS-CoV: 2002-3 outbreak, severe, low transmission, 10% mortality
#FarberCOVID19
-HCoV-229E: seasonal, self-limiting respiratory illness (15-20% of common colds)
-SARS-CoV: 2002-3 outbreak, severe, low transmission, 10% mortality
#FarberCOVID19
-MERS-CoV: 2013-14 outbreak, 855 cases and 333 deaths; self-limiting, transmission from camels
-MHV (murine Hepatitis virus): highly contagious in mice, common problem in vivariums #FarberCOVID19
-MHV (murine Hepatitis virus): highly contagious in mice, common problem in vivariums #FarberCOVID19
How is SARS-CoV2 different? Like MHV, COVID-19 has a high transmission rate. But viral shedding starts when you& #39;re asymptomatic—no symptoms. That didn& #39;t happen with the SARS outbreak in & #39;02, shedding happened when people were feeling sick. #FarberCOVID19
That also happens with influenza. You feel so sick you stay home. You don& #39;t shed and spread.
With COVID-19, people are walking around w/out symptoms shedding the virus. *Transmission rate: 1 person infects 2-2.5. In some, 1 person can infect 5-6 individuals. #FarberCOVID19
With COVID-19, people are walking around w/out symptoms shedding the virus. *Transmission rate: 1 person infects 2-2.5. In some, 1 person can infect 5-6 individuals. #FarberCOVID19
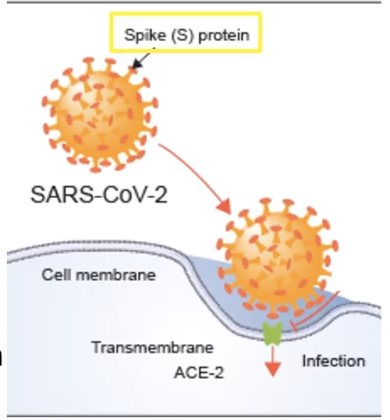
SARS-CoV-2 infects on the surface. Using its spike proteins to bind and recognize the cellular receptor. This is how the virus gets into the cells. #FarberCOVID19
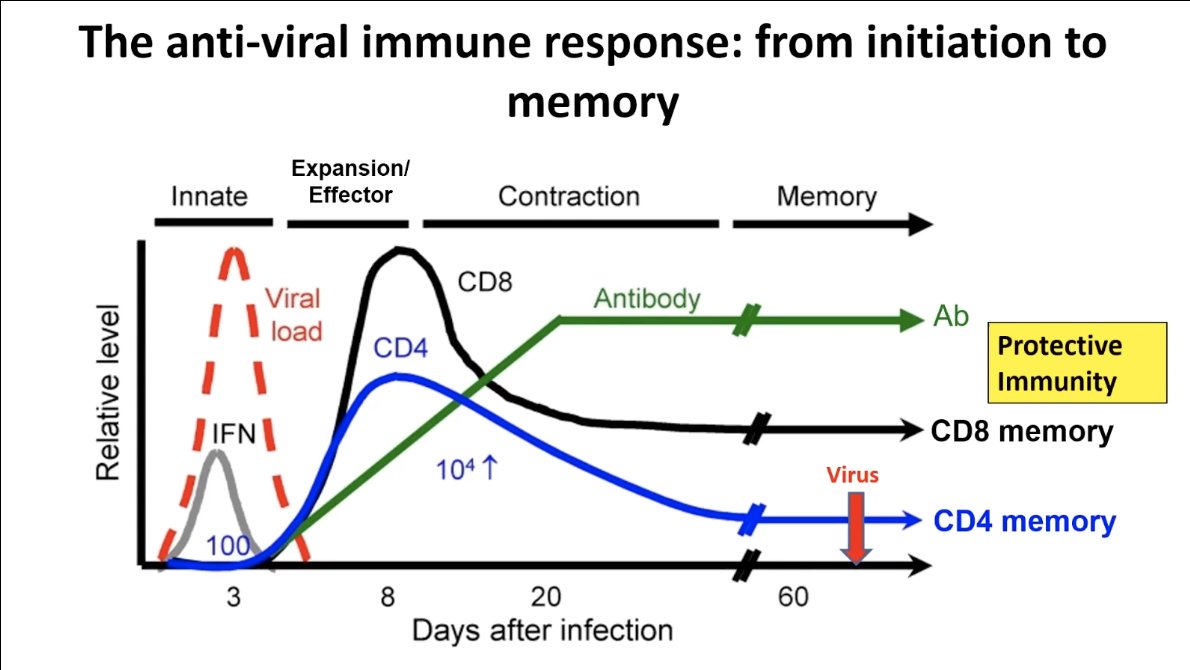
When a virus gets into a cell, the anti-viral immune response can be divided into different phases. Usually, the virus infects and starts to replicate within the cells (logarithmic increase of viral load). #FarberCOVID19
The host responds first with innate cells, including cells the virus infects. This is really important for early control of viral load. #FarberCOVID19
Then initiates the adaptive immune response (T cells, CD4, CD8, and B cells that produce antibody). Expanding rapidly, usually peaking a week after infection right when the viral load is coming down. #FarberCOVID19
