#COVID19 Early vs delayed intubation. IMV has many known adverse effects and complications. Why would anyone want to intubate early? Two proposed reasons: 1) Prolonged hypoxemia might be harmful 2) Severely increased work of breathing might actually increase lung damage. (1)
In the words of Dr Martin J. Tobin: Evidence of end-organ damage is difficult to demonstrate in patients with PaO2 above 40 mmHg (equivalent to oxygen saturation of approximately 75%). https://doi.org/10.1164/rccm.202004-1076ED">https://doi.org/10.1164/r... (3)
Profound hypoxemia by itself should NOT cause significant physiological stress (think of congenital heart disease patients). Certainly there can be profoundly hypoxemic patients who feel just fine. (*palliative pt) https://twitter.com/cameronks/status/1243582723945566208?s=20">https://twitter.com/cameronks... (4)
Keeping this in mind PLUS the fact of ventilator shortage, many people have thought about the concept of #PermissiveHypoxemia https://twitter.com/medevidenceblog/status/1244829300861177856?s=20">https://twitter.com/medeviden... https://twitter.com/MercadalJordi/status/1245985815769092097?s=20">https://twitter.com/MercadalJ... https://twitter.com/adamdavidthomas/status/1245474476088627203?s=20">https://twitter.com/adamdavid... https://twitter.com/PaulBerglMD/status/1247289285637746688?s=20">https://twitter.com/PaulBergl... https://twitter.com/pedrodammert/status/1249171614060744706?s=20">https://twitter.com/pedrodamm... (5)
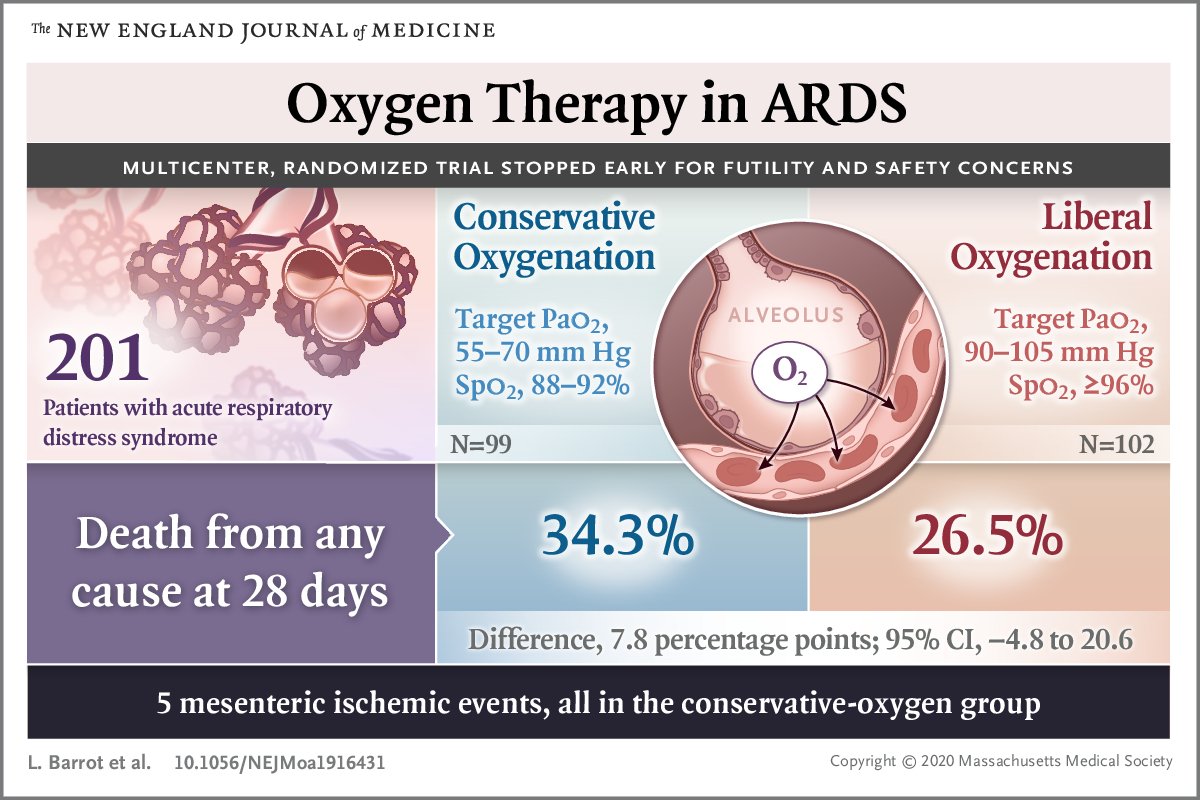
However, this is not to say that we should have lower O2sat% goals for all patients. Published evidence suggests that lower O2 goals could induce harm: e.g. 5 events of mesenteric ischemia, bearing in mind these were patients on vasopressors (70%) and average age was 63 (6)
Efforts to increase oxygenation should be taken. However if despite all efforts, refractory hypoxemia ensues, an individualized approach should be taken to identify patients who can benefit from #PermissiveHypoxemia (young, w good or increased CO, no vasopressors, no PAD) (7)
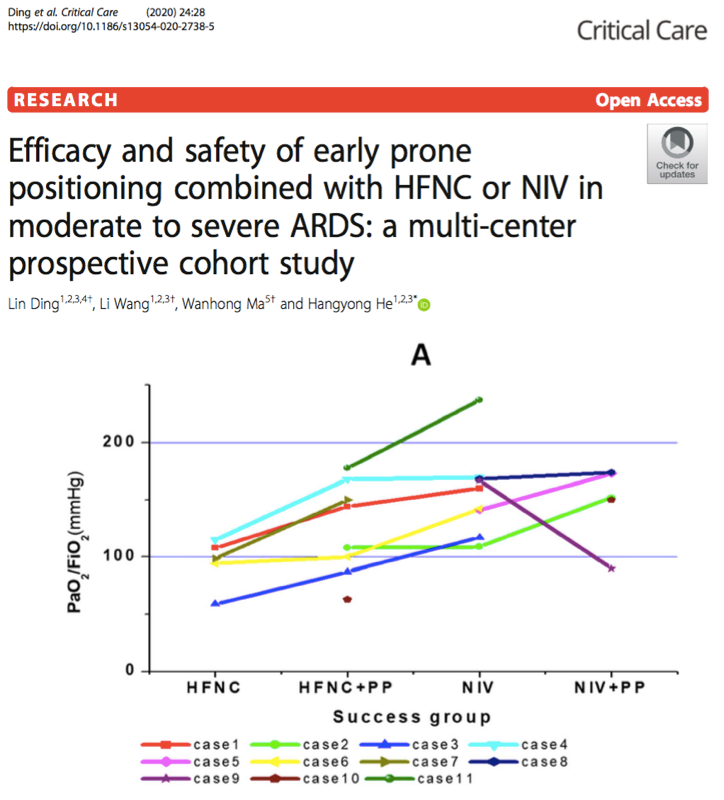
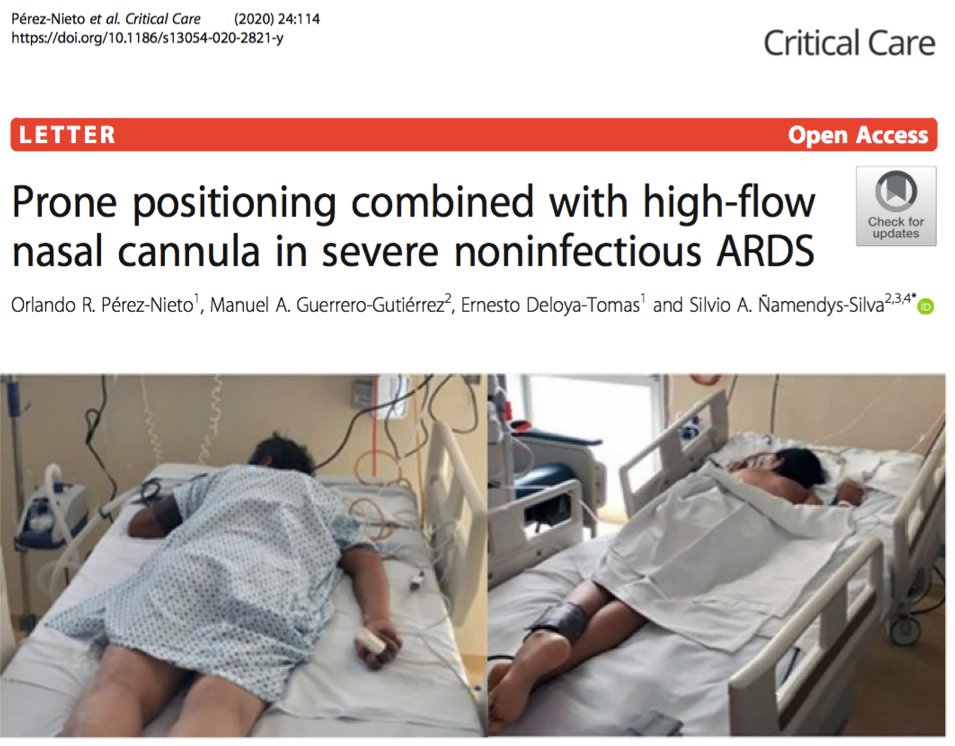
