This one has lots of clues for our understanding of #COVID19 and heavily implicates mononuclear phagocytes as central to severe pathology.
A thread....
https://www.biorxiv.org/content/10.1101/2020.04.08.029769v1">https://www.biorxiv.org/content/1...
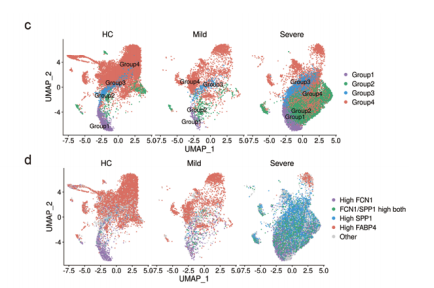
They sampled #PBMC from severe and recovery stage #COVID19 and integrated data with reference healthy #PBMC
Fairly standard cell type annotation.
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤩" title="Star-struck" aria-label="Emoji: Star-struck">Recovery stage samples are after Tocilizumab - anti-IL6R monoclonal Ab
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤩" title="Star-struck" aria-label="Emoji: Star-struck">Recovery stage samples are after Tocilizumab - anti-IL6R monoclonal Ab https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤩" title="Star-struck" aria-label="Emoji: Star-struck">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤩" title="Star-struck" aria-label="Emoji: Star-struck">
Fairly standard cell type annotation.
Fairly standard cell type annotation.
This bit is easy for PBMC nowadays and can be semi automated... https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤨" title="Face with raised eyebrow" aria-label="Emoji: Face with raised eyebrow">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤨" title="Face with raised eyebrow" aria-label="Emoji: Face with raised eyebrow">
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Cluster 13 are clearly T-mono doublets. Maybe these are physiological? Evidence of physical interaction/crosstalk?
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Cluster 13 are clearly T-mono doublets. Maybe these are physiological? Evidence of physical interaction/crosstalk?  https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤷♂️" title="Man shrugging" aria-label="Emoji: Man shrugging">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤷♂️" title="Man shrugging" aria-label="Emoji: Man shrugging">
This bit is easy for PBMC nowadays and can be semi automated...
https://www.medrxiv.org/content/10.1101/2020.02.23.20026690v1.full.pdf">https://www.medrxiv.org/content/1... inflammatory monocyte/macrophage population in bronchoalveolar lavage fluid
Back to the tocilizumab study...
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">They also see prominent plasma cells which recede during recovery, and are rare in health.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">They also see prominent plasma cells which recede during recovery, and are rare in health.
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">There are some proliferating and effector CD8 T cells expressing PRDM1.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">There are some proliferating and effector CD8 T cells expressing PRDM1.
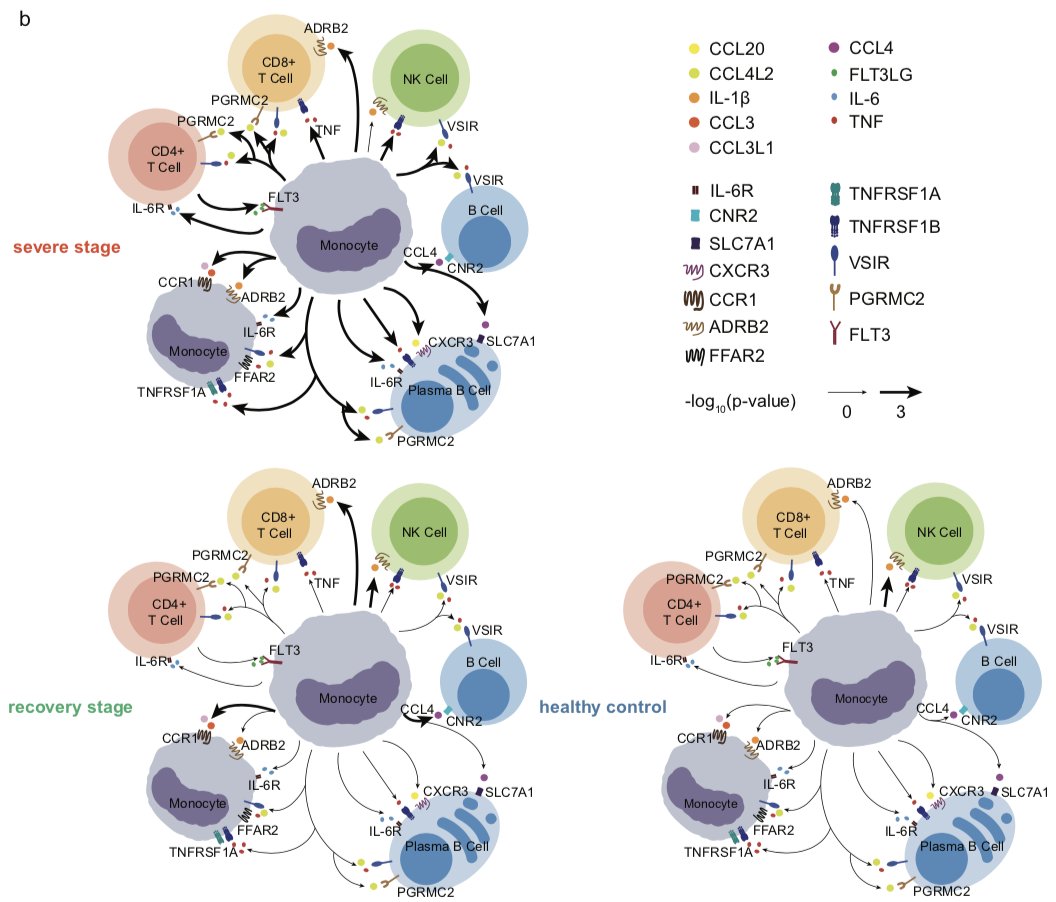
Authors looked at putative interactions using CellPhoneDB -  https://abs.twimg.com/emoji/v2/... draggable="false" alt="💪" title="Flexed biceps" aria-label="Emoji: Flexed biceps">tool developed by @teichlab @mirjana_e @roserventotormo
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💪" title="Flexed biceps" aria-label="Emoji: Flexed biceps">tool developed by @teichlab @mirjana_e @roserventotormo  https://abs.twimg.com/emoji/v2/... draggable="false" alt="💪" title="Flexed biceps" aria-label="Emoji: Flexed biceps">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💪" title="Flexed biceps" aria-label="Emoji: Flexed biceps">
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Severe stage enriched for mono->lymphocyte signalling
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Severe stage enriched for mono->lymphocyte signalling
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Some IL6-IL6R signalling
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Some IL6-IL6R signalling  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Downwards arrow" aria-label="Emoji: Downwards arrow"> after tocilizumab
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Downwards arrow" aria-label="Emoji: Downwards arrow"> after tocilizumab
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">severe stage monos signal -> plasma cells ++
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">severe stage monos signal -> plasma cells ++
Overall model is that in severe #COVID19, monocytes are v activated and signal to lymphocytes incl plasma cells to orchestrate the phenotype...
Tentative implications:
