CD8+ T cells play an important role in clearing respiratory virus. I looked at 10 preprints from @biorxivpreprint and @medrxivpreprint all exploring T cell responses to #SARS2/ #COVID19. In no particular order, here’s what I found interesting, and then some comments below. 1/17
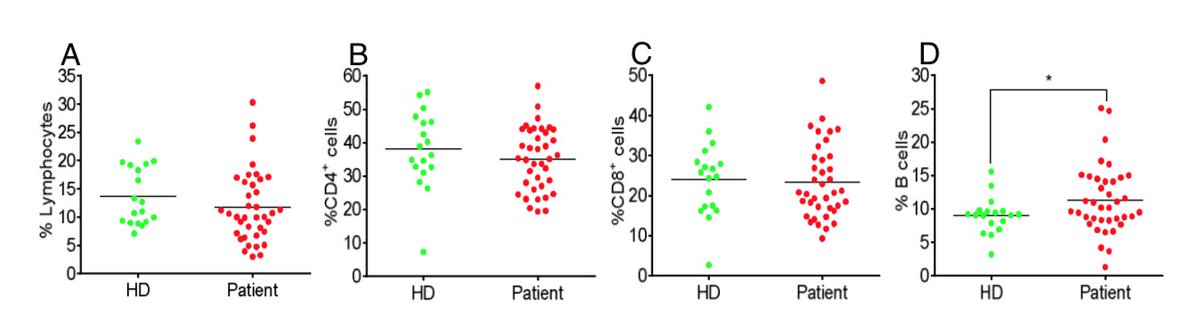
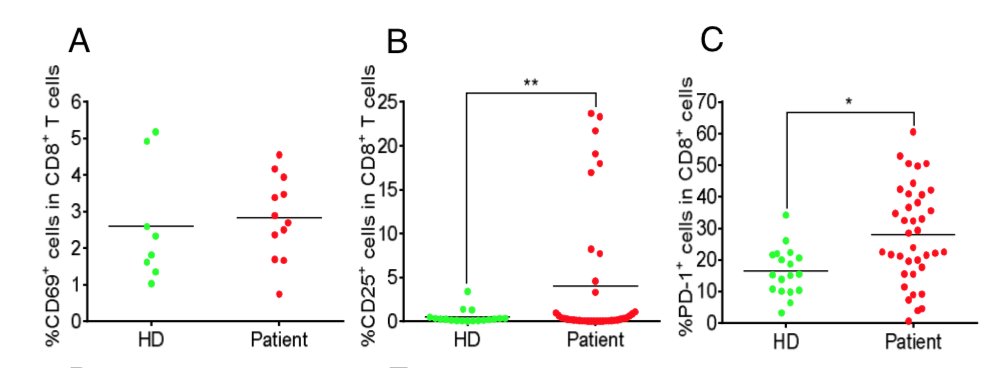
First up. Yang et al, looked at PBMCs from 38 #SARSCoV2 patients and 18 health donors: https://www.medrxiv.org/content/10.1101/2020.03.23.20040675v2.">https://www.medrxiv.org/content/1... CD8+ T cells were more activated (CD69+, CD25+, PD1+), but no T-cell-penia.
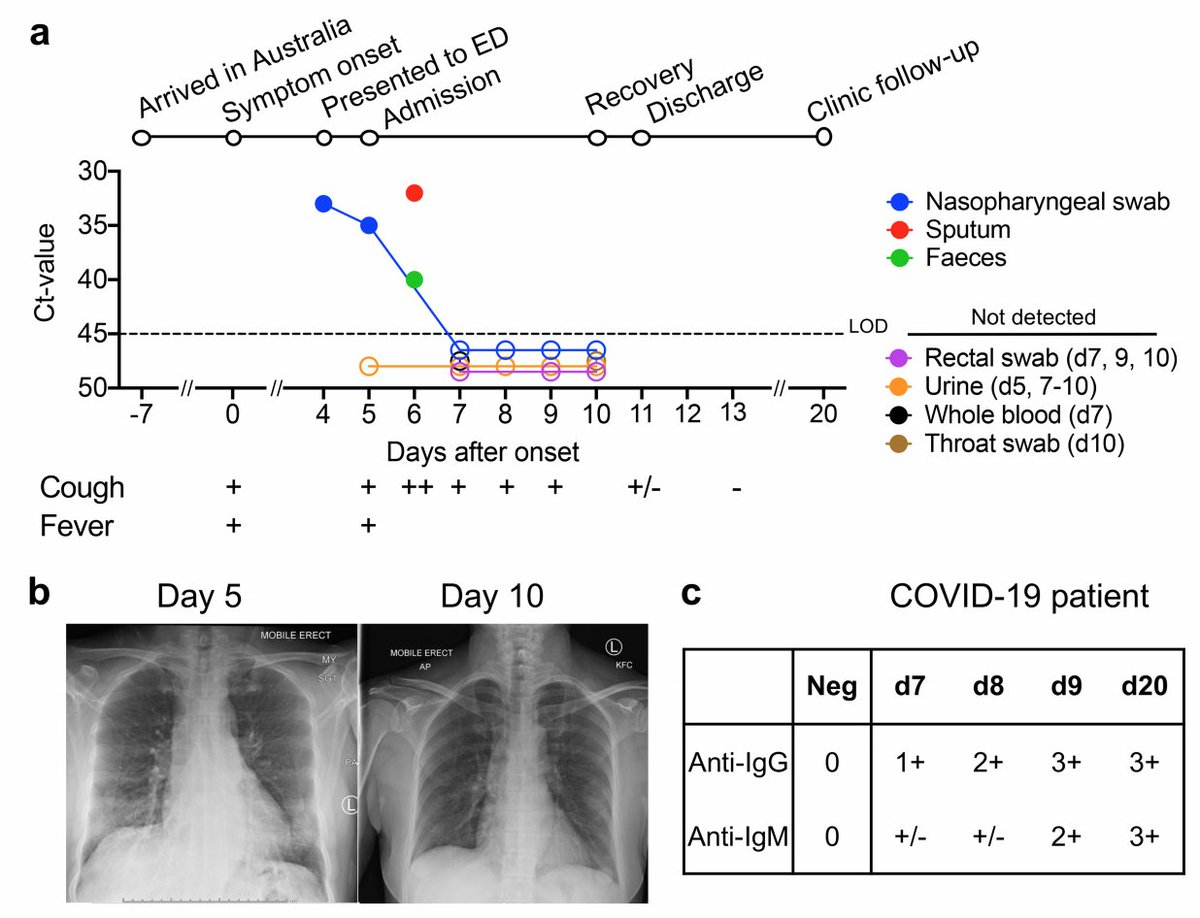
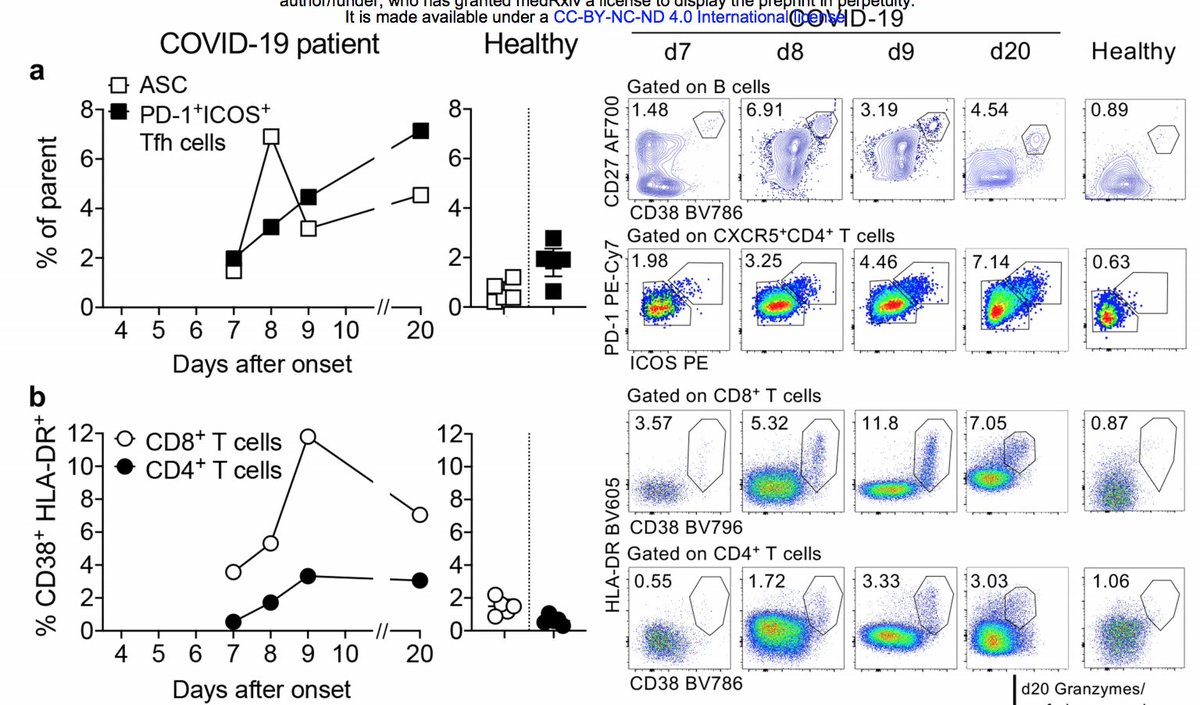
