1/20 Tweetorial about Lung Protective Ventilation and Driving Pressure motivated by the complex vent management in #Covid-19. Enjoy!
Note- all in Volume Control
@cardionerds @CPSolvers @thecurbsiders @DxRxEdu @AnnaPodolanczuk @BBroderickMD @sanjayvdesai @sanjum @DrDaleNeedham
Note- all in Volume Control
@cardionerds @CPSolvers @thecurbsiders @DxRxEdu @AnnaPodolanczuk @BBroderickMD @sanjayvdesai @sanjum @DrDaleNeedham
2/Covid causes ARDS. The cornerstone of ARDS management is lung protective ventilation → reduce mechanical stress on the lung → minimize ventilator-induced lung injury. The landmark ARMA trial showed lower tidal volume ventilation helps in this effort https://www.nejm.org/doi/full/10.1056/NEJM200005043421801">https://www.nejm.org/doi/full/...
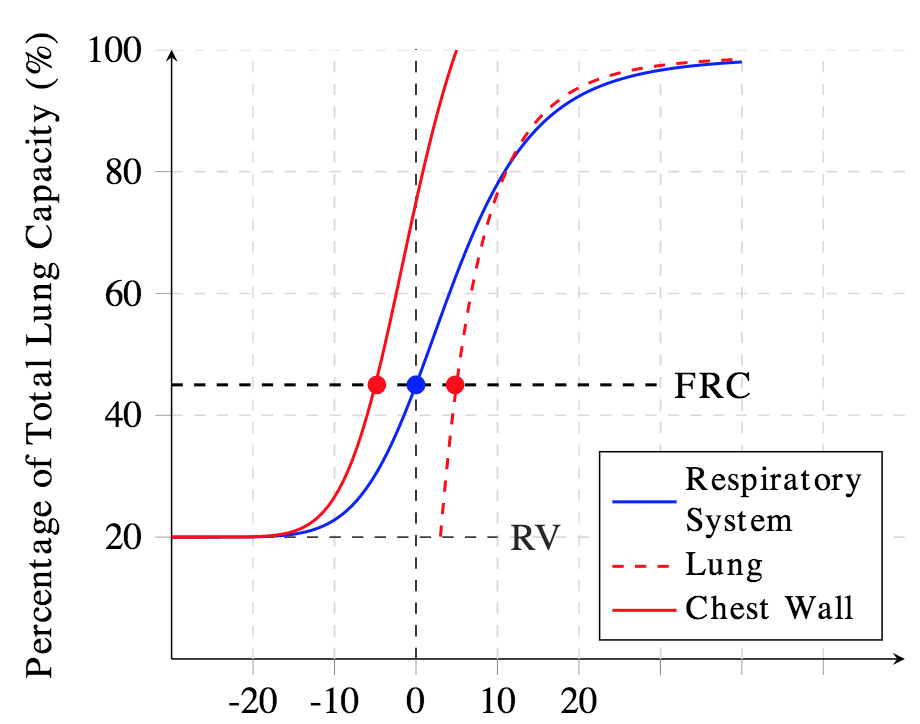