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🚫" title="No entry sign" aria-label="Emoji: No entry sign">Need to break myeloid/innate activation - that seems proximal.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🚫" title="No entry sign" aria-label="Emoji: No entry sign">Need to break myeloid/innate activation - that seems proximal.
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="💊" title="Pill" aria-label="Emoji: Pill">IL6 blockade seems well motivated given these data
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💊" title="Pill" aria-label="Emoji: Pill">IL6 blockade seems well motivated given these data
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="💊" title="Pill" aria-label="Emoji: Pill">Inflammasome blockade also worth trying
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💊" title="Pill" aria-label="Emoji: Pill">Inflammasome blockade also worth trying

 Read on Twitter
Read on Twitter #singlecell #COVID19 paper alerthttps://abs.twimg.com/emoji/v2/... draggable="false" alt="🚨" title="Police cars revolving light" aria-label="Emoji: Police cars revolving light">This one has lots of clues for our understanding of #COVID19 and heavily implicates mononuclear phagocytes as central to severe pathology.A thread.... https://www.biorxiv.org/content/1..." title="https://abs.twimg.com/emoji/v2/... draggable="false" alt="🚨" title="Police cars revolving light" aria-label="Emoji: Police cars revolving light"> #singlecell #COVID19 paper alerthttps://abs.twimg.com/emoji/v2/... draggable="false" alt="🚨" title="Police cars revolving light" aria-label="Emoji: Police cars revolving light">This one has lots of clues for our understanding of #COVID19 and heavily implicates mononuclear phagocytes as central to severe pathology.A thread.... https://www.biorxiv.org/content/1..." class="img-responsive" style="max-width:100%;"/>
#singlecell #COVID19 paper alerthttps://abs.twimg.com/emoji/v2/... draggable="false" alt="🚨" title="Police cars revolving light" aria-label="Emoji: Police cars revolving light">This one has lots of clues for our understanding of #COVID19 and heavily implicates mononuclear phagocytes as central to severe pathology.A thread.... https://www.biorxiv.org/content/1..." title="https://abs.twimg.com/emoji/v2/... draggable="false" alt="🚨" title="Police cars revolving light" aria-label="Emoji: Police cars revolving light"> #singlecell #COVID19 paper alerthttps://abs.twimg.com/emoji/v2/... draggable="false" alt="🚨" title="Police cars revolving light" aria-label="Emoji: Police cars revolving light">This one has lots of clues for our understanding of #COVID19 and heavily implicates mononuclear phagocytes as central to severe pathology.A thread.... https://www.biorxiv.org/content/1..." class="img-responsive" style="max-width:100%;"/>
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Cluster 13 are clearly T-mono doublets. Maybe these are physiological? Evidence of physical interaction/crosstalk? https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤷♂️" title="Man shrugging" aria-label="Emoji: Man shrugging">" title="Fairly standard cell type annotation.This bit is easy for PBMC nowadays and can be semi automated... https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤨" title="Face with raised eyebrow" aria-label="Emoji: Face with raised eyebrow">https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Cluster 13 are clearly T-mono doublets. Maybe these are physiological? Evidence of physical interaction/crosstalk? https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤷♂️" title="Man shrugging" aria-label="Emoji: Man shrugging">">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Cluster 13 are clearly T-mono doublets. Maybe these are physiological? Evidence of physical interaction/crosstalk? https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤷♂️" title="Man shrugging" aria-label="Emoji: Man shrugging">" title="Fairly standard cell type annotation.This bit is easy for PBMC nowadays and can be semi automated... https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤨" title="Face with raised eyebrow" aria-label="Emoji: Face with raised eyebrow">https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Cluster 13 are clearly T-mono doublets. Maybe these are physiological? Evidence of physical interaction/crosstalk? https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤷♂️" title="Man shrugging" aria-label="Emoji: Man shrugging">">