Oxigenation efforts include HFNC (might increase aerosol risk), and awake proning. Awake proning is a promising strategy to avoid intubation. We have been doing this with NRB mask with some success (foto by our ED Head @doctorthierry). Case series by Ding and @OrlandoRPN (8)
Great and very illustrative case of "Happy Hypoxemia" by @PulmCrit https://twitter.com/PulmCrit/status/1250527251709546496?s=20">https://twitter.com/PulmCrit/... (9)
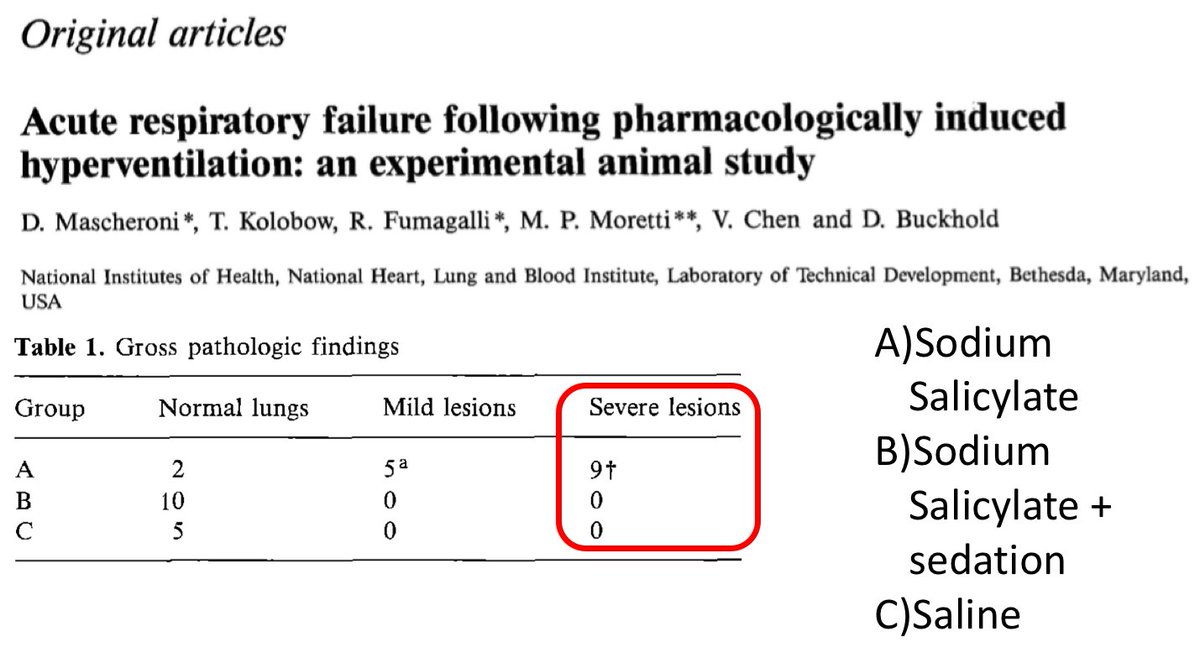
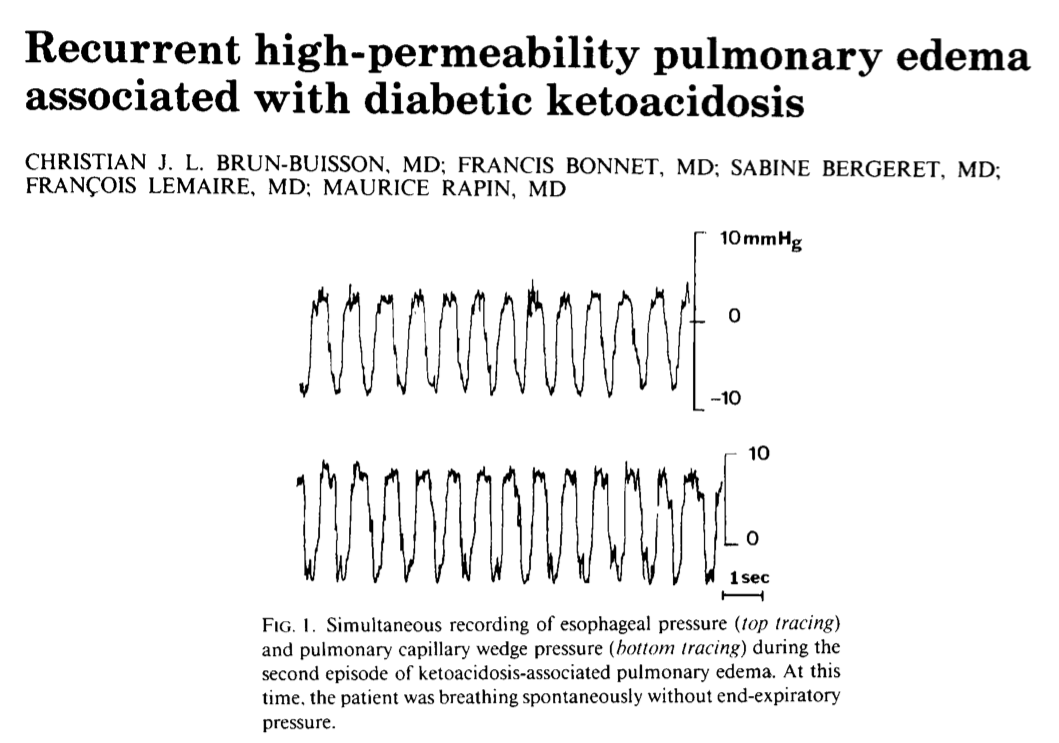
Evidence of P-SILI is weak but plausible. In sheep, infusion of sodium salycilate to the brain causes lung injury and this can be prevented by sedation. There are case reports of patients with DKA developing non cardiogenic pulmonary edema presumably from heavy breathing (11)
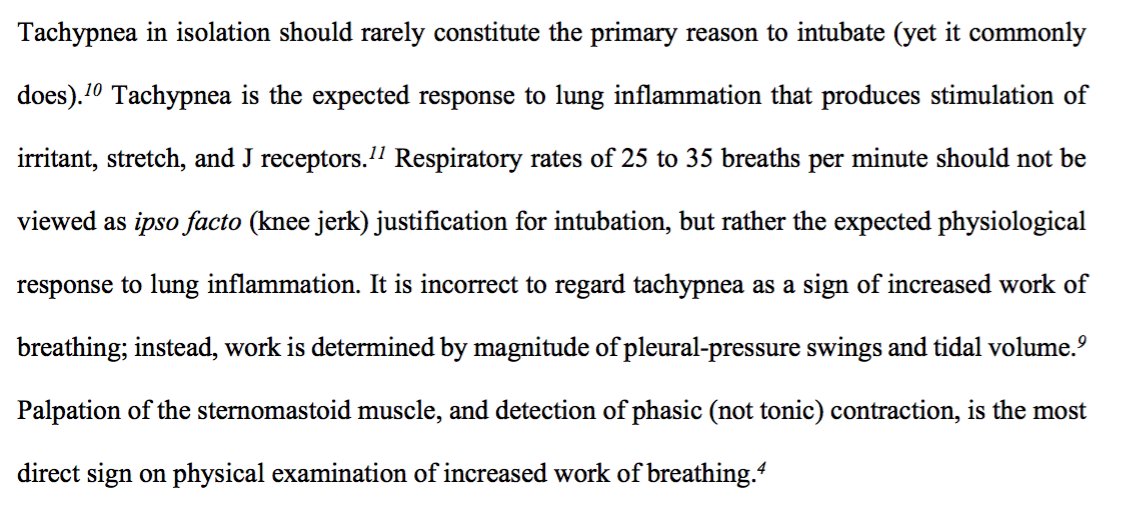
According to this, P-SILI develops when there is a high transpulmonary pressure through high pleural swings (increased EFFORT). Tachypnea by itself is not expected to cause this unless accompanied by heavy work of breathing. Again from Dr Tobin https://doi.org/10.1164/rccm.202004-1076ED">https://doi.org/10.1164/r... (12)
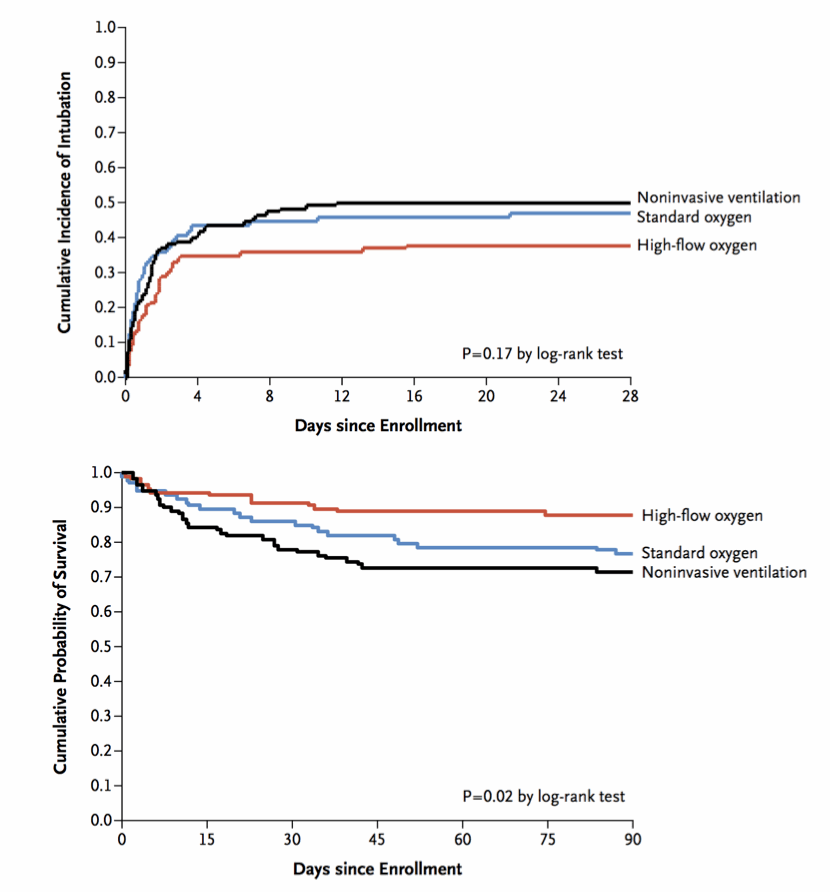