3/ In ARDS, there is reduced lung and respiratory system compliance. Respiratory system compliance (Crs) is made up of lung compliance and chest wall compliance, and while considering these two components separately is extremely important, for now, let& #39;s just focus on Crs
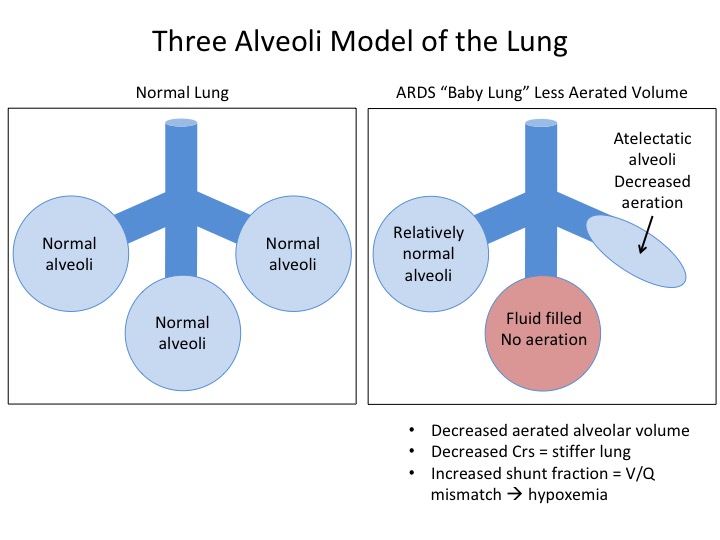
4/ Crs is reduced in ARDS, and while there may be some increased stiffness (a tire is harder to inflate than a latex balloon), mostly this is driven by a decreased functional lung size (a small rubber band is harder to stretch than a large rubber band)
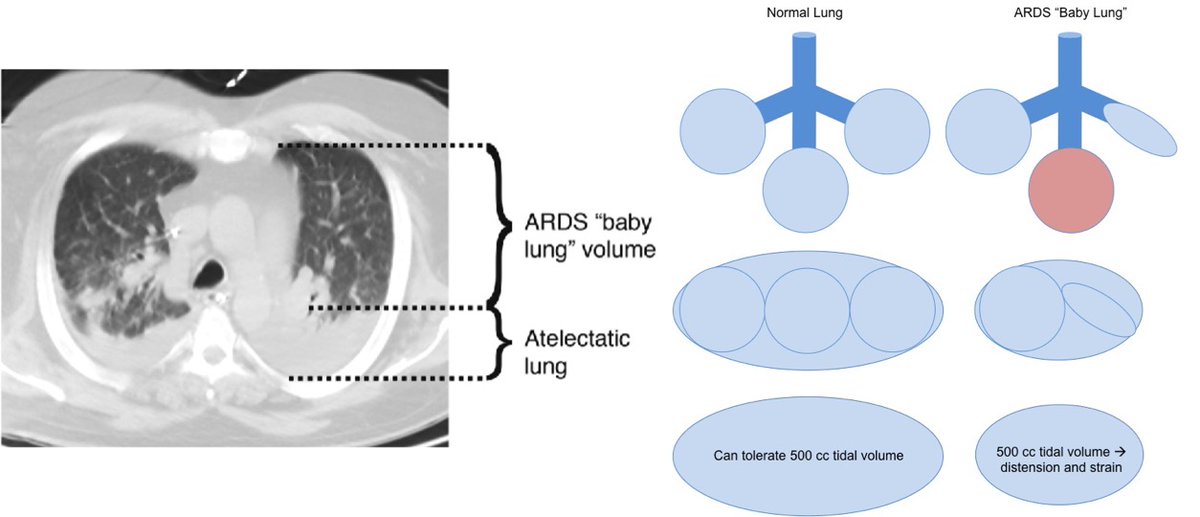
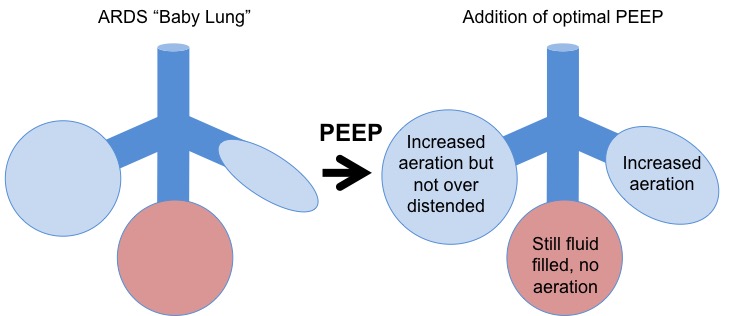
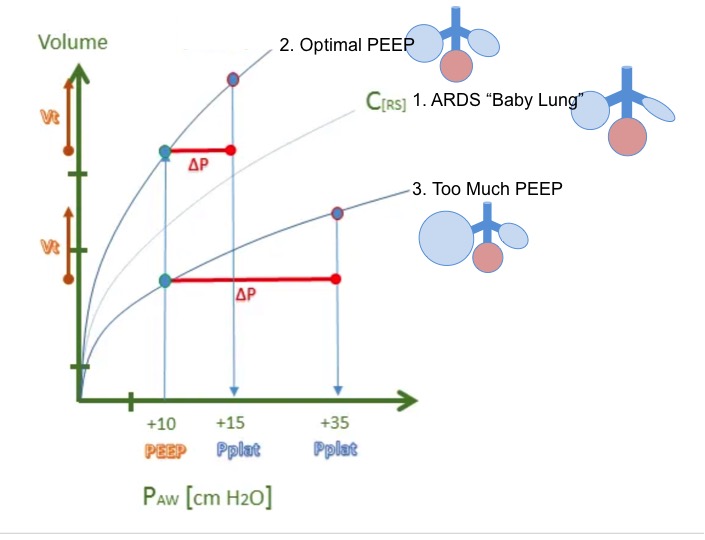
5/ In ARDS, the functional size of the lung is reduced because some of the alveoli are collapsed or filled with non-cardiogenic pulmonary edema. This is called the “baby lung” model. Since there are fewer well-aerated alveoli, the lung is overall stiffer ≈ reduced Crs.