Thevarajan et al ( https://www.medrxiv.org/content/10.1101/2020.02.20.20025841v1)">https://www.medrxiv.org/content/1... looked at one patient with mild symptoms. CD8 T cells were activated (based on HLA-DR/CD38) and produced effector cytokines by day 7, increased by day 9, and decreased by day 20 as virus was cleared. Activation preceded viral clearance.
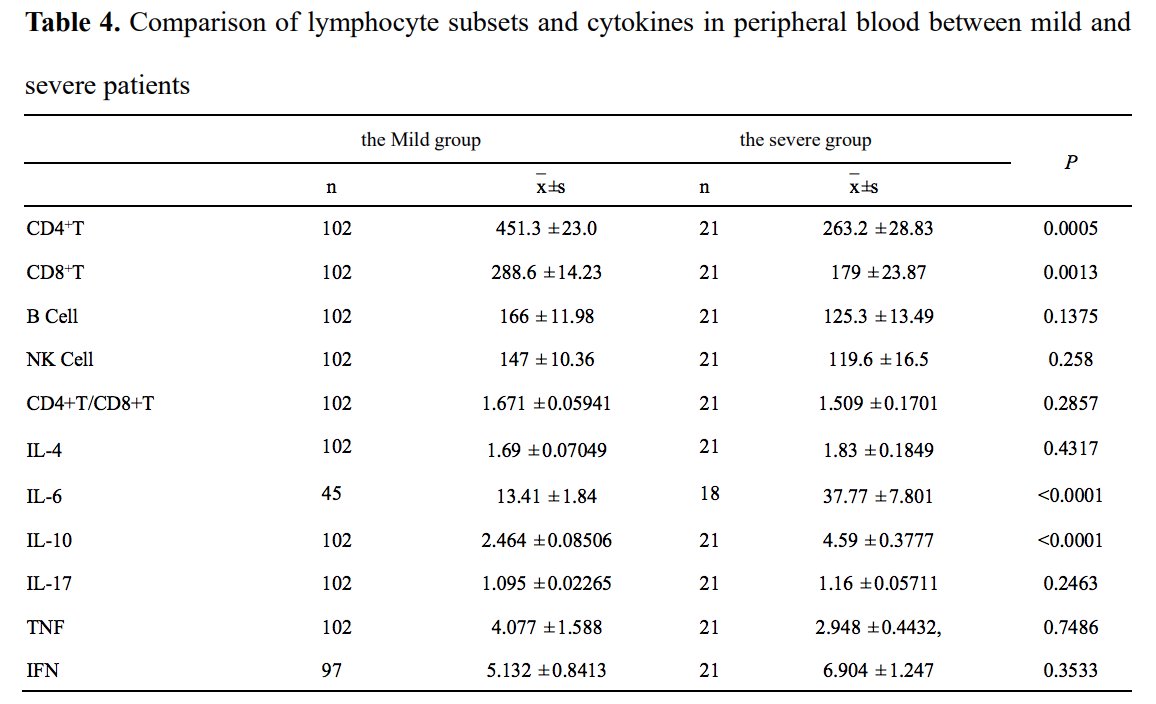
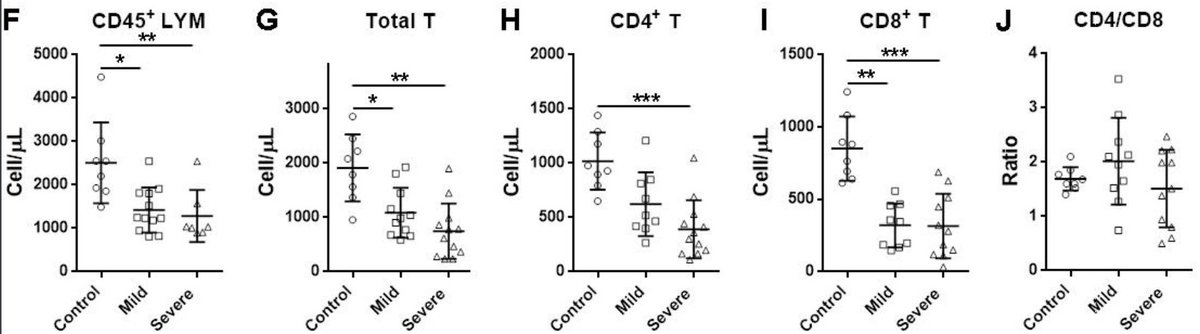
Wan et al ( https://www.medrxiv.org/content/10.1101/2020.02.10.20021832v1)">https://www.medrxiv.org/content/1... looked at 123 hospitalized patients (103 mild and 21 severely ill). In PBMCs, there were fewer CD4 and CD8 cells in the severe group; and more IL-6. No difference in CD4/CD8 ratios. 4/17
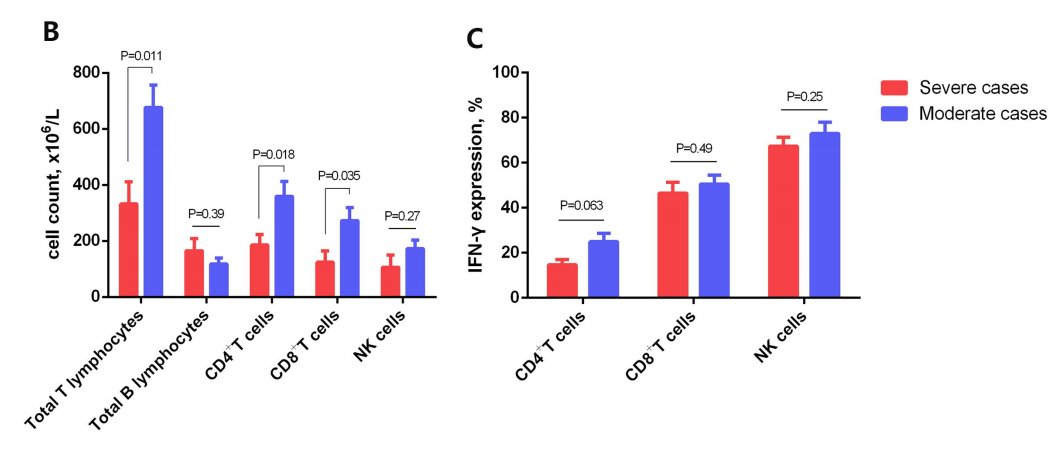
