#COVID19 #Tweetorial about infective endocarditis (IE) and TEE use in these times. @OKhaliqueMD @HeartOTXHeartMD @RonBlankstein @DocStrom @chiarabd @NitiCardio
As most of us know, we are in a pandemic, with a highly contagious disease that has caused exponential outbreak levels worldwide. Cleanest data set from Diamond Princess Cruise Ship data, suggests an R0=2.28 (reproductive number) of https://www.sciencedirect.com/science/article/pii/S1201971220300916?via%3Dihub">https://www.sciencedirect.com/science/a...
In an usual practice we do TEE freely, and without many constraints, but during these times, we have to think more about what is the risk of exposure as there are many asymptomatic individuals that could be contagious and produce high viral loads. https://www.nejm.org/doi/full/10.1056/NEJMc2001468">https://www.nejm.org/doi/full/...
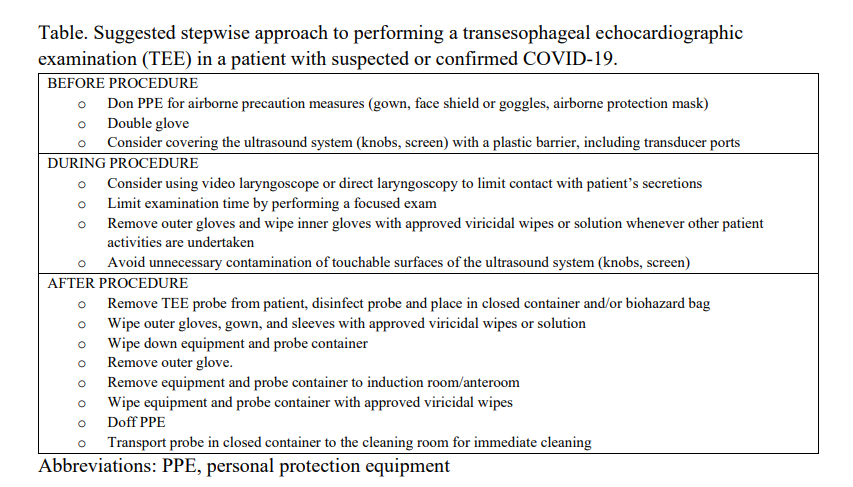
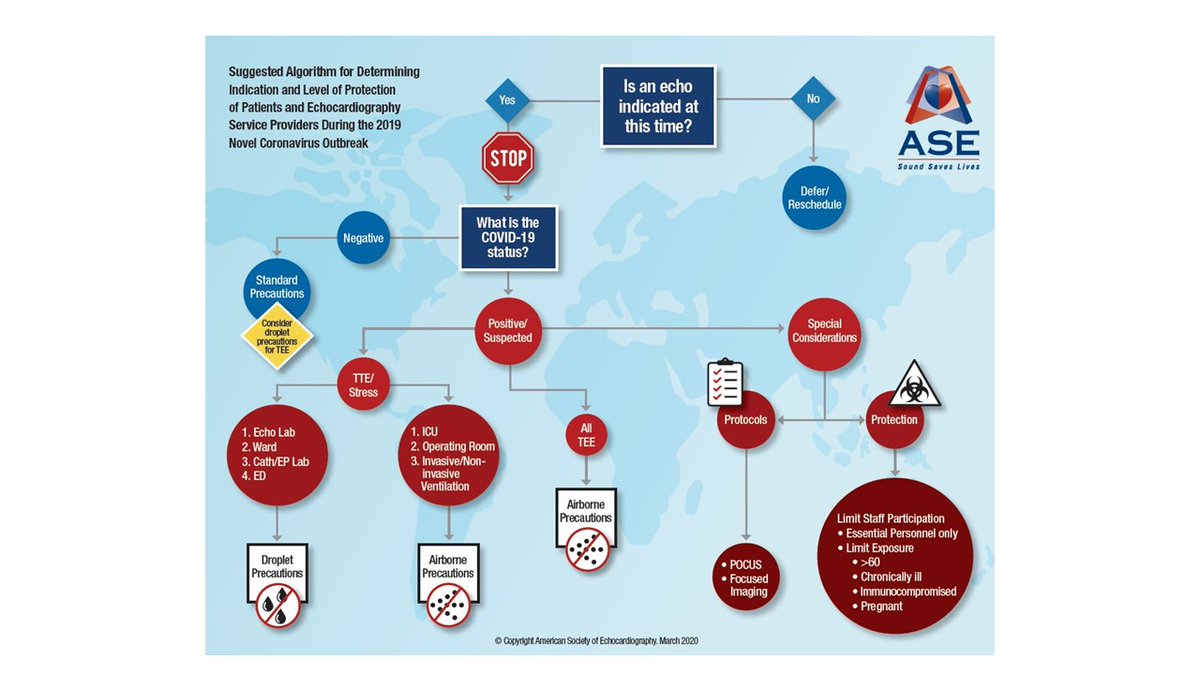
@ASE360 #COVID19 statement considers TEE as an aerosol generating procedure and provide guidance on how to perform it in PUIs or confirmed cases. https://www.asecho.org/wp-content/uploads/2020/04/COPE_COVID_Supplement_FINAL.pdf">https://www.asecho.org/wp-conten...
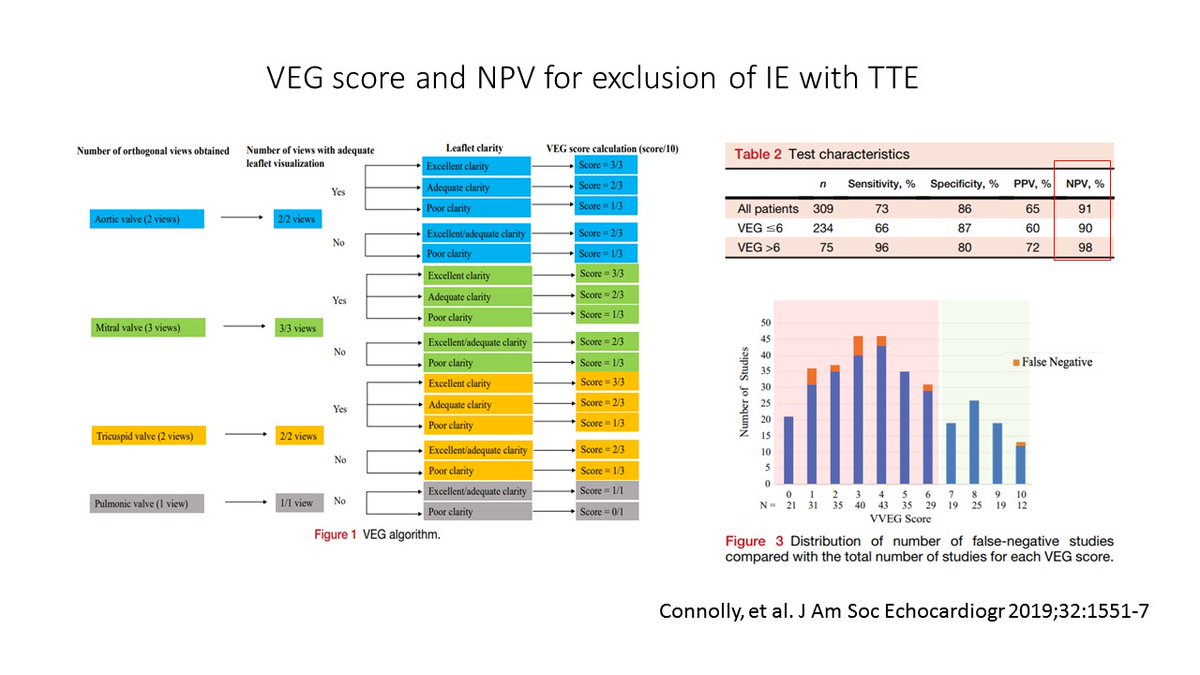
However there are some alternatives that are very good and can be employed in a patient with suspected endocarditis.A very good quality TTE that is negative for vegetations can exclude endocarditis really well. Include in your report some statement about technical quality for IE.
