#nephmadness #EthicsRegion
1/ Kidney failure treatment: what’s the right decision?
An active, 77-year old Retiree with diabetes and ischemic cardiomyopathy has advanced kidney disease and needs to think about treatment options. Would you recommend dialysis?
1/ Kidney failure treatment: what’s the right decision?
An active, 77-year old Retiree with diabetes and ischemic cardiomyopathy has advanced kidney disease and needs to think about treatment options. Would you recommend dialysis?
2/ As well as more medical information, an intuitive impression regarding your patient’s survival can predict outcomes too: such as the response to the “surprise question: “Would I be surprised if this patient died in the next one year?”
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2518805/">https://www.ncbi.nlm.nih.gov/pmc/artic...
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2518805/">https://www.ncbi.nlm.nih.gov/pmc/artic...
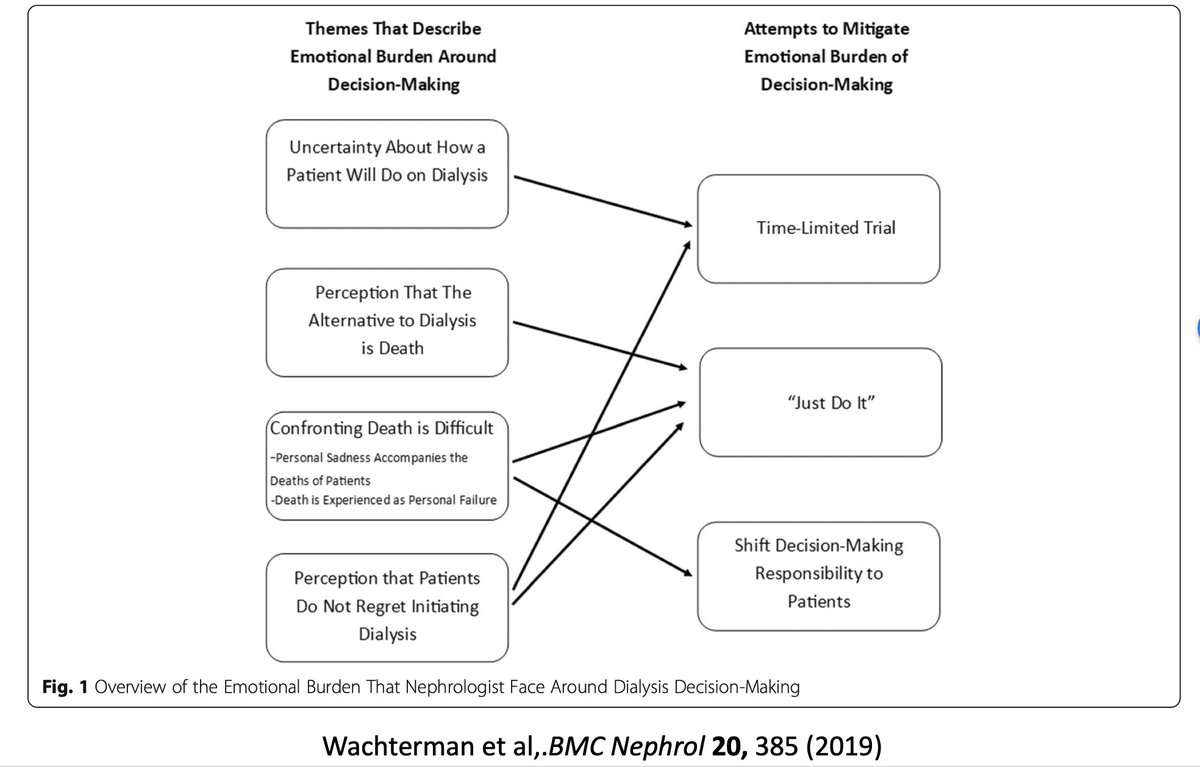
3/ It’s worth remembering that our recommendations may be influenced by our own uncertainty (regarding prognosis) and discomfort with discussing death or dying, as shown in this qualitative study:
https://bmcnephrol.biomedcentral.com/track/pdf/10.1186/s12882-019-1565-x">https://bmcnephrol.biomedcentral.com/track/pdf...
https://bmcnephrol.biomedcentral.com/track/pdf/10.1186/s12882-019-1565-x">https://bmcnephrol.biomedcentral.com/track/pdf...