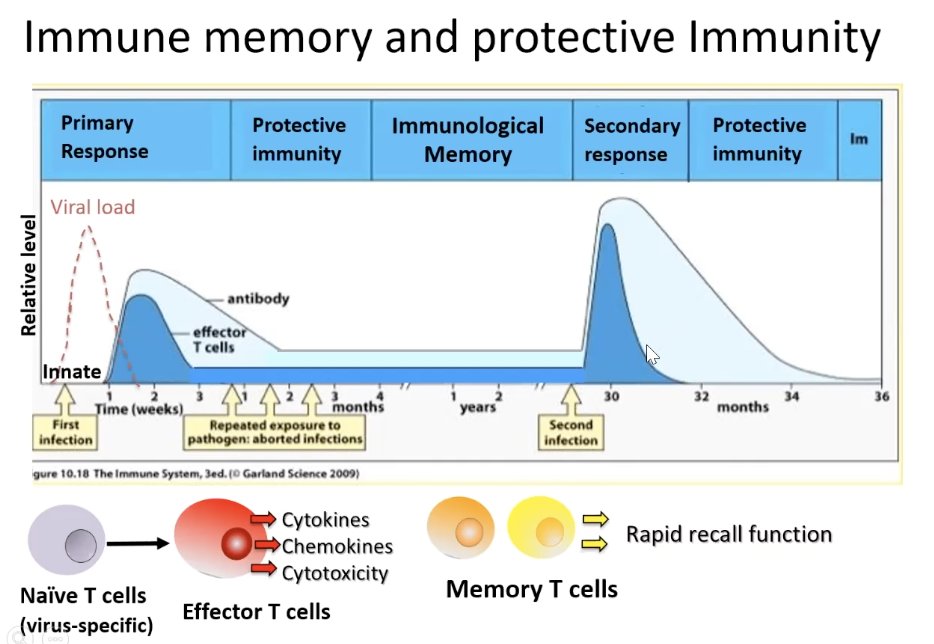
Antibody always appears later. The peak of the antibody is a few weeks after infection. Once infection is cleared, the expansion of T cells will contract and a lot will die bc you don& #39;t need them anymore. But they don& #39;t go down to baseline. #FarberCOVID19
You actually maintain a population of expanded CD4 and CD8 cells and antibody that comprise the immunological memory. Giving you protective immunity against the virus in the future. #FarberCOVID19
This immunological memory is what happens in respiratory viruses like influenza. But what we don& #39;t yet know what happens with SARS-C0V2. #FarberCOVID19
SARS-C0V2 is so new, research is just now starting to rapidly come out, some unpublished or in pre-print (not yet peer reviewed), and ranges in quality. The point of this webinar is to summarize what is known about COVID-19 & share data from controlled experiments. #FarberCOVID19
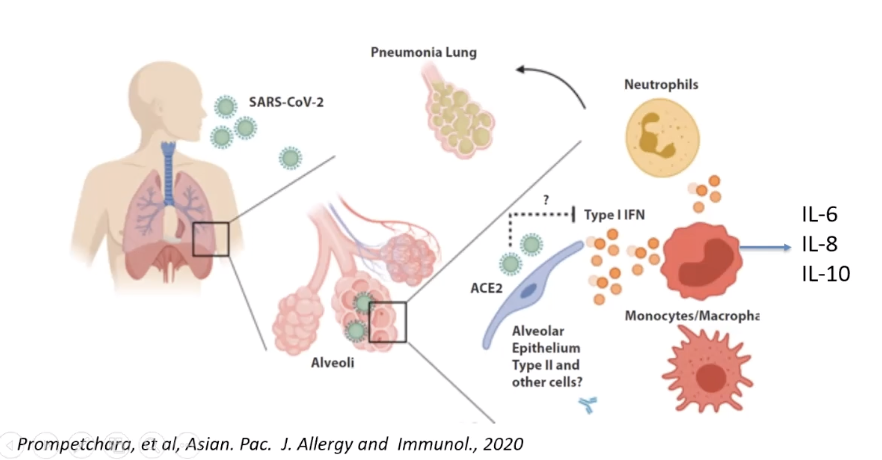
Back to the innate response to viral infection (first phase of immunologic response): Type I Interferons
-produced by infected cells, triggers pathways to inhibit viral cell replication in the cell, and trigger recruitment & activation of innate cells. #FarberCOVID19
-produced by infected cells, triggers pathways to inhibit viral cell replication in the cell, and trigger recruitment & activation of innate cells. #FarberCOVID19
So virus infects lungs > infect epithelial cells that produce Type I IFN > this will recruit monocytes, macrophages, neutrophils & NK cells.
*What we know abt SARS-CoV2 & SARS 2003: they do not induce Type I IFN resulting in delayed & dysregulated innate immunity #FarberCOVID19
*What we know abt SARS-CoV2 & SARS 2003: they do not induce Type I IFN resulting in delayed & dysregulated innate immunity #FarberCOVID19
So with COVID-19, from the very beginning there are limits and alterations in the way SARS-CoV2 is recognized by the immune system. #FarberCOVID19
What about the next phase: adaptive immunity? Primary T cell response is essential to get rid of the virus. #FarberCOVID19