The FLORALI trial might add some indirect evidence of this. BIPAP provides pressure support so; If pt has a high respiratory drive, BIPAP could actually worsen P-SILI. CPAP is not expected to do this. HFNC by reducing dead space can reduce WOB. 10.1056/NEJMoa1503326 (13)
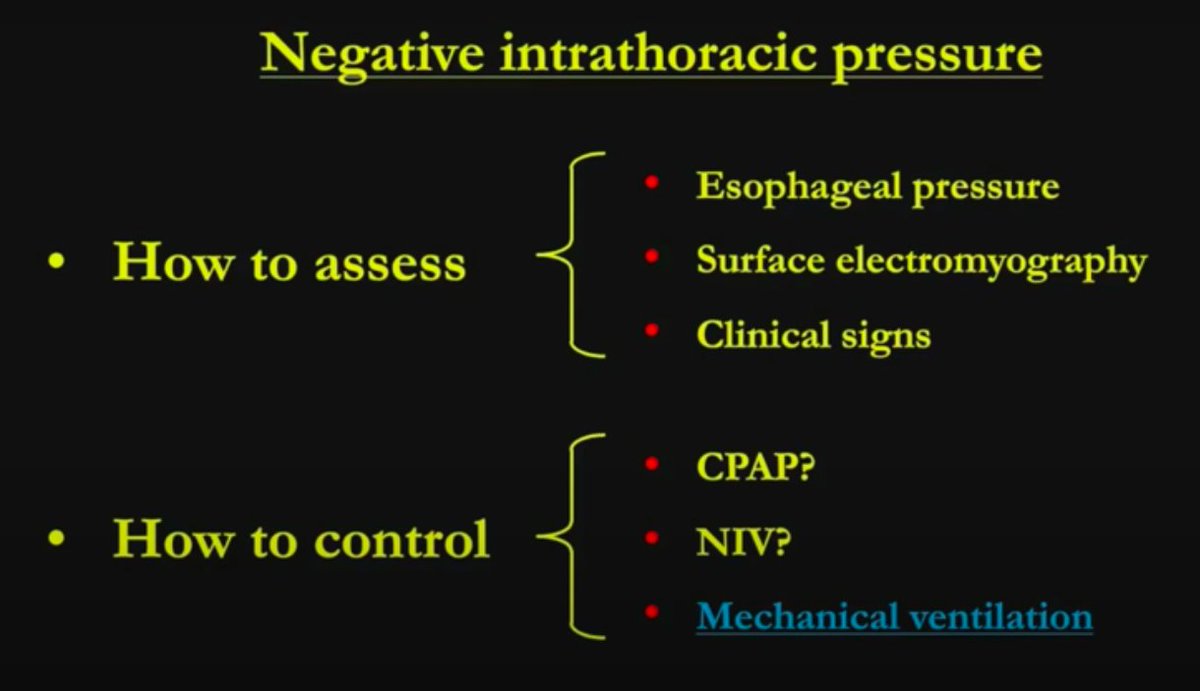
How then to evaluate increased respiratory effort? @gattinon acknowledges that while esophageal catheter is helpful, this is not a tool that should be used during a pandemic. In his webinar, he mentions that clinical assessment is key (14)
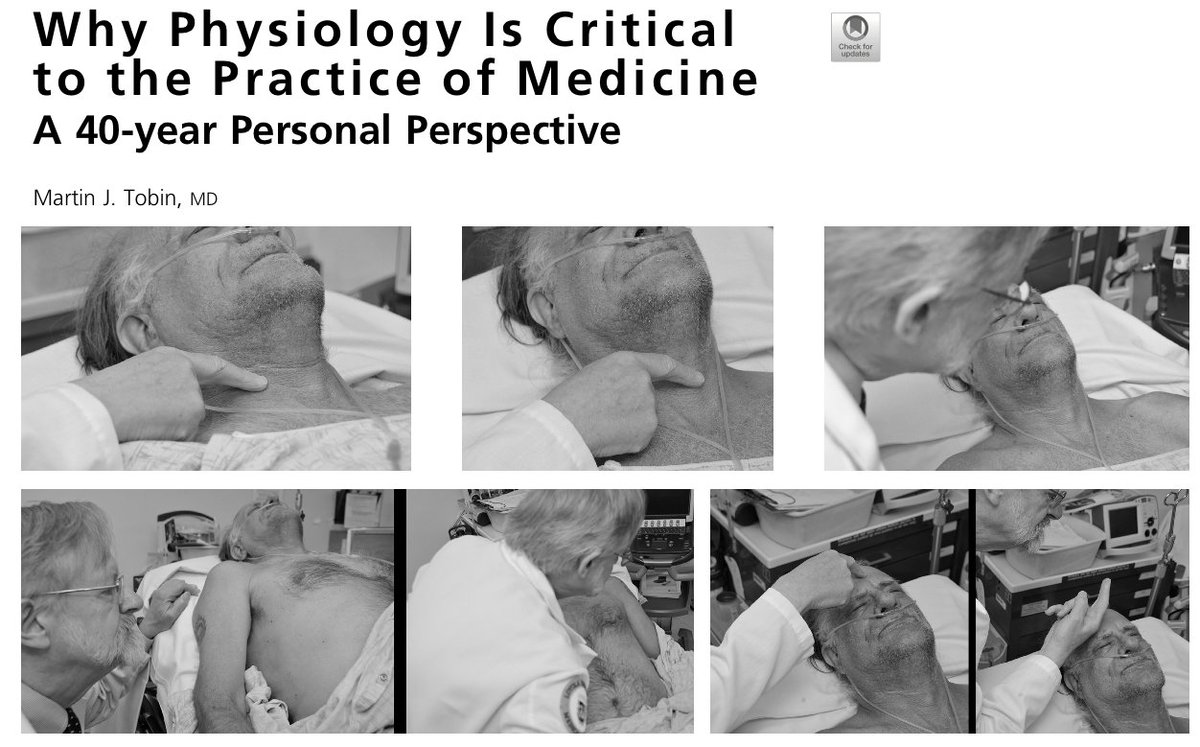
How to clinically asses effort? Again, Dr Tobin comes to the rescue with one of the best written articles I& #39;ve read in clinical medicine. Palpation of sternomastoid and traquea, inspection of suprasternal fossa, intercostals, and Hoover sign https://doi.org/10.1016/j.ccm.2019.02.012">https://doi.org/10.1016/j... (15)
So, its not straight forward. Intubation should not be guided by any single parameter. Certainly not only for hypoxemia or tachypnea. In some patients, this can be tolerated #zentensivist. WOB assessment is extremely important and if increased should point the need for intubation