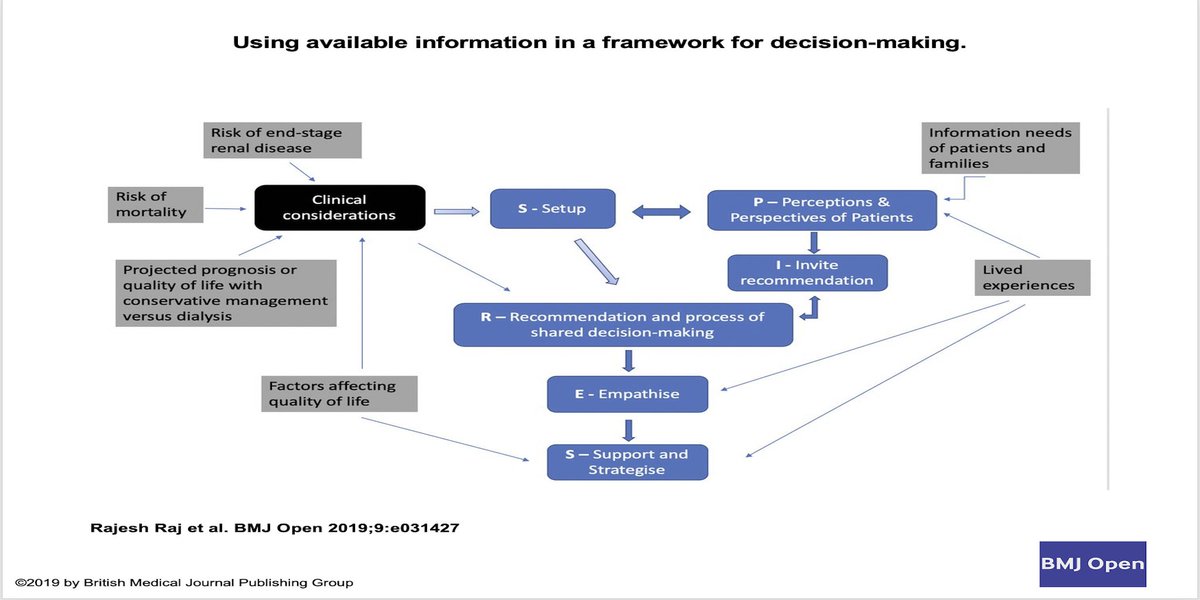
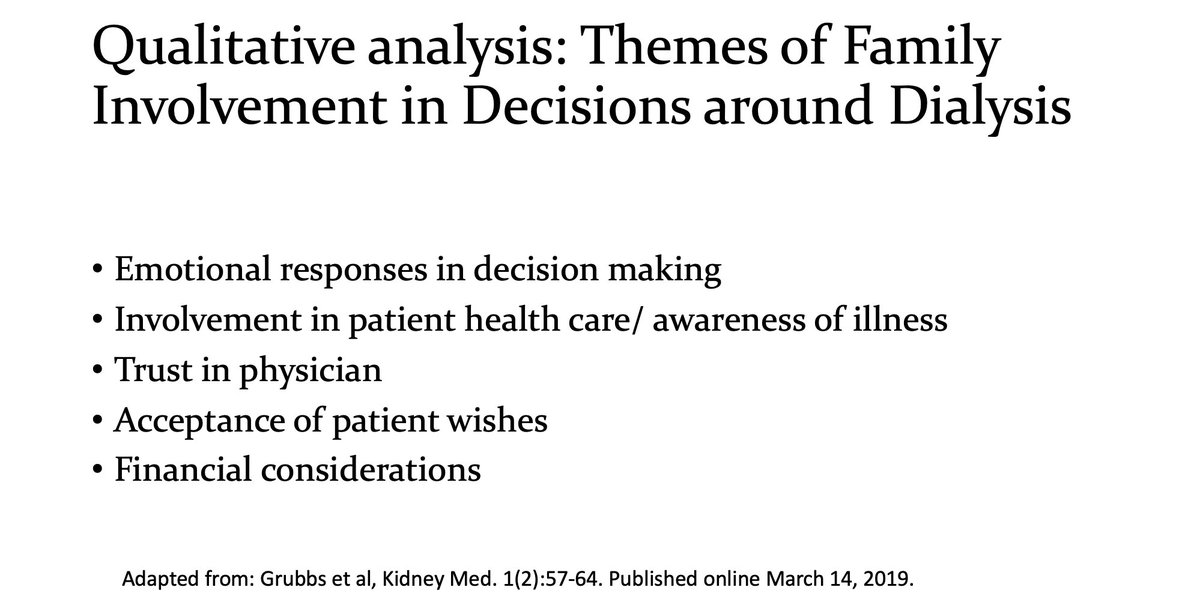
4/ Assuming we can now have a Discussion with the patient, how can we better facilitate this conversation? Shouldn& #39;t we get family involved too?
https://www.kidneymedicinejournal.org/article/S2590-0595(19)30019-6/pdf">https://www.kidneymedicinejournal.org/article/S...
https://www.kidneymedicinejournal.org/article/S2590-0595(19)30019-6/pdf">https://www.kidneymedicinejournal.org/article/S...