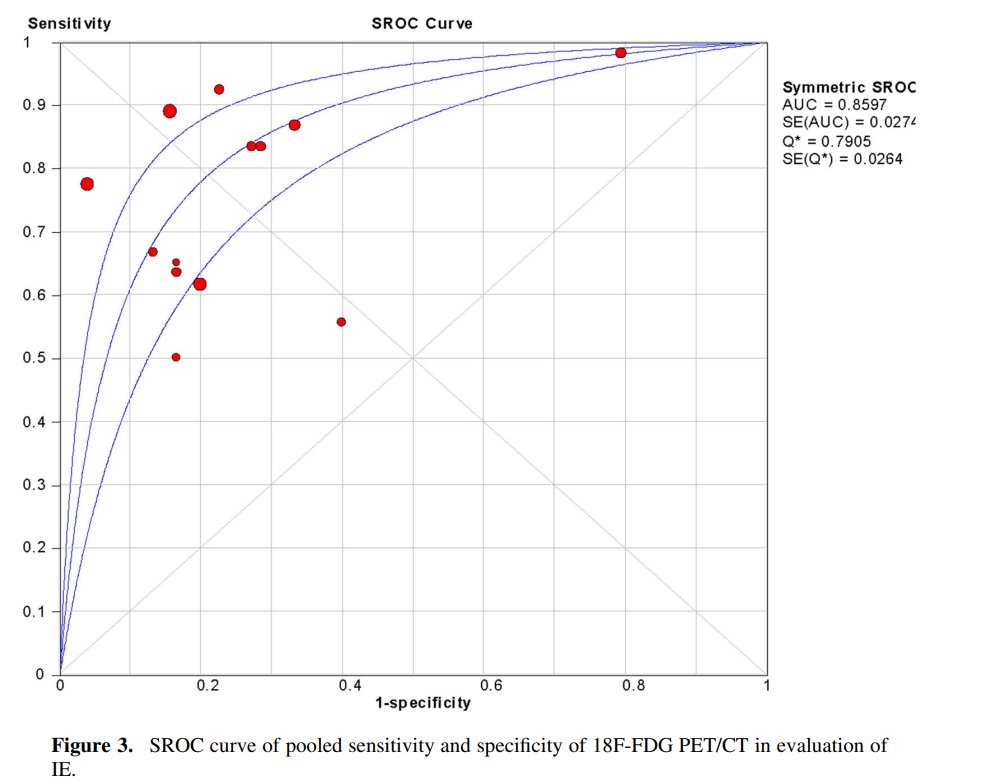
A very good option is the use of FDG-PET, but there& #39;s a caveat. Not as sensitive in native IE, but performs well to r/o prosthetic valve endocarditis. A meta-analysis of the dx performance of FDG-PET in IE found sens 78%/ spec 77% and higher sens for prosthetic valve IE of 80%
Link for metananlysis: https://pubmed.ncbi.nlm.nih.gov/29086386/ ">https://pubmed.ncbi.nlm.nih.gov/29086386/...
#YeSCCT and #WhyCMR can help to identify complications such as paravalvular abscesses and #YeSCCT probably better if prosthetic valve is present. Limitations in identifying vegetations are encountered in both modalities.
Make sure you go carefully through the modified Duke& #39;s Criteria for endocarditis and assess the indication of the TEE. Stringency should be determined depending on how far from the COVID peak your state/province is. Good communication with ID important. Wear full PPE for TEE.

 Read on Twitter
Read on Twitter