ping some #zentensivist twitter friends: @msiuba @Thind888 @PulmCrit @pulmcritter @medevidenceblog @Acute_Pulmo_Med @iceman_ex @ResusTonight @some4mv

 Read on Twitter
Read on Twitter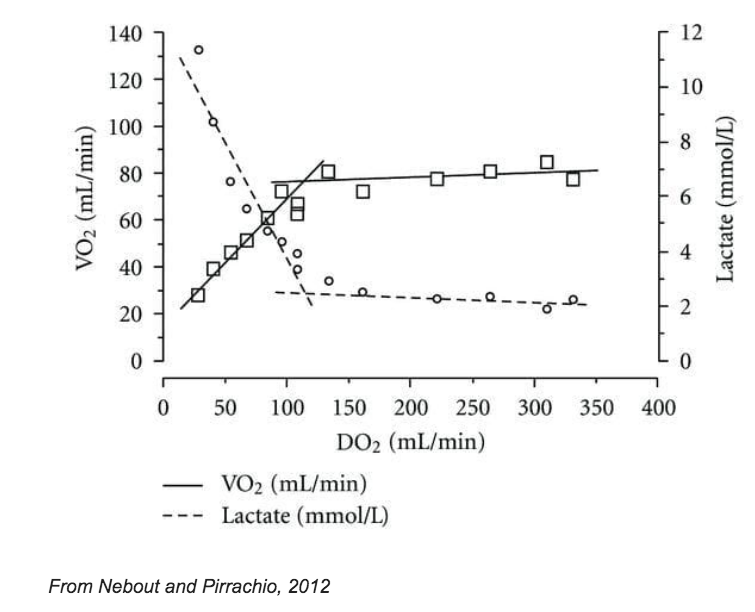 Should we tolerate hypoxemia? Physiology 1st: If nothing else changes, even a 40% sat would still mean a DO2 of about 2x VO2 (normally 5x greater). Increased CO can improve this a lot. A young, previously healthy and hemodynamically stable pt should tolerate 80% just fine (2)" title="https://abs.twimg.com/emoji/v2/... draggable="false" alt="1⃣" title="Keycap digit one" aria-label="Emoji: Keycap digit one">Should we tolerate hypoxemia? Physiology 1st: If nothing else changes, even a 40% sat would still mean a DO2 of about 2x VO2 (normally 5x greater). Increased CO can improve this a lot. A young, previously healthy and hemodynamically stable pt should tolerate 80% just fine (2)" class="img-responsive" style="max-width:100%;"/>