Here& #39;s a model of T cell response to influenza infection. In the lymph nodes, the naive T cells will activate and clonally expand and differentiate to infector cells that will traffic to the lung and get rid of infected epithelial cells. #FarberCOVID19
At the same time, T cells will also coordinate and help B cells to be activated and produce virus-specific antibodies. So it& #39;s the coordinated adaptive immunity of T cells and antibodies that effectively clear this virus. But T cells direct the show. #FarberCOVID19
*T cell response to SARS-CoV2 is not yet known. We can assume that we are getting a T cell response bc of antibodies. And we know that T cells are going to the lungs. #FarberCOVID19
Now to the B cell response: antibodies. T cells get B cells to the virus > B cells differentiate to antibody-secreting plasma cells > antibodies then have multiple effector functions to get rid of the pathogen. #FarberCOVID19
antibodies can:
-neutralize microbes and toxins by preventing virus from entering cells
-mark the pathogen for destruction by macrophages
-fix and recruit complements (serum protein), the cleanup function #FarberCOVID19
-neutralize microbes and toxins by preventing virus from entering cells
-mark the pathogen for destruction by macrophages
-fix and recruit complements (serum protein), the cleanup function #FarberCOVID19
The reason we are so focused on the antibody response to SARS-CoV2 is bc it& #39;s something we can measure. We can& #39;t measure T cells in the lung but we can measure antibody immunity in the serum. #FarberCOVID19
With COVID-19, people do mount antibodies to this virus, and the antibody response can peak anywhere from 10 days to two weeks after symptom onset, both in mild and severe cases. Yet, some individuals do not develop a detectable antibody response. #FarberCOVID19
COVID-19 is a prolonged disease, so this immune response is really raging against the virus for weeks. #FarberCOVID19
What going on w/ this prolonged severity? Or when someone looks like they& #39;re getting better & then all of the sudden crashes? Is it the virus or is the immune response raging out of control?