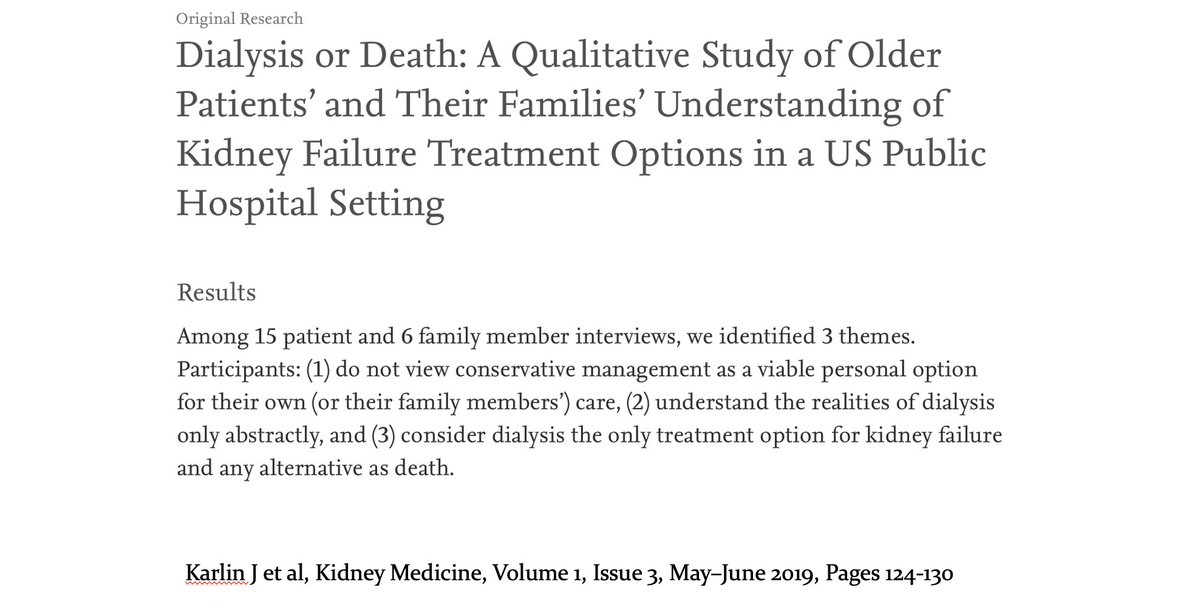
5/ Few things are as hard as choosing between dialysis or no-dialysis. Patients may think conservative care is not an option, or that there is no real choice:that it& #39;s dialysis or death!
https://www.sciencedirect.com/science/article/pii/S2590059519300330
https://www.sciencedirect.com/science/a... href=" https://www.ncbi.nlm.nih.gov/pubmed/22560169 ">https://www.ncbi.nlm.nih.gov/pubmed/22...
https://www.sciencedirect.com/science/article/pii/S2590059519300330
6/ In fact, choosing not to have dialysis and opting for renal supportive care instead might be the ideal decision for some patients - As discussed in this thread:
https://twitter.com/Kidneymedic/status/1239893164531412992">https://twitter.com/Kidneymed...
https://twitter.com/Kidneymedic/status/1239893164531412992">https://twitter.com/Kidneymed...