Should we tolerate hypoxemia? Physiology 1st: If nothing else changes, even a 40% sat would still mean a DO2 of about 2x VO2 (normally 5x greater). Increased CO can improve this a lot. A young, previously healthy and hemodynamically stable pt should tolerate 80% just fine (2)" title="https://abs.twimg.com/emoji/v2/... draggable="false" alt="1⃣" title="Keycap digit one" aria-label="Emoji: Keycap digit one">Should we tolerate hypoxemia? Physiology 1st: If nothing else changes, even a 40% sat would still mean a DO2 of about 2x VO2 (normally 5x greater). Increased CO can improve this a lot. A young, previously healthy and hemodynamically stable pt should tolerate 80% just fine (2)" class="img-responsive" style="max-width:100%;"/>

 What about Patient Self Induced Lung Injury? Some believe non intubated patients with prolonged heavy work of breathing can cause themselves lung injury through big changes in transpulmonary pressure (pleural swings). They advocate early intubation to prevent this (10)" title="https://abs.twimg.com/emoji/v2/... draggable="false" alt="2⃣" title="Keycap digit two" aria-label="Emoji: Keycap digit two">What about Patient Self Induced Lung Injury? Some believe non intubated patients with prolonged heavy work of breathing can cause themselves lung injury through big changes in transpulmonary pressure (pleural swings). They advocate early intubation to prevent this (10)">
What about Patient Self Induced Lung Injury? Some believe non intubated patients with prolonged heavy work of breathing can cause themselves lung injury through big changes in transpulmonary pressure (pleural swings). They advocate early intubation to prevent this (10)" title="https://abs.twimg.com/emoji/v2/... draggable="false" alt="2⃣" title="Keycap digit two" aria-label="Emoji: Keycap digit two">What about Patient Self Induced Lung Injury? Some believe non intubated patients with prolonged heavy work of breathing can cause themselves lung injury through big changes in transpulmonary pressure (pleural swings). They advocate early intubation to prevent this (10)">
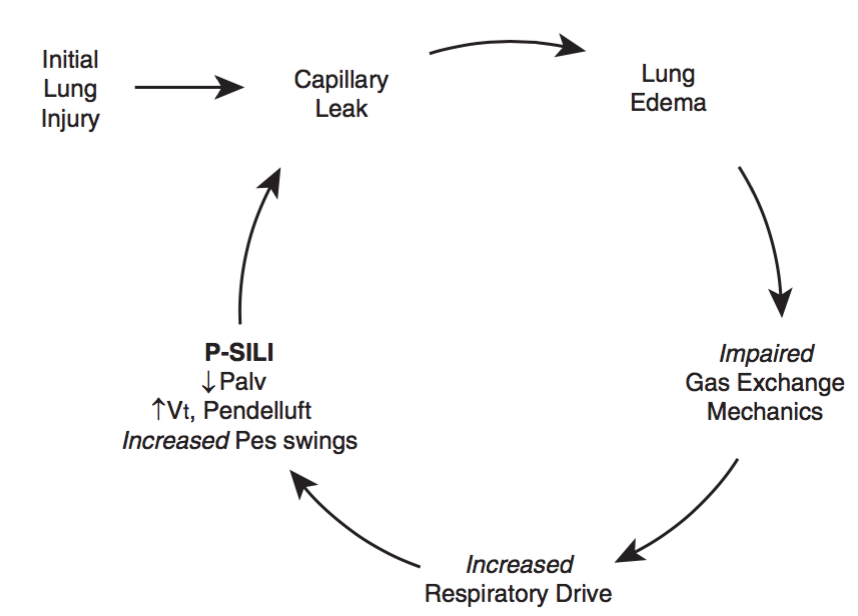 What about Patient Self Induced Lung Injury? Some believe non intubated patients with prolonged heavy work of breathing can cause themselves lung injury through big changes in transpulmonary pressure (pleural swings). They advocate early intubation to prevent this (10)" title="https://abs.twimg.com/emoji/v2/... draggable="false" alt="2⃣" title="Keycap digit two" aria-label="Emoji: Keycap digit two">What about Patient Self Induced Lung Injury? Some believe non intubated patients with prolonged heavy work of breathing can cause themselves lung injury through big changes in transpulmonary pressure (pleural swings). They advocate early intubation to prevent this (10)">
What about Patient Self Induced Lung Injury? Some believe non intubated patients with prolonged heavy work of breathing can cause themselves lung injury through big changes in transpulmonary pressure (pleural swings). They advocate early intubation to prevent this (10)" title="https://abs.twimg.com/emoji/v2/... draggable="false" alt="2⃣" title="Keycap digit two" aria-label="Emoji: Keycap digit two">What about Patient Self Induced Lung Injury? Some believe non intubated patients with prolonged heavy work of breathing can cause themselves lung injury through big changes in transpulmonary pressure (pleural swings). They advocate early intubation to prevent this (10)">