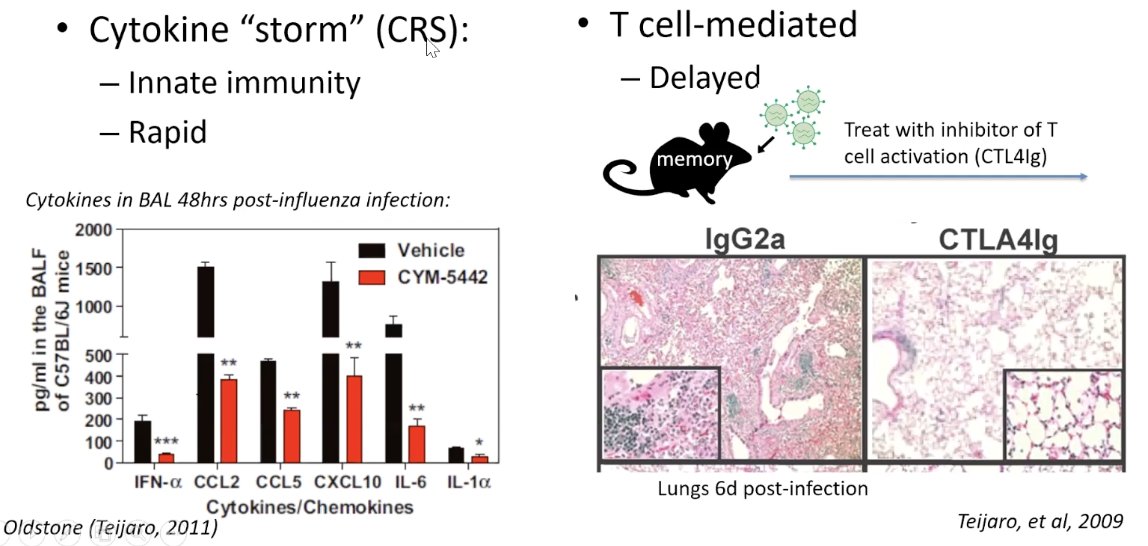
Well, there are 2 types of immunopathology (ex in influenza mice model): #FarberCOVID19
Well, there are 2 types of immunopathology (ex in influenza mice model): #FarberCOVID19
It could be very important to define the immunopathology in order to develop ways to treat the symptoms of this prolonged disease. #FarberCOVID19
There is cytokine release syndrome (CRS) in some individuals with COVID-19. Right now, this is being treated with Tocilizumab (an anti-IL-6 receptor) and has been shown to help people recover. #FarberCOVID19
The problem is that all the trials now are one-arm trials. Meaning there is only the treatment group and not the control group. So the jury is still out, but people are being treated with this @nyphospital and clinical trials are underway. #FarberCOVID19
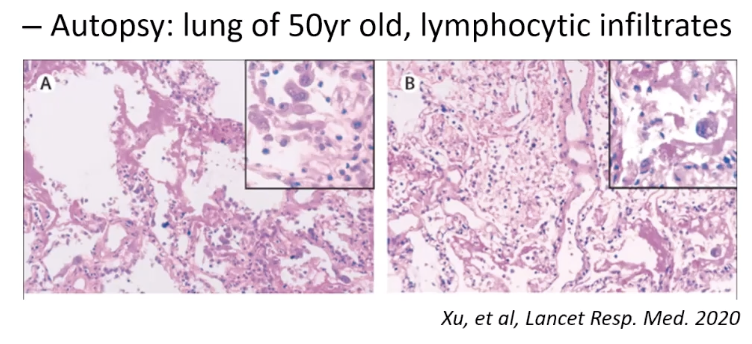
We also know that in some of the cases where one looked to be doing okay and then crashed, we& #39;re seeing lymphocytic infiltrates. In this autopsy, you& #39;re seeing a lack of airways a lot of T cells. #FarberCOVID19
So we need to know:
-What are the immune correlates of disease severity?
