A case in the age of #COVID19
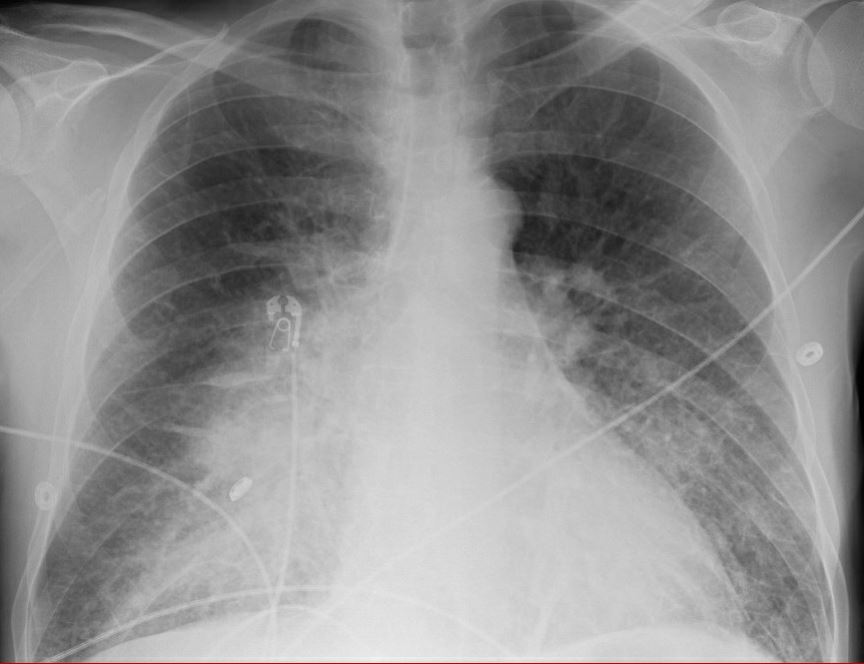
A 50 yo man with no PMH came to ED with confusion & hypoxemia. Admission CXR shown. Possible COVID+ contact.
A Protecting
B RR 28 SpO2 92% 60% HFNC
C BP 90/65 HR 105, Cap Ref 4 s
D A&0 x 4
E - T 37.9
L CRP 3x ULN, WBC 21 (PMNs)
#Tweetorial
A 50 yo man with no PMH came to ED with confusion & hypoxemia. Admission CXR shown. Possible COVID+ contact.
A Protecting
B RR 28 SpO2 92% 60% HFNC
C BP 90/65 HR 105, Cap Ref 4 s
D A&0 x 4
E - T 37.9
L CRP 3x ULN, WBC 21 (PMNs)
#Tweetorial
On arrival to the ICU he develops shock requiring vasopressors. Abx staretd. Mottling on knees. What& #39;s the next step?
Case details to follow tomorrow!
Case details to follow tomorrow!
ABG in ED 7.38 / 34 / 70 / 21 on 5L NC in ED, I did not repeat on HFNC.
IL-6 level 120 (normal: <6)
https://twitter.com/doormusings/status/1252429495945973768?s=21">https://twitter.com/doormusin... https://twitter.com/doormusings/status/1252429495945973768">https://twitter.com/doormusin...
IL-6 level 120 (normal: <6)
https://twitter.com/doormusings/status/1252429495945973768?s=21">https://twitter.com/doormusin... https://twitter.com/doormusings/status/1252429495945973768">https://twitter.com/doormusin...
Let& #39;s resume the case. #POCUS won the poll handily.
Starting with everybody& #39;s favorite, the IVC view.
Starting with everybody& #39;s favorite, the IVC view.
What should we do now??
Here& #39;s a PLAX for you. Best axis we could get on all following pictures.
What is the most important finding on this clip?
Let& #39;s interrogate that MV a bit more... thoughts?
Throwing some color... best refinement of the signal we could get
What should we do now??
This is a case of ACUTE mitral regurgitation causing cardiogenic shock.
Patient was transferred from the community to a referral center for emergent valve replacement.
Etiology unclear, non-ischemic, did not appear infectious. Multiple ruptured leaflets of P2 intra-op.
Patient was transferred from the community to a referral center for emergent valve replacement.
Etiology unclear, non-ischemic, did not appear infectious. Multiple ruptured leaflets of P2 intra-op.
Summary/Takeaways:
- Every case of shock should get a focused echo
- Each echo needs to include visual and color interrogation of valves!
- There are other causes of infiltrates than #COVID19
- Emergent valve disorders from LITFL: https://litfl.com/emergent-valve-disorders/">https://litfl.com/emergent-...
- Every case of shock should get a focused echo
- Each echo needs to include visual and color interrogation of valves!
- There are other causes of infiltrates than #COVID19
- Emergent valve disorders from LITFL: https://litfl.com/emergent-valve-disorders/">https://litfl.com/emergent-...
Oh! and one more thing: a collapsible IVC does NOT mean "needs fluids".
This patient had vigorous resp effort, the IVC essentially not interpretable even for RAP.
Fluids would have certainly caused morbidity and potentially mortality here.
This patient had vigorous resp effort, the IVC essentially not interpretable even for RAP.
Fluids would have certainly caused morbidity and potentially mortality here.

 Read on Twitter
Read on Twitter