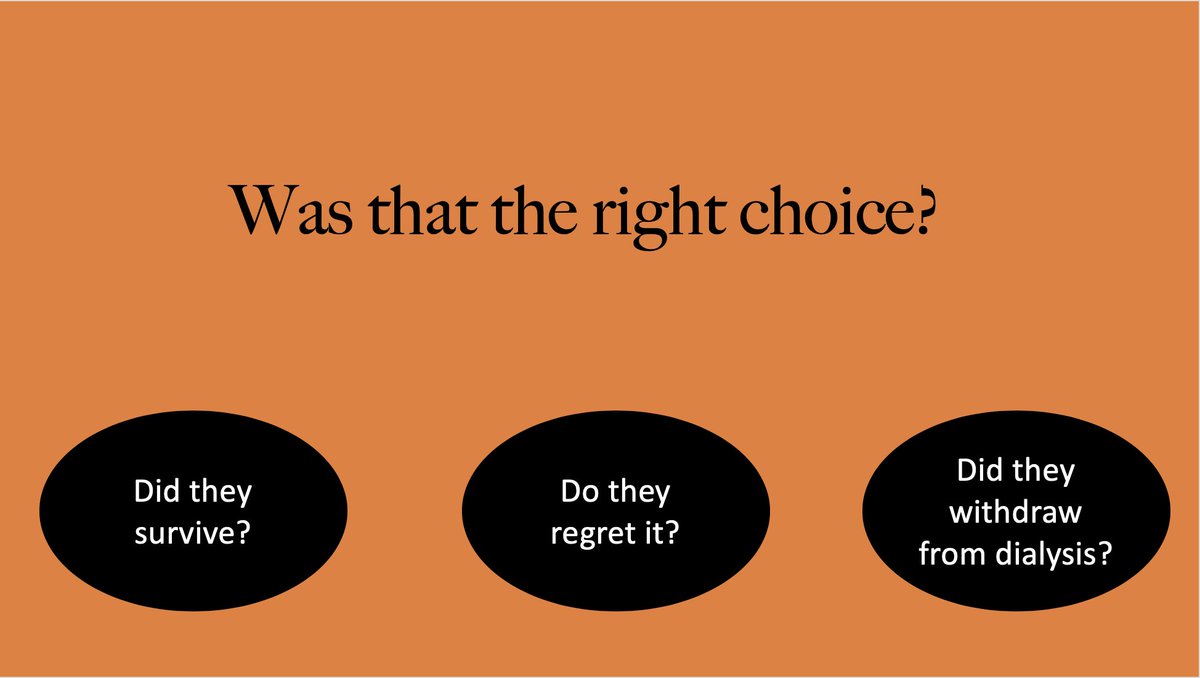
7/ How does anyone know if the choice they made was the right one? And what factors make it “the right choice?”
Survival?
Quality of life and Regret about the decision?
Dialysis withdrawal rates?
Survival?
Quality of life and Regret about the decision?
Dialysis withdrawal rates?
8/ Survival isn& #39;t an ideal yardstick - especially if this at the cost of a lower QOL. With multiple comorbidities, being on dialysis may not even alter survival!
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4317735/
https://www.ncbi.nlm.nih.gov/pmc/artic... href=" https://www.ncbi.nlm.nih.gov/pubmed/23652841 ">https://www.ncbi.nlm.nih.gov/pubmed/23...
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4317735/
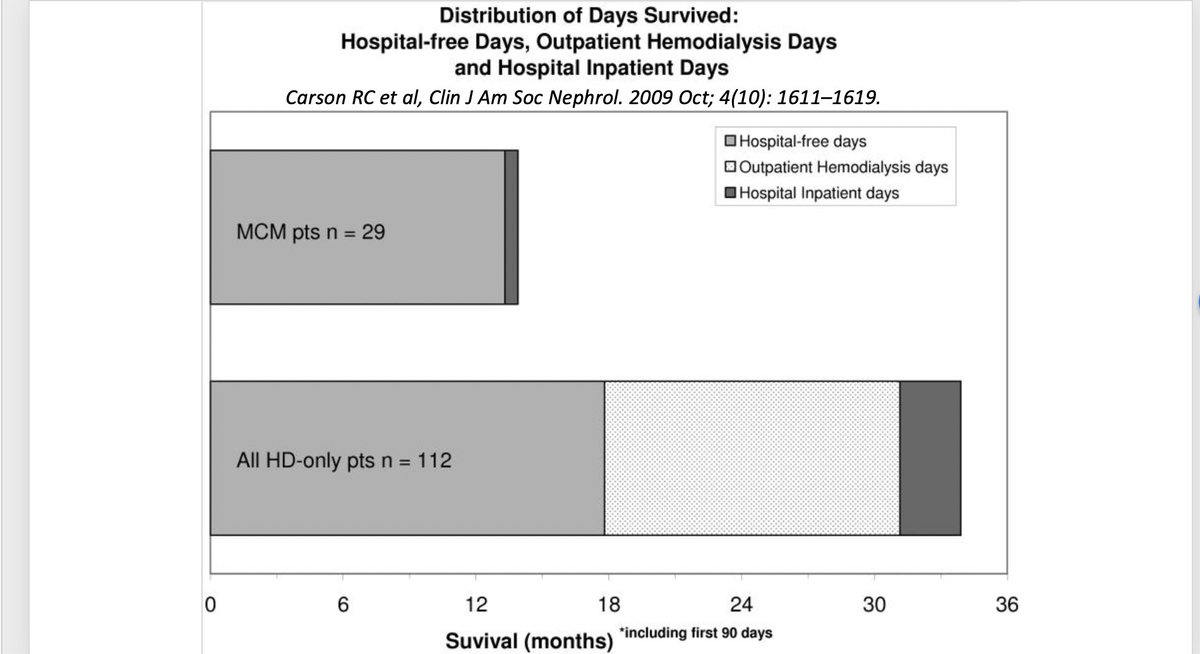
9/ In fact, even though patients may choose dialysis wanting to live longer, they may not have more time at home when they need to go to dialysis thrice a week!