-When do they occur?
#FarberCOVID19
-What are the immune correlates of disease severity?
-When do they occur?
#FarberCOVID19
It may be appropriate to treat for cytokine release syndrome early on in infection, and then later it may be better to treat the lymphocytic part of this with modulators that act like T cells. #FarberCOVID19
One of the advantages now is that we have a lot of immune modulators on the market that can target different aspects. But we still don& #39;t yet know exactly what& #39;s going on with SARS-CoV2, we need to look at the respiratory environment for answers. #FarberCOVID19
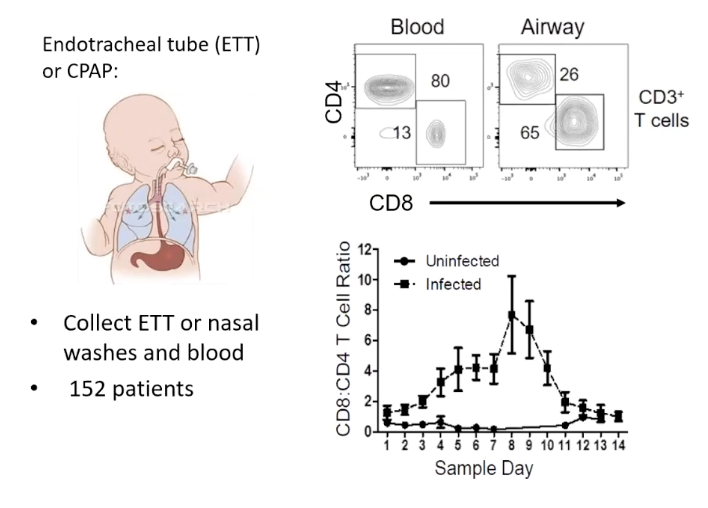
In collecting samples from the respiratory tract in 152 pediatric patients with respiratory virus, we& #39;ve found a lot of T cells in these airway samples. And the nature of these T cells in the airway is very different from blood. #FarberCOVID19
Even though you can readily sample blood, it& #39;s not always very representative of what& #39;s going on in the respiratory environment. In fact, most of the time it& #39;s not representative at all. #FarberCOVID19
What we& #39;ve found is this increase in T cell content correlates with lung injury and inversely with viral load (in pediatric patients with respiratory virus, non COVID-19). So the T cells are clearing the virus, but they& #39;re also causing more damage. #FarberCOVID19
So if we& #39;re to use this to design a therapy for COVID-19, you want to modulate that T cell response to get that sweet spot. Where they& #39;re mediating protection but not causing tissue damage. #FarberCOVID19
Using this approach to understand respiratory immunity in COVID-19 patients, we need to start with these critical questions:
#FarberCOVID19
#FarberCOVID19
-Is viral clearance associated w/ a particular composition of innate and adaptive cell subsets in the airways?
