some pearls from an article by Martin Tobin about when to intubate patients with COVID (yep, the same one who edited Tobin& #39;s textbook on mechanical ventilation)... ( #1/6)
(full article: https://bit.ly/2XDgovQ )">https://bit.ly/2XDgovQ&q...
(full article: https://bit.ly/2XDgovQ )">https://bit.ly/2XDgovQ&q...
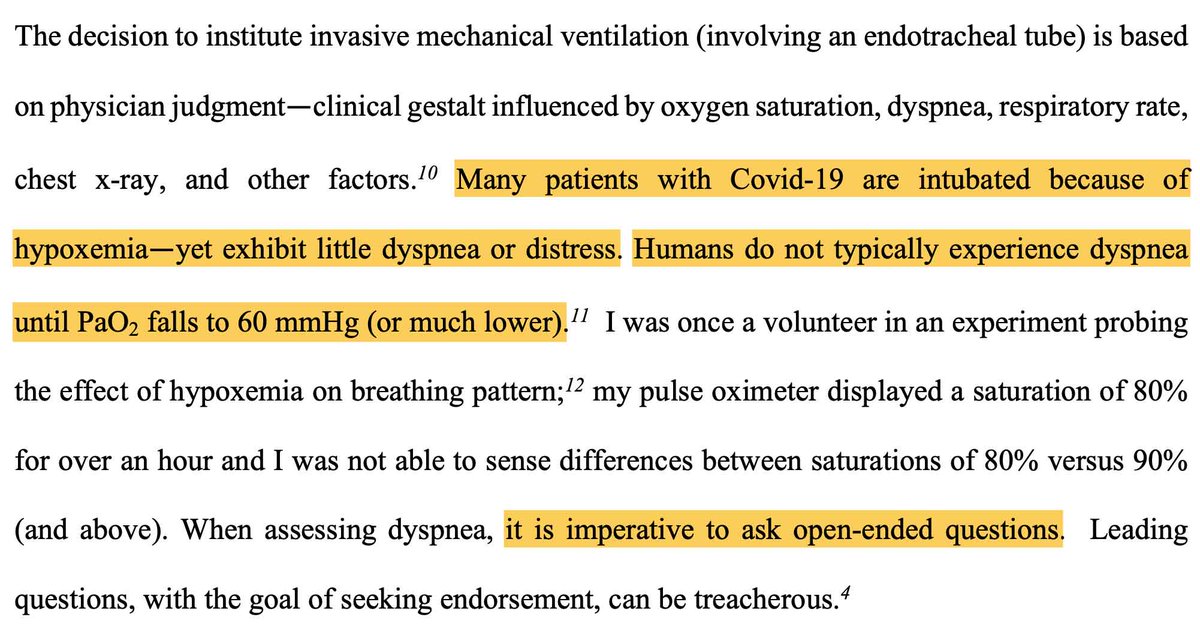
hypoxemia is rarely a clinically relevant cause of dyspnea. it& #39;s essential to think about oxygenation & ventilation *separately.* (for example: a hypoxemic COVID patient without chronic lung disease who is mentating normally & not dyspneic is probably *not* hypercapneic).( #2/6)
also, tachypnea must be teased apart from an increased work of breathing. a tachypneic patient who looks & feels well probably doesn& #39;t have an excessive work of breathing. high work of breathing is more worrisome than tachypnea regarding progressive diaphragmatic fatigue. ( #3/6)
dramatic infiltrates are not an indication for intubation (physiology is more important than radiology!). however, dramatic infiltrates *do* suggest a higher risk of deterioration - and may indicate a need for closer monitoring. ( #4/6)
survival depends on tissue oxygen delivery (not oxygen saturation). euvolemic patients with normal hemoglobin concentration and cardiac reserve generally do fine with an oxygen saturation in the 80s. ( #5/6)
ultimately, nobody knows the optimal trigger for intubating COVID patients. hopefully these concepts might help a bit in these enormously challenging bedside decisions. when in doubt, consider asking a colleague for a second opinion & seeing how the patient evolves over time.

 Read on Twitter
Read on Twitter