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2758251/">https://www.ncbi.nlm.nih.gov/pmc/artic...
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2758251/">https://www.ncbi.nlm.nih.gov/pmc/artic...
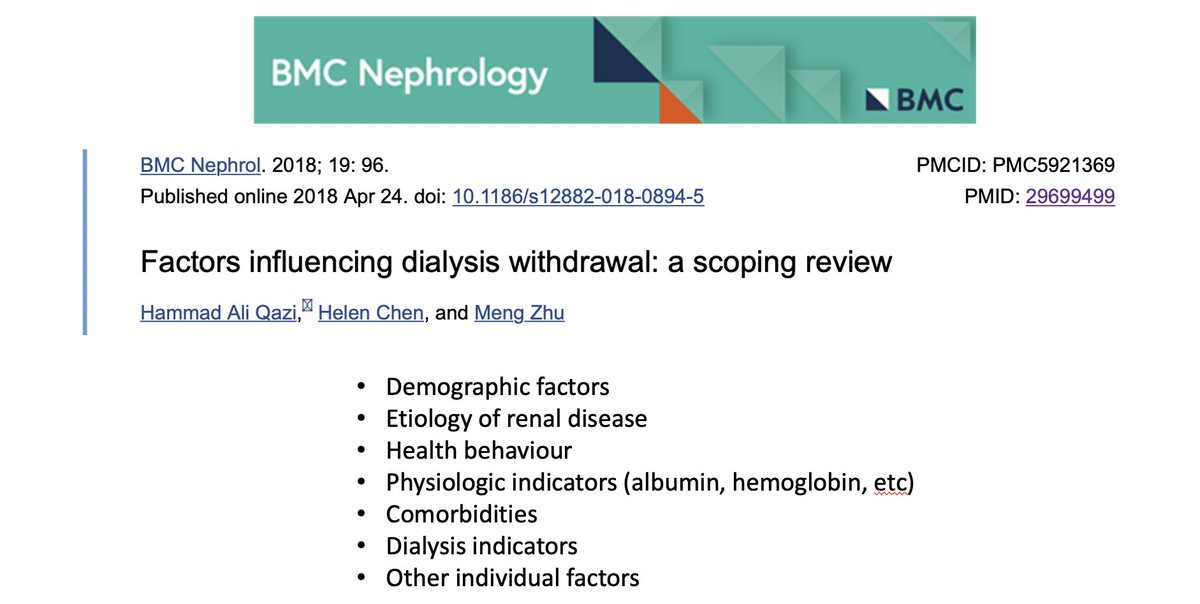
11/ Do right decisions mean no subsequent withdrawal from dialysis? Perhaps not, as several factors, some appearing late, can affect withdrawal - including increasing age, comorbidities (cancer, dementia, loss of mobility, etc)
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5921369/">https://www.ncbi.nlm.nih.gov/pmc/artic...
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5921369/">https://www.ncbi.nlm.nih.gov/pmc/artic...