-What are the immune correlates w/ lung injury or other clinical measures of disease severity and how differ w/ age or male versus female? #FarberCOVID19
-What are the immune correlates w/ lung injury or other clinical measures of disease severity and how differ w/ age or male versus female? #FarberCOVID19
We are now doing longitudinal analysis of endotracheal tube washes versus blood in COVID-19 patients (like what is shown in the above pediatric study). #FarberCOVID19
We are:
-obtaining respiratory samples and blood daily from intubated COVID-19 patients in ICU and PICU
-assessing immune cell composition, viral load, transcriptomics, cytokines/chemokines and antibodies
-correlating immune parameters w/ clinical measures #FarberCOVID19
-obtaining respiratory samples and blood daily from intubated COVID-19 patients in ICU and PICU
-assessing immune cell composition, viral load, transcriptomics, cytokines/chemokines and antibodies
-correlating immune parameters w/ clinical measures #FarberCOVID19
In our first enrolled patient (who has fortunately recovered), we& #39;ve done 6 consecutive days of paired airway and blood, and we can tell you that there are many immune cells in airways. #FarberCOVID19
It& #39;s too early to call right now, but this is feasible and we will be able to follow the immune response over time and collect as much data as possible. #FarberCOVID19
What about immune memory & protective immunity? When you meet the virus again, you should get an immediate mobilization of memory T cells & antibody response that protects you. *That is the goal, & what we hope those recovered from COVID-19 have, but we don& #39;t know. #FarberCOVID19
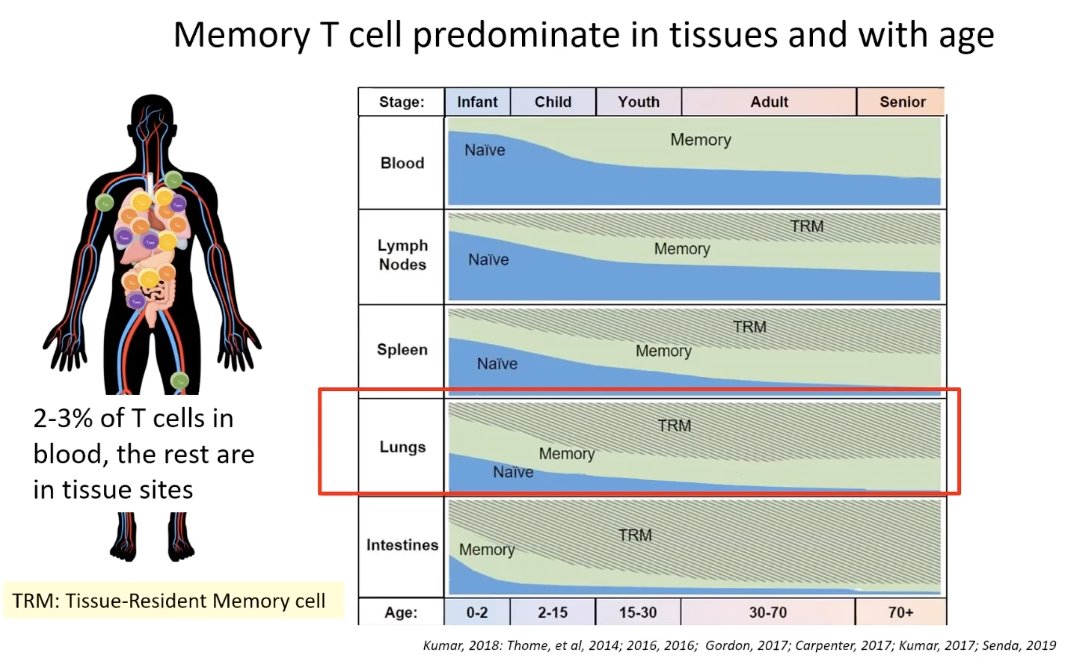
That takes us to the memory T cell. What is the nature of the memory T cell?
-the majority of T cells reside in tissue sites, only 2-3% in blood
-T cells also accumulate rapidly with age
#FarberCOVID19
-the majority of T cells reside in tissue sites, only 2-3% in blood
-T cells also accumulate rapidly with age
#FarberCOVID19
Most of the memory you& #39;ll find is TRM, tissue-resident memory cells. The lungs, throughout most of our lives, are mostly TRM. Representing all the respiratory pathogens that we& #39;ve encountered over our lives. #FarberCOVID19
As you can see in the previous graphic, TRM dominates in people over the age of 30. We don& #39;t have as many naive cells or response to new pathogens. This is the exact group that suffers most from COVID-19. #FarberCOVID19
Children and young adults are doing well and not getting COVID-19 bc they have the new T cells and their immune response is designed to handle new pathogens. So, the circumstantial evidence points to a T cell needed immunity being the correlate of protection. #FarberCOVID19
In the lab, we& #39;ve found that resident memory T cells (TRM) provide optimal protective immunity to respiratory illness. The TRM actually stands on guard in the lungs. Take SARS-CoV, it was airway memory CD4 T cells that protected against infection. #FarberCOVID19
So, the big question— What about a vaccine for COVID-19?