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Cluster 13 are clearly T-mono doublets. Maybe these are physiological? Evidence of physical interaction/crosstalk? https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤷♂️" title="Man shrugging" aria-label="Emoji: Man shrugging">" title="Fairly standard cell type annotation.This bit is easy for PBMC nowadays and can be semi automated... https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤨" title="Face with raised eyebrow" aria-label="Emoji: Face with raised eyebrow">https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Cluster 13 are clearly T-mono doublets. Maybe these are physiological? Evidence of physical interaction/crosstalk? https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤷♂️" title="Man shrugging" aria-label="Emoji: Man shrugging">">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Cluster 13 are clearly T-mono doublets. Maybe these are physiological? Evidence of physical interaction/crosstalk? https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤷♂️" title="Man shrugging" aria-label="Emoji: Man shrugging">" title="Fairly standard cell type annotation.This bit is easy for PBMC nowadays and can be semi automated... https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤨" title="Face with raised eyebrow" aria-label="Emoji: Face with raised eyebrow">https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Cluster 13 are clearly T-mono doublets. Maybe these are physiological? Evidence of physical interaction/crosstalk? https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤷♂️" title="Man shrugging" aria-label="Emoji: Man shrugging">">
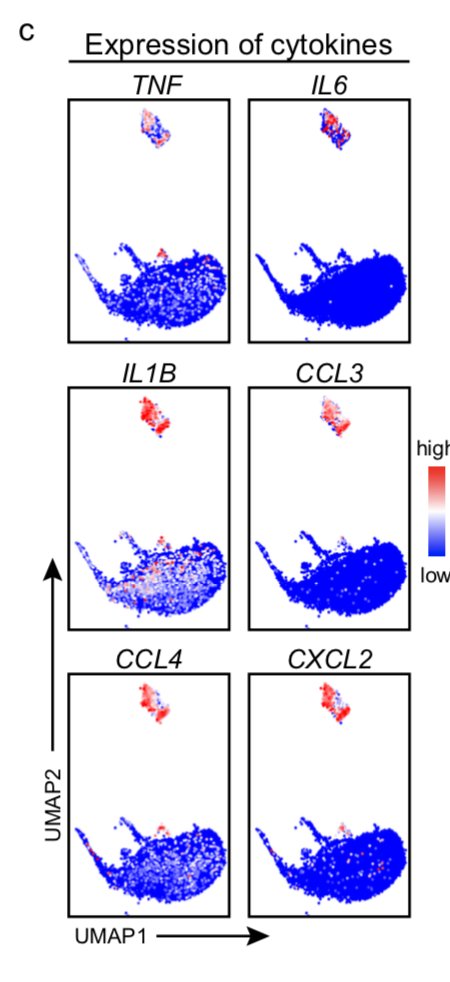 there is a monocyte cluster specific enriched in severe #COVID19 and receding during recovery/anti-IL6R...https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Expressing LOADS of cytokines & chemokineshttps://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol"> #Inflammasome gene upregulation (Il1B, NRLP3)https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Severe #COVID19 monocytes express https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">IL6 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤒" title="Face with thermometer" aria-label="Emoji: Face with thermometer">" title="https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">there is a monocyte cluster specific enriched in severe #COVID19 and receding during recovery/anti-IL6R...https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Expressing LOADS of cytokines & chemokineshttps://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol"> #Inflammasome gene upregulation (Il1B, NRLP3)https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Severe #COVID19 monocytes express https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">IL6 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤒" title="Face with thermometer" aria-label="Emoji: Face with thermometer">">
there is a monocyte cluster specific enriched in severe #COVID19 and receding during recovery/anti-IL6R...https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Expressing LOADS of cytokines & chemokineshttps://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol"> #Inflammasome gene upregulation (Il1B, NRLP3)https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Severe #COVID19 monocytes express https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">IL6 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤒" title="Face with thermometer" aria-label="Emoji: Face with thermometer">" title="https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">there is a monocyte cluster specific enriched in severe #COVID19 and receding during recovery/anti-IL6R...https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Expressing LOADS of cytokines & chemokineshttps://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol"> #Inflammasome gene upregulation (Il1B, NRLP3)https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Severe #COVID19 monocytes express https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">IL6 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤒" title="Face with thermometer" aria-label="Emoji: Face with thermometer">">
 there is a monocyte cluster specific enriched in severe #COVID19 and receding during recovery/anti-IL6R...https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Expressing LOADS of cytokines & chemokineshttps://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol"> #Inflammasome gene upregulation (Il