Chen et al ( https://www.medrxiv.org/content/10.1101/2020.02.16.20023903v1)">https://www.medrxiv.org/content/1... looked at 21 patients (10 moderatly and 11 severely ill). Reduced cell count of CD4 and CD8+ T cell counts in severely ill patients, but similar number of IFNy+ T cells cells between groups. 5/17
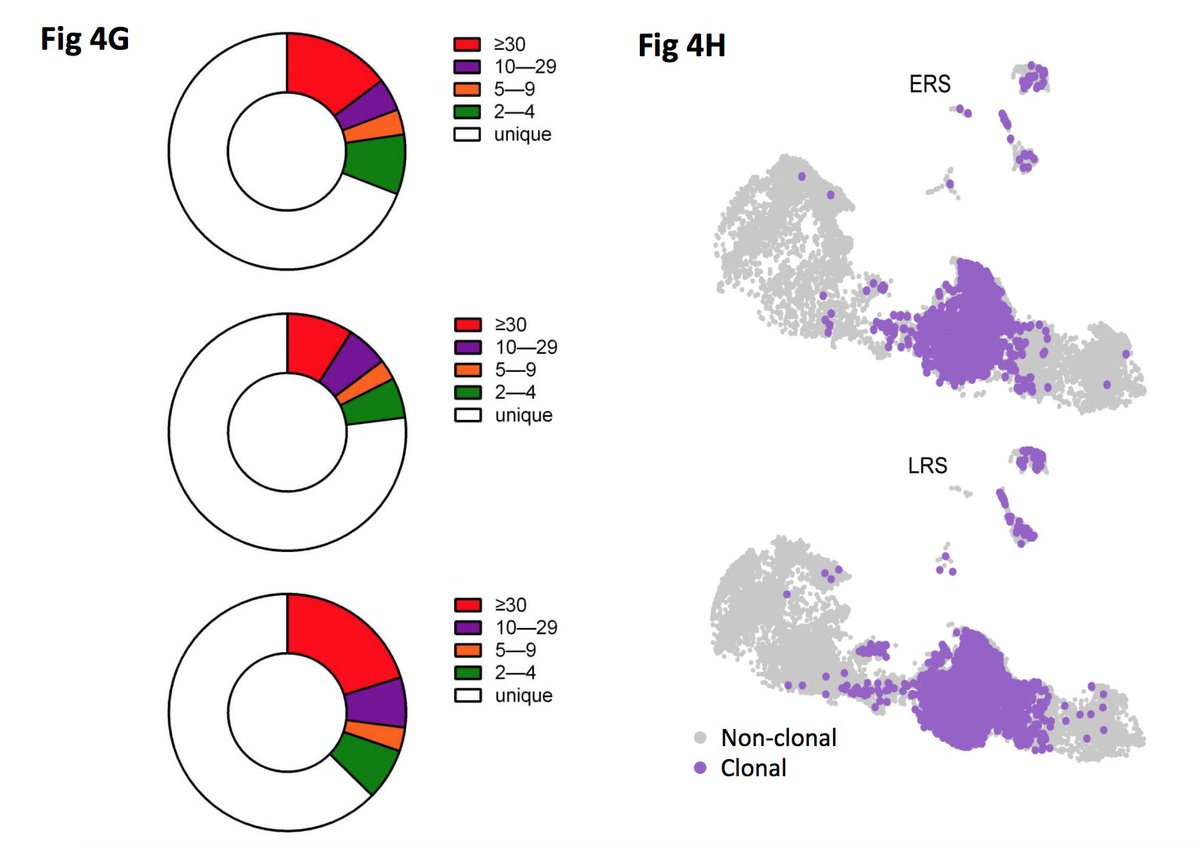
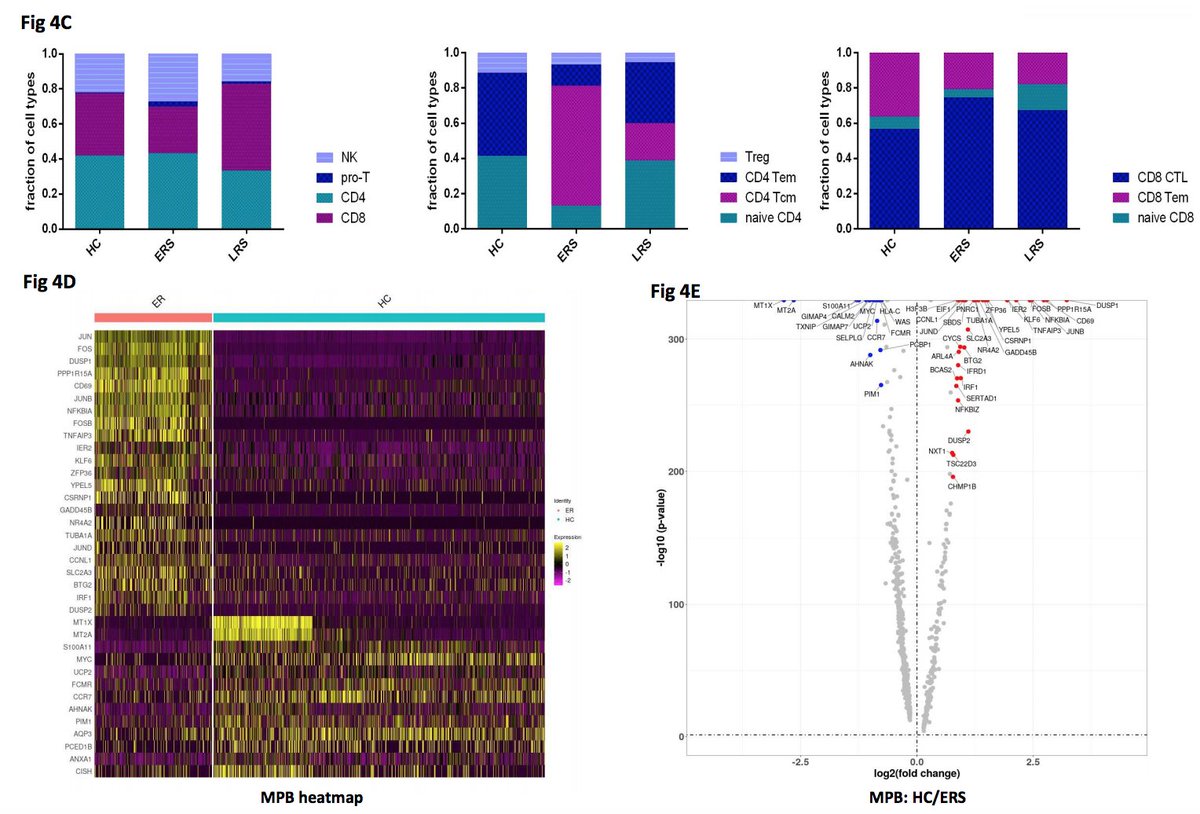
Wen et al ( https://www.medrxiv.org/content/10.1101/2020.03.23.20039362v2)">https://www.medrxiv.org/content/1... used scRNASeq to examine healthy controls, early (ERS) and late patients recovering. ERS patients had less CD8+ cells in periphery but more effectors. Found clonally expanded CD8s that had an inflammatory phenotype but data not shown? 6/17