6/ If you deliver the same volume to the “baby lung” as a normal lung → high distending pressures and strain → ventilator-induced lung injury. This is why low Vt ventilation is lung protective. One measure of this is plateau pressure, and we think levels > 30 are harmful.
7/ Determining the exact volume of the “baby lung” is difficult, so as small Vt as possible are preferred to avoid over-distention. Decrease Vt so plateau pressure is < 30. To do this, tolerate less alveolar ventilation and permissive hypercapnia as long as the pH is >7.15 – 7.2
8/ With PEEP, we add another element. Using PEEP we can recruit more aerated alveoli. This leads to more surface area for gas exchange and improved oxygenation AND increased functional lung size. The increased size of the “baby lung” can increase Crs and decrease lung stiffness
9/ However, if you use too much PEEP, you get diminishing returns. You don’t recruit more alveoli, and instead over-distend them. This doesn’t improve oxygenation, causes harmful stretch of the lung, and can increase the risk of barotrauma and pneumothoraces.
10/ Wow! There is a lot to keep straight. To review – you want to use lung protective tidal volumes, but predicting the volume of the “baby lung” is difficult so the smaller the better. PEEP is helpful to recruit aerated lung, but too much can be bad. How do we optimize it all?
11/ This is where driving pressure (ΔP) comes in to play.
Respiratory system compliance (Crs) = change in volume of the lungs (ΔV) / change in pressure in the lungs (ΔP).
ΔV is tidal volume, which we are setting, so rearranging:
Driving Pressure ΔP = Vt / Crs
Respiratory system compliance (Crs) = change in volume of the lungs (ΔV) / change in pressure in the lungs (ΔP).
ΔV is tidal volume, which we are setting, so rearranging:
Driving Pressure ΔP = Vt / Crs
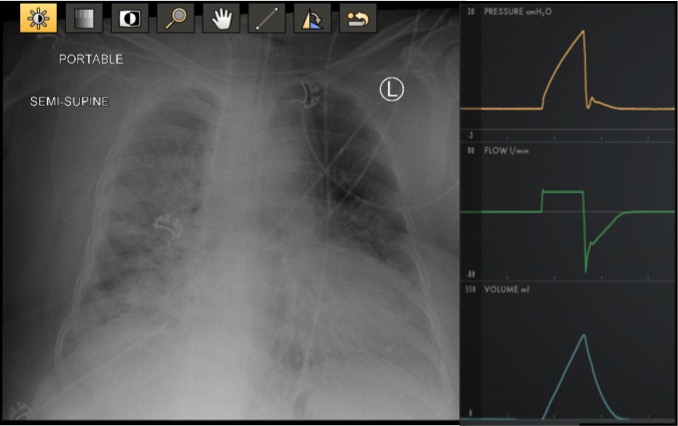
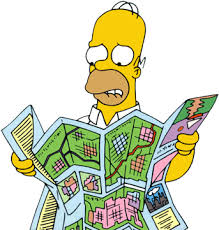
13/ Too much algebra. Thankfully, with the ventilator, we have a simpler way of measuring Driving Pressure. As long as the patient is making no effort (sedated +/- paralyzed):
Driving Pressure = Plateau pressure – PEEP.
This can be seen in the diagram below:
Driving Pressure = Plateau pressure – PEEP.