For a vaccine, we need to identify the protective correlate: specific immune response to a vaccine closely associated w/ protection against infection, disease. #FarberCOVID19
For a vaccine, we need to identify the protective correlate: specific immune response to a vaccine closely associated w/ protection against infection, disease. #FarberCOVID19
The existing vaccine strategies include:
-inactive vaccine (ex: polio, Hep A)
-subunit vaccine (ex: Hep B, pertussis, HPV)
-live, attenuated vaccine (ex: measles, yellow fever) #FarberCOVID19
-inactive vaccine (ex: polio, Hep A)
-subunit vaccine (ex: Hep B, pertussis, HPV)
-live, attenuated vaccine (ex: measles, yellow fever) #FarberCOVID19
Most anti-viral vaccines work by neutralizing antibodies and block the virus& #39;s ability to infect. But for some infectious diseases, like HIV/AIDS, Hep C, despite best efforts it doesn& #39;t always work. #FarberCOVID19
Currently, there are no vaccines for human coronaviruses which means there is nothing to reference in creating a COVID-19 vaccine. As of now, there are 52 strategies currently in development, some in trials. #FarberCOVID19
Most COVID-19 viral strategies are focusing on the spiked protein, the receptor the virus uses to get into the cell and blocking that protein. #FarberCOVID19
There are also viral vectors used to express the Spike protein. This kind of approach has been used successfully. Recently, with Ebola, where they expressed the subunit of Ebola virus. #FarberCOVID19
That strategy for COVID-19 is now being made by several companies. And some have said that vaccine formulation will be ready in a few months. But how can we predict if this will be successful with no ongoing trials in humans? #FarberCOVID19
We can look at the trials in MERS virus in camels (highly lethal w/ zoonotic transmission). One approach is to vaccinate the animal, like we do with rabies in our pets. #FarberCOVID19
The trial takes a naive group and previously infected group, gives a few booster shots, and then does an infectious challenge. Much like us with COVID-19, placing infected and not infected in the same space. #FarberCOVID19
In the MERS trial, the camels bests able to protect against infection and respond to the vaccine were animals that were already infected. This suggests that the immunity is cumulative. Maybe having some seropositivity will help, and continue to build up. #FarberCOVID19
Of course, we are not camels, so this doesn& #39;t show what a Spiked protein will do, but important to note. #FarberCOVID19
But we do know that Lung TRM will mediate protection to respiratory virus and there are certain vaccines that will give you these lung tissue-resident membranes. #FarberCOVID19
In a mice study comparing injectable inactivated flu vaccine with intranasal live-attenuated flu vaccine, T cells were only found in those with live-attenuated vaccine, but humoral immunity was higher with injectable. Then underwent viral challenge. #FarberCOVID19
In the viral challenge, mice who either already had the flu or got the live-attenuated vaccine were fully protected. Those with injectable inactivated or unvaccinated had significant morbidity due to viral infection. So, what does this mean? #FarberCOVID19
Vaccines can generate this immunity but you need to go to the site, and you need that attenuated low-level infection. #FarberCOVID19
In Summary:
1. Everyone is/was naive to SARS-CoV2. Children fare better bc they have more new T cells to respond to new pathogens. #FarberCOVID19
1. Everyone is/was naive to SARS-CoV2. Children fare better bc they have more new T cells to respond to new pathogens. #FarberCOVID19
2. The primary immune response in adults to COVID-19 is dysregulated and not efficiently protective. #FarberCOVID19
3. Vaccines—unclear whether antibody correlates with protection. Targeting humoral immunity may have limited efficacy in preventing disease. (Anti-virals may provide alternate or additive protection) #FarberCOVID19
4. Local respiratory environment is important for immunity and monitoring immunopathology. Local vaccination with live-attenuated strains for protection is a strategy that should be pursued. And targeting at the appropriate stage of disease. #FarberCOVID19
That concludes the COVID-19 and Immunology webinar with Dr. Farber. Thanks for following along! We will share additional materials and video details when available. #FarberCOVID19

 Read on Twitter
Read on Twitter