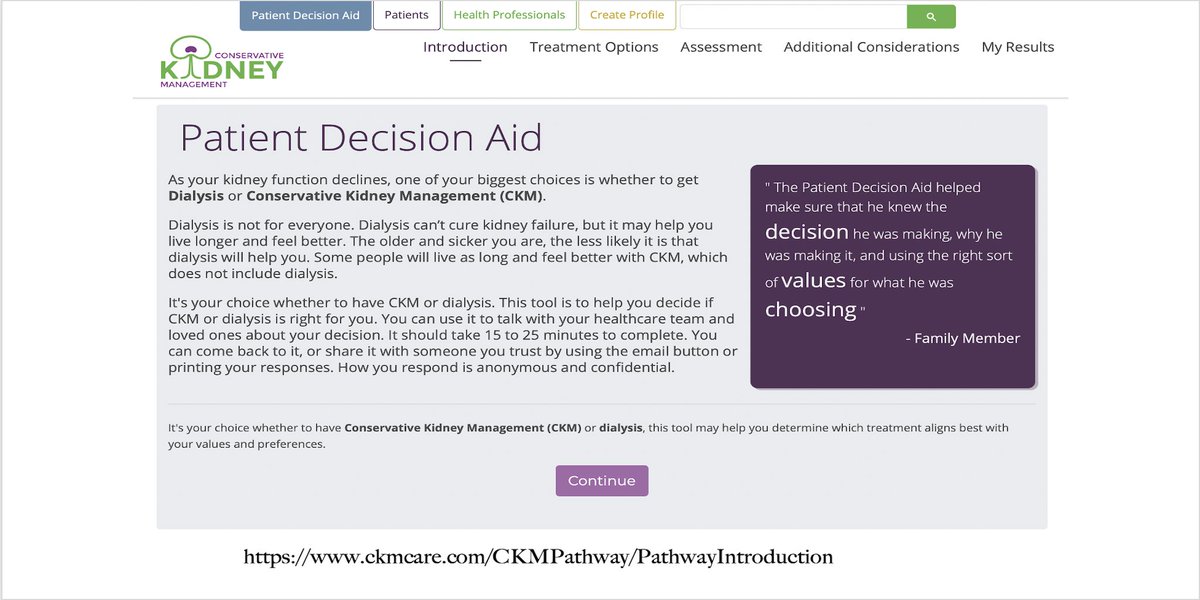
12/ To practice patient-centered medicine, though, one needs to explore what outcomes are important for patients: we must learn to ask. Patient decision aids can help them focus on these aspects: many aids are available online
https://www.ncbi.nlm.nih.gov/pubmed/28212179 ">https://www.ncbi.nlm.nih.gov/pubmed/28...
https://www.ncbi.nlm.nih.gov/pubmed/28212179 ">https://www.ncbi.nlm.nih.gov/pubmed/28...
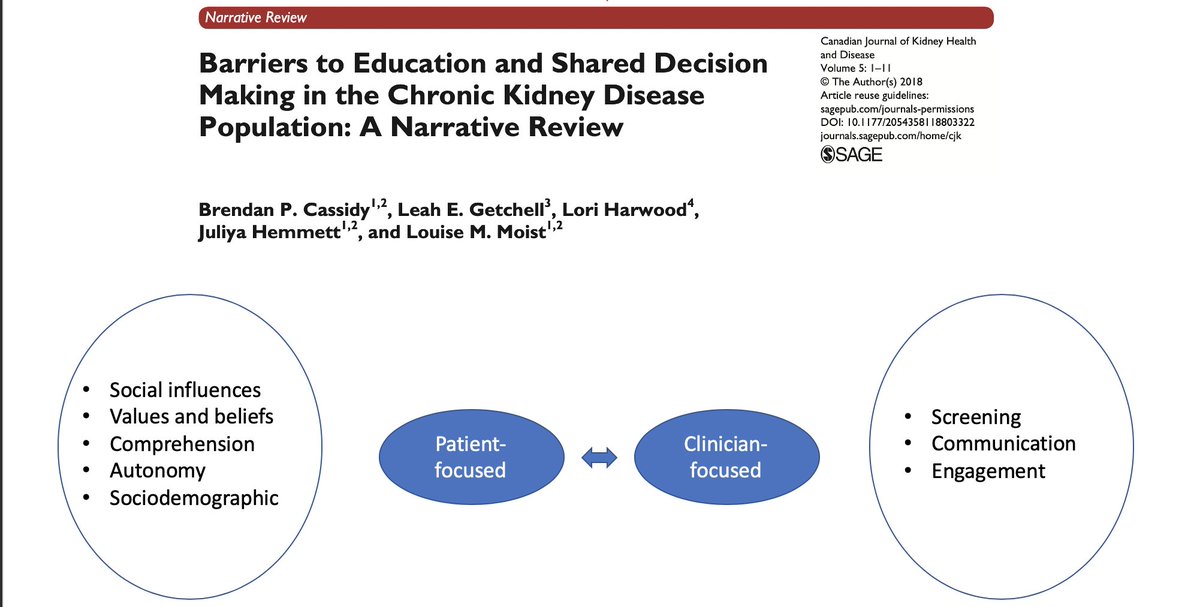
13/ Factoring patient choice in "shared" decision-making is challenging as one has to address patient values, beliefs, health literacy & cognitive deficits. But there are ways around these challenges
https://rebrand.ly/9kyonhg
https://rebrand.ly/9kyonhg&q... href=" https://rebrand.ly/p8m6ajg ">https://rebrand.ly/p8m6ajg&q...