This can be seen in the diagram below:
14/ Changing PEEP changes Crs (slope of the line)
Add optimal PEEP we recruit alveoli, the compliance increases and the curve shifts up and to the left (line 1 to line 2)
Add too much PEEP, we over-distend, worsen compliance and the curve shifts down and to the right (line 3)
Add optimal PEEP we recruit alveoli, the compliance increases and the curve shifts up and to the left (line 1 to line 2)
Add too much PEEP, we over-distend, worsen compliance and the curve shifts down and to the right (line 3)
15/ As you can see, with optimal PEEP and improved compliance, the ΔP is lower for the same Vt. Conversely, with worse compliance, the same Vt causes a higher ΔP.
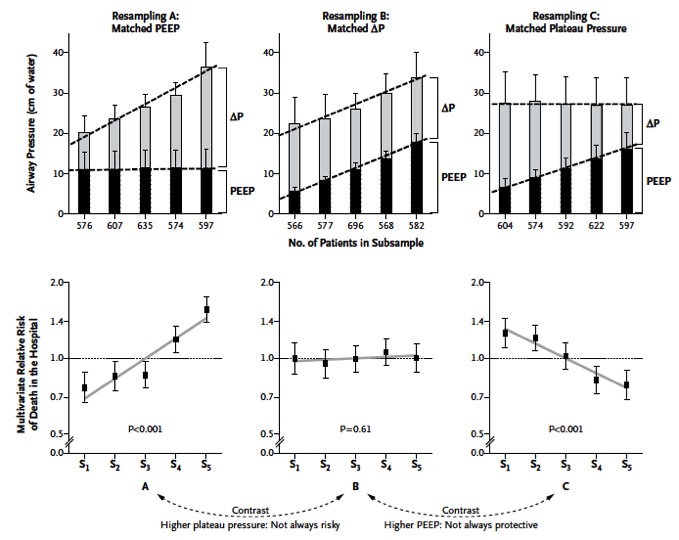
16 / That is great, but why does this matter? In NEJM in 2015 Amato et al retrospectively analyzed prior ARDS data and showed that the amount of driving pressure ΔP was most closely associated with mortality, and was a better predictor of mortality than PEEP or Plateau Pressure.
17/ ΔP is affected by Vt and PEEP, and we don’t have an RCT yet about the best way to titrate these settings to optimize ΔP. For now, it is best to be aware of it as a prognosticator and when titrating PEEP.
A ΔP > 12-15 is associated with increased mortality.
A ΔP > 12-15 is associated with increased mortality.
18/ If you increase the PEEP a certain amount (x), and the ΔP increases by more than (x), you should be wary that you may be over-distending.
If the ΔP goes up by less than (x), you& #39;re probably recruiting alveoli!
Try to find the optimal level of recruitment with plat <30.
If the ΔP goes up by less than (x), you& #39;re probably recruiting alveoli!
Try to find the optimal level of recruitment with plat <30.
19/ In sum, lung protective ARDS management includes:
-Low tidal volume ventilation. Remember the “baby lung”
-Reduce Vt with permissive hypercapnia (pH>7.15-7.2)
-Target plateau pressure < 30
-Increase PEEP for recruitment of alveoli to optimize Crs
-As titrate PEEP measure ΔP
-Low tidal volume ventilation. Remember the “baby lung”
-Reduce Vt with permissive hypercapnia (pH>7.15-7.2)
-Target plateau pressure < 30
-Increase PEEP for recruitment of alveoli to optimize Crs
-As titrate PEEP measure ΔP
20/ Thanks for reading!! Here are some websites and resources I used for this tweetorial.
http://Pulmccm.org"> http://Pulmccm.org for amazing images
https://tinyurl.com/ydgtty6v
https://tinyurl.com/ydgtty6v&... href=" https://tinyurl.com/yaff226b
https://tinyurl.com/yaff226b&... href=" https://tinyurl.com/y7tmgaqf
https://tinyurl.com/y7tmgaqf&... href=" https://tinyurl.com/yadq8xlf
https://tinyurl.com/yadq8xlf&... href=" https://tinyurl.com/tlabd55 ">https://tinyurl.com/tlabd55&q... https://tinyurl.com/y85zjtex ">https://tinyurl.com/y85zjtex&...
http://Pulmccm.org"> http://Pulmccm.org for amazing images
https://tinyurl.com/ydgtty6v

 Read on Twitter
Read on Twitter