Shi et al ( https://www.medrxiv.org/content/10.1101/2020.03.12.20034736v1).">https://www.medrxiv.org/content/1... Controls, 31 mild and 25 severer cases were compared. CD4 and CD8s reduced in all infected cases in PBMCs. No change in CD4/CD8 ratio. Speculate that T cells are being recruited to infectious sites. 7/17
Campbell et al ( https://www.biorxiv.org/content/10.1101/2020.03.30.016931v1)">https://www.biorxiv.org/content/1... predicted 30 HLA class I epitopes; 10 predicted epitopes overlapped with SARS-CoV epitopes. 8/17
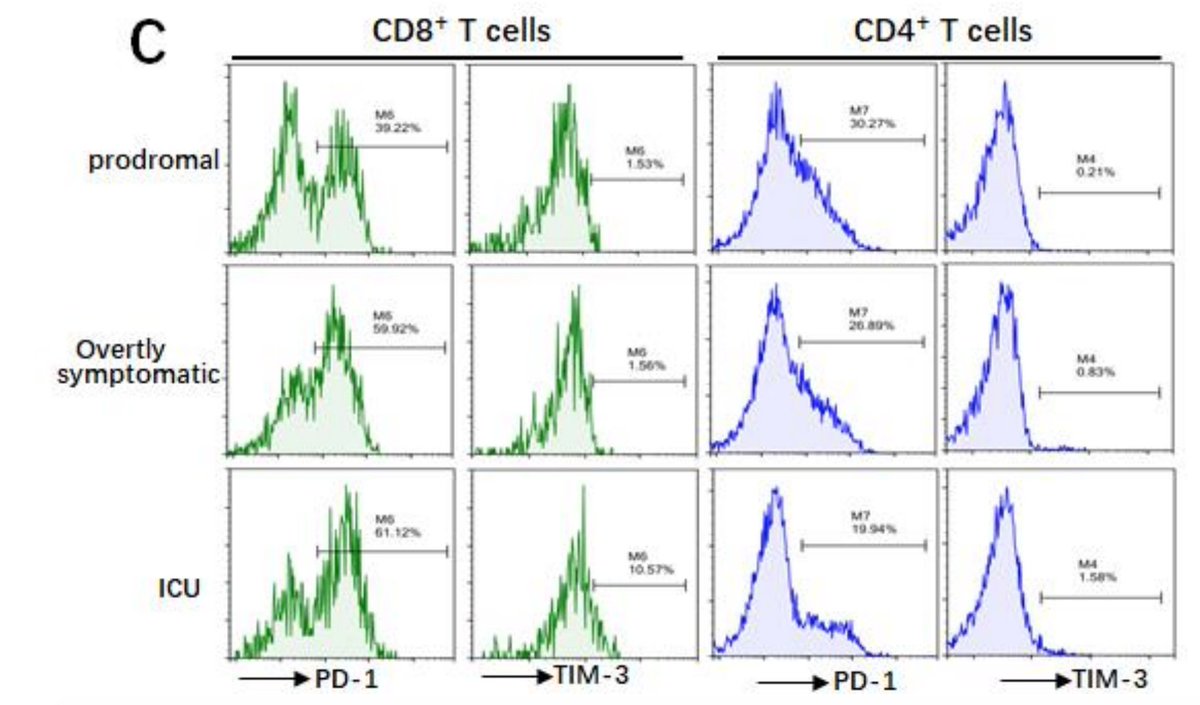
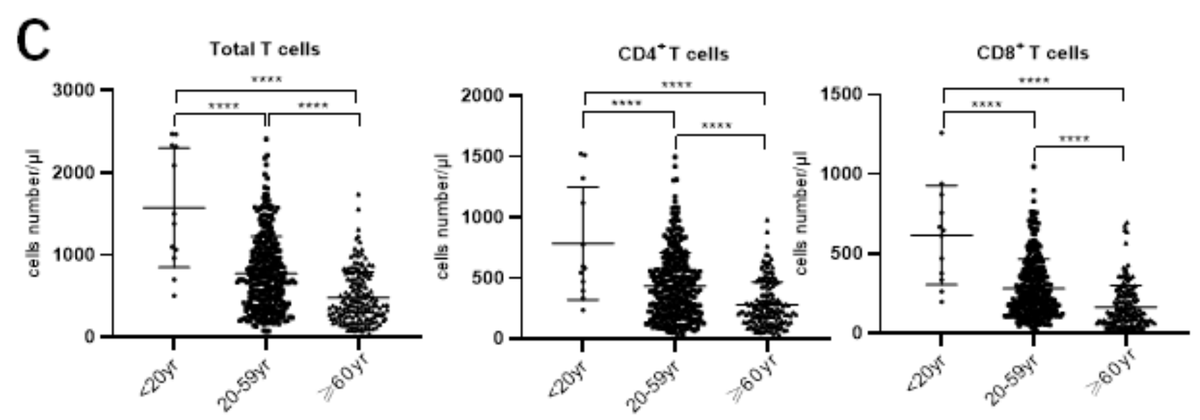
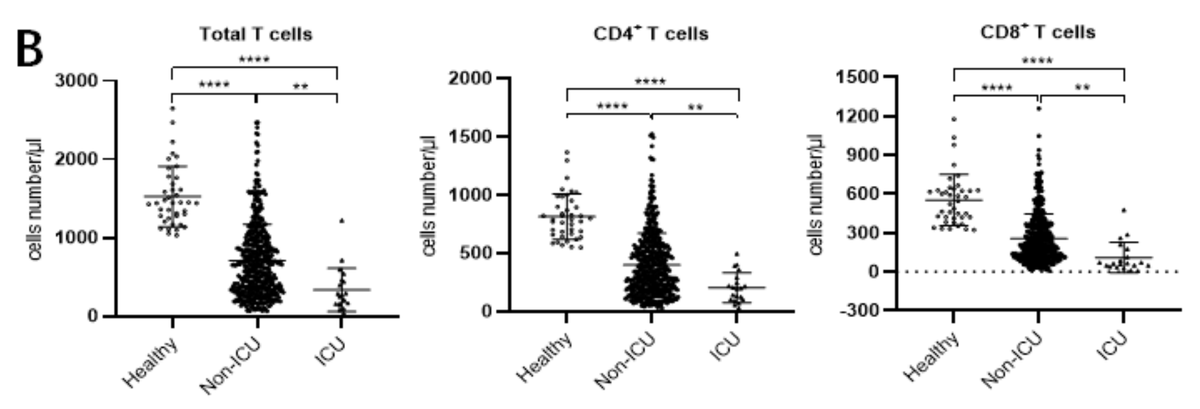