https://rebrand.ly/9kyonhg
14/ Another very useful resource is this website that offers training modules in communication about supportive care; and the RPA guidelines that discuss dialysis initiation and withdrawal:
http://nephro-talk.com"> http://nephro-talk.com
http://nephro-talk.com"> http://nephro-talk.com
15/ Here& #39;s a new definition:
"A well-informed patient that chooses a treatment that brings her closest to the outcomes she wants to have is a patient that’s made the right decision!"
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6988330/">https://www.ncbi.nlm.nih.gov/pmc/artic...
"A well-informed patient that chooses a treatment that brings her closest to the outcomes she wants to have is a patient that’s made the right decision!"
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6988330/">https://www.ncbi.nlm.nih.gov/pmc/artic...

 Read on Twitter
Read on Twitter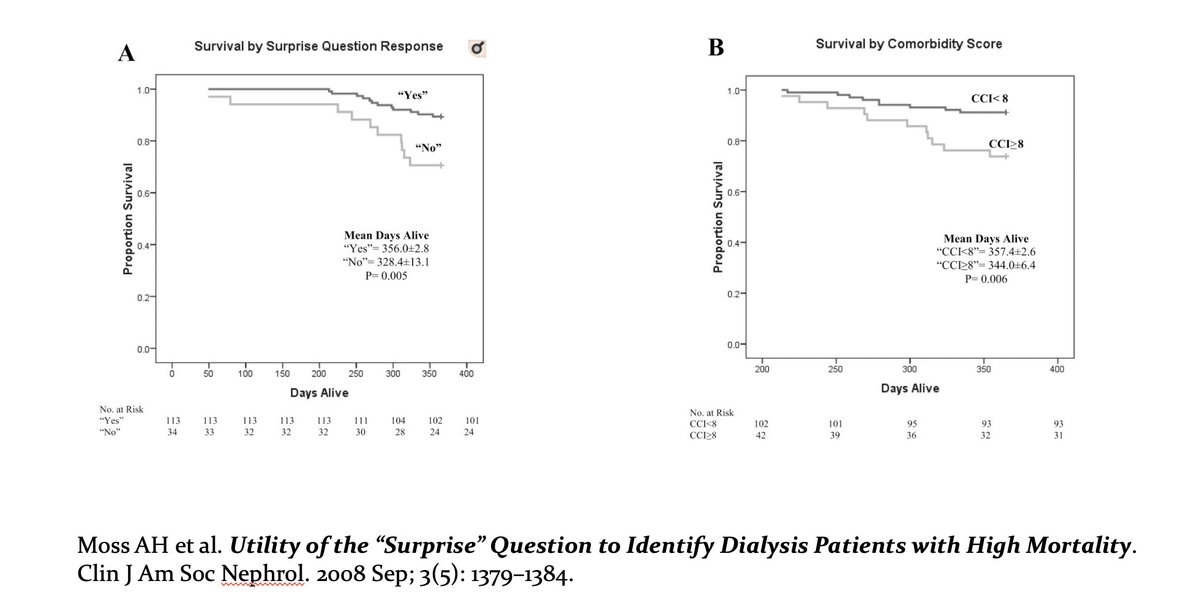
 https://www.ncbi.nlm.nih.gov/pubmed/22..." title="5/ Few things are as hard as choosing between dialysis or no-dialysis. Patients may think conservative care is not an option, or that there is no real choice:that it& #39;s dialysis or death! https://www.sciencedirect.com/science/a... href=" https://www.ncbi.nlm.nih.gov/pubmed/22560169 ">https://www.ncbi.nlm.nih.gov/pubmed/22..." class="img-responsive" style="max-width:100%;"/>
https://www.ncbi.nlm.nih.gov/pubmed/22..." title="5/ Few things are as hard as choosing between dialysis or no-dialysis. Patients may think conservative care is not an option, or that there is no real choice:that it& #39;s dialysis or death! https://www.sciencedirect.com/science/a... href=" https://www.ncbi.nlm.nih.gov/pubmed/22560169 ">https://www.ncbi.nlm.nih.gov/pubmed/22..." class="img-responsive" style="max-width:100%;"/>
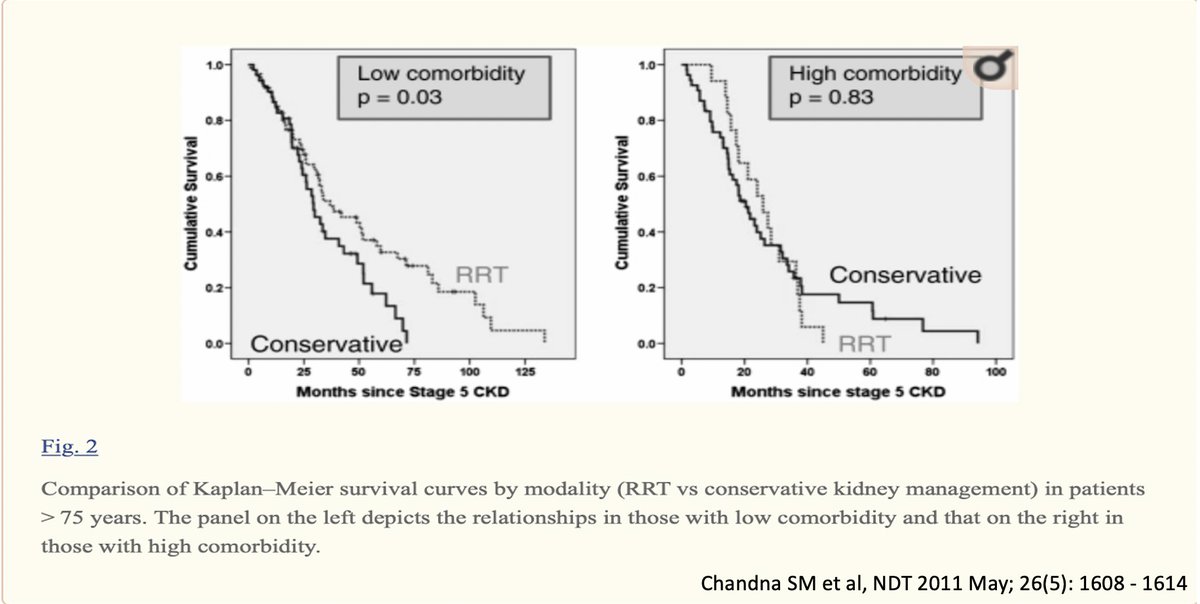 https://www.ncbi.nlm.nih.gov/pubmed/23..." title="8/ Survival isn& #39;t an ideal yardstick - especially if this at the cost of a lower QOL. With multiple comorbidities, being on dialysis may not even alter survival! https://www.ncbi.nlm.nih.gov/pmc/artic... href=" https://www.ncbi.nlm.nih.gov/pubmed/23652841 ">https://www.ncbi.nlm.nih.gov/pubmed/23..." class="img-responsive" style="max-width:100%;"/>
https://www.ncbi.nlm.nih.gov/pubmed/23..." title="8/ Survival isn& #39;t an ideal yardstick - especially if this at the cost of a lower QOL. With multiple comorbidities, being on dialysis may not even alter survival! https://www.ncbi.nlm.nih.gov/pmc/artic... href=" https://www.ncbi.nlm.nih.gov/pubmed/23652841 ">https://www.ncbi.nlm.nih.gov/pubmed/23..." class="img-responsive" style="max-width:100%;"/>
 https://rebrand.ly/p8m6ajg&q..." title="13/ Factoring patient choice in "shared" decision-making is challenging as one has to address patient values, beliefs, health literacy & cognitive deficits. But there are ways around these challenges https://rebrand.ly/9kyonhg&q... href=" https://rebrand.ly/p8m6ajg ">https://rebrand.ly/p8m6ajg&q..." class="img-responsive" style="max-width:100%;"/>
https://rebrand.ly/p8m6ajg&q..." title="13/ Factoring patient choice in "shared" decision-making is challenging as one has to address patient values, beliefs, health literacy & cognitive deficits. But there are ways around these challenges https://rebrand.ly/9kyonhg&q... href=" https://rebrand.ly/p8m6ajg ">https://rebrand.ly/p8m6ajg&q..." class="img-responsive" style="max-width:100%;"/>