Diao et al ( https://www.medrxiv.org/content/10.1101/2020.02.18.20024364v1)">https://www.medrxiv.org/content/1... examined 499 patients. The more severe COVID19, the fewer T cells in the periphery. Pts > 60 years had fewer T cells. Cell # correlate weakly to cytokine levels. And T cells in affected cases expressed ‘exhaustion” makers PD1 and TIM3. 9/17
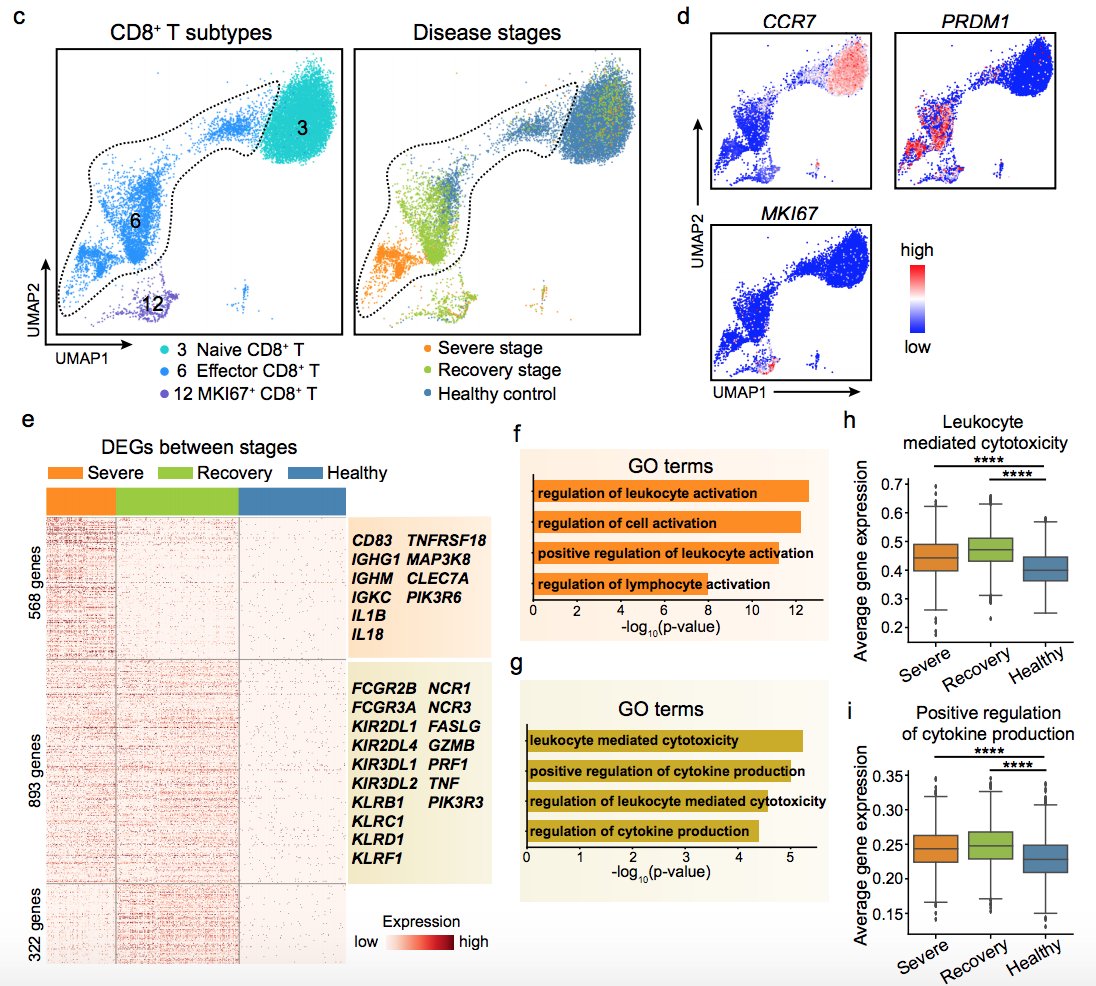
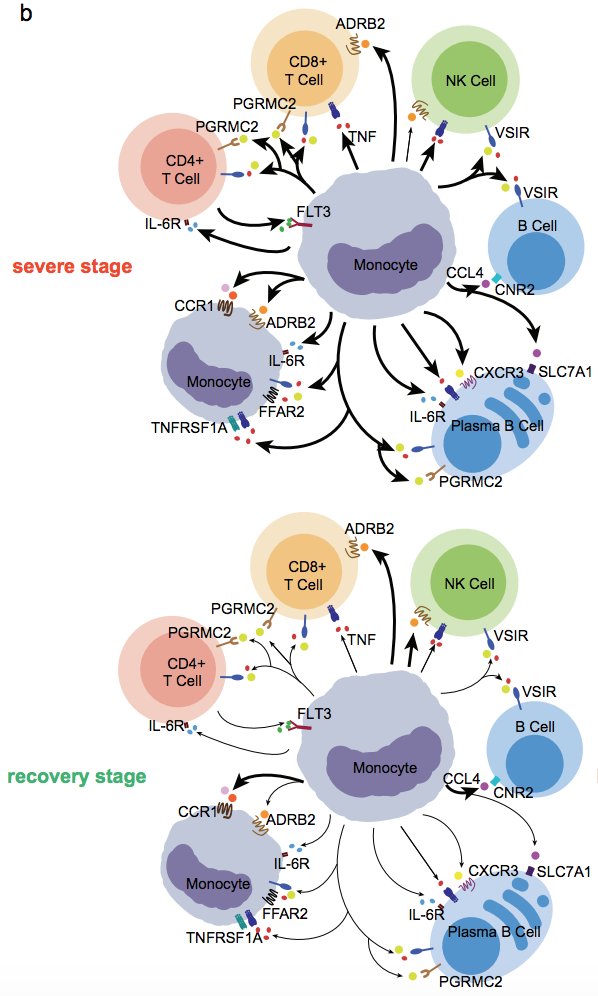
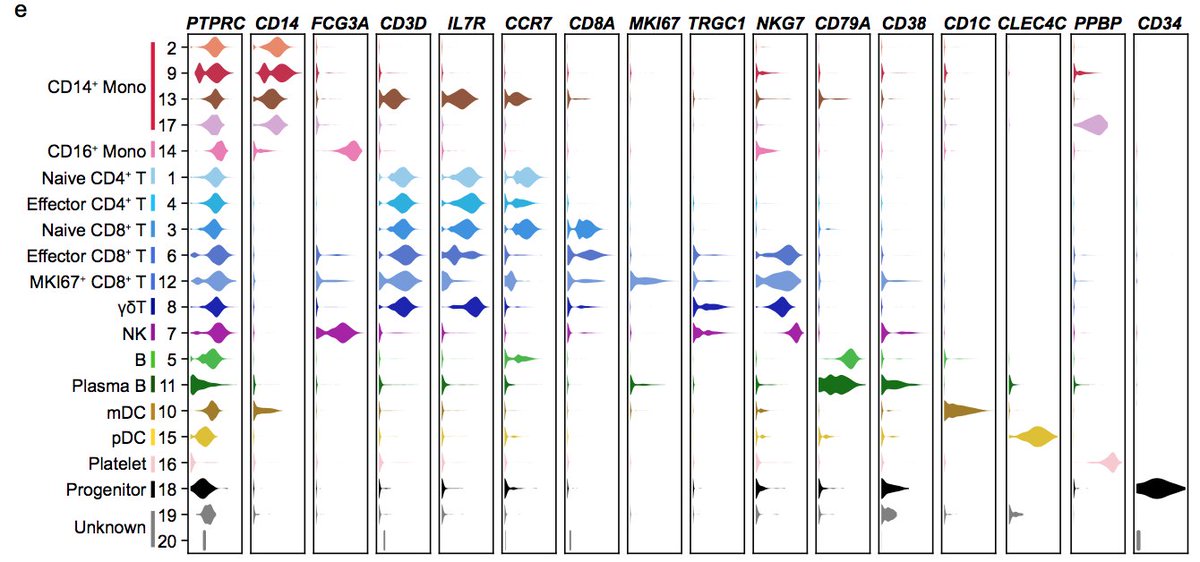
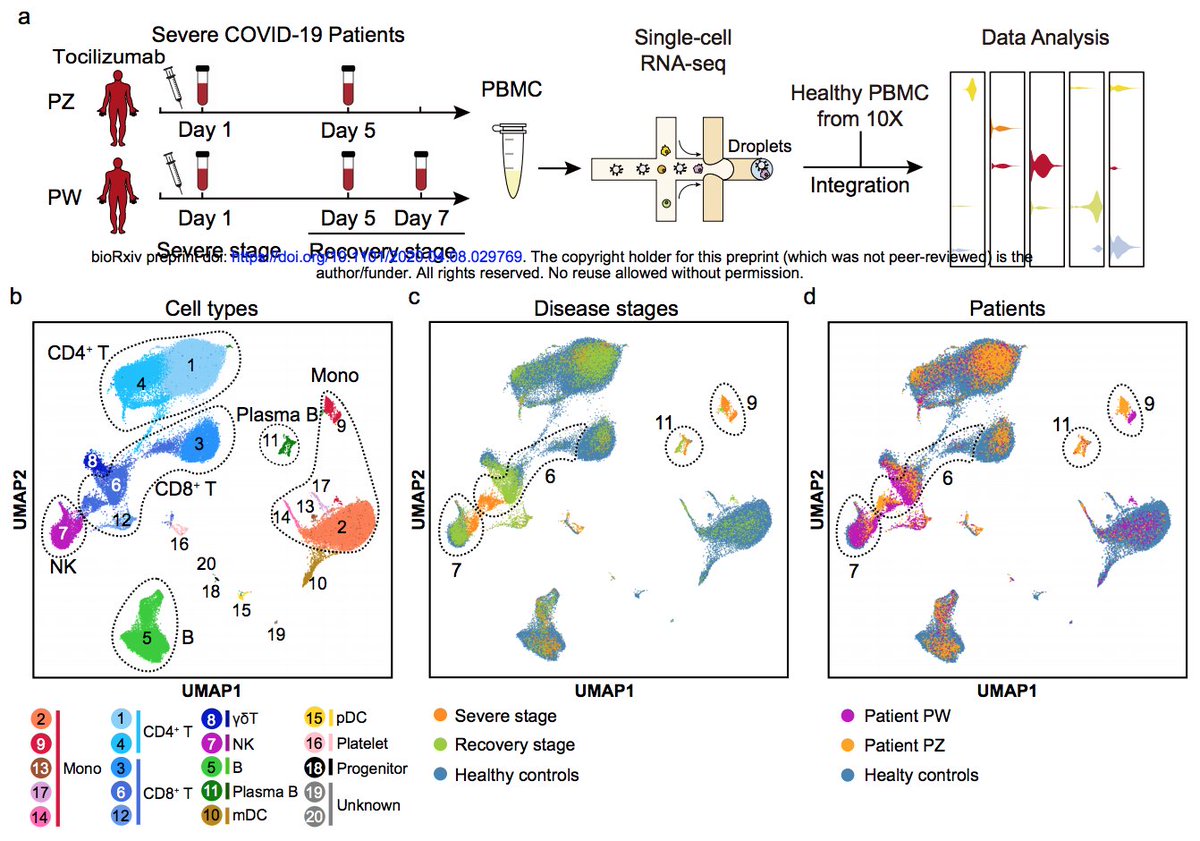
Guo et al ( https://biorxiv.org/content/10.1101/2020.04.08.029769v1)">https://biorxiv.org/content/1... used scRNAseq on immune cells in 2 pts during treatment with anti-IL6 and recovery. Monocytes directs CD4 T cells through IL6. CD8s in severe patients had an effector genotype. High effector cytokine levels in on-going and recovery stage. 10/17
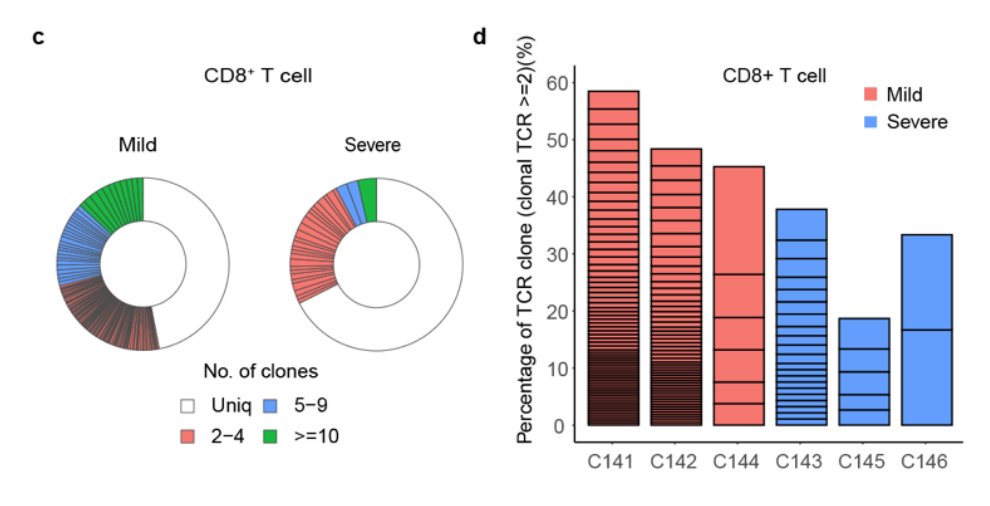
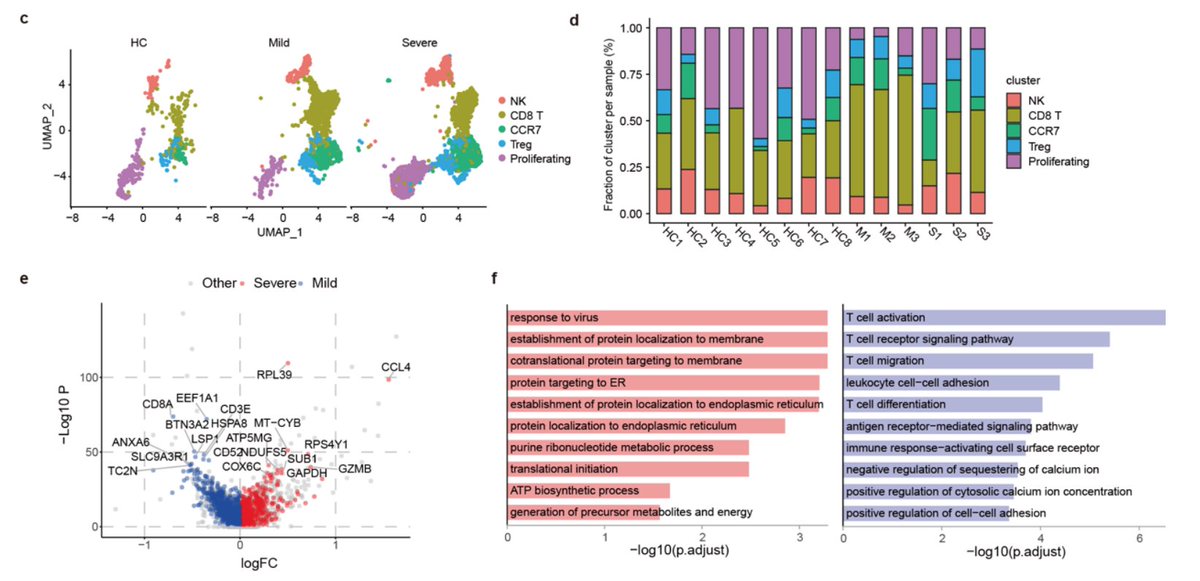
Liao et al ( https://www.medrxiv.org/content/10.1101/2020.02.23.20026690v1)">https://www.medrxiv.org/content/1... did scRNA/TCR-seq on BAL in 3 mild/3 severe cases. Increased T cells #’s in lungs, less so in severe pts, where cells had proliferative profile. All had effector genotype. Found clonally expanded clones and more so in mild cases. 11/17
Some comments: 1) impressive effort of all authors: under an emerging epidemic, they collected, analyzed and report these findings! 2) Methods are lacking in some papers. 3) Most data on PBMCs. 4) More advanced methods done on low # of patients at random time-points. 12/17
My feeling from reading these papers is that the T cell response is ramped up early on, cells get activated and traffic to infectious sites, where they increase cytotoxicity. Low numbers in periphery most likely because of this redirection. Looks like textbook immunology. 13/17
One point: seems most patients develop a functional T cell response. To me this does not indicate that the virus specifically inhibits T cells as might be inferred from a paper by Wang et al ( https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7136698/).">https://www.ncbi.nlm.nih.gov/pmc/artic... PD1 expression does not mean exhaustion just activation. 14/17
Thevarajan et al reveal that T cell response preceeds viral clearance. Guo et al data also indicate effectors stay after clearance, at least short term. Liao et al’s paper looking at cellular interaction in BAL finds clonally expanded effectors. All in all: T cells matter. 15/17
Comparison between mild and severe patients important. Cytokine “mis-communication” produced by monocytes/macrophages and effects on T cells a major theme. Do severe cases have poor T cell clones/expansion? Do older patients have lower #& #39;s or poor initial response? 16/17
Next step I think are tetramers. Campbell et al’s study indicate that some from SARS-Cov might be cross-reactive and could be used. Bigger sample groups, analyzed in timed manner. Important to keep focus on older population and mild/severe cases. Fin. 17/17

 Read on Twitter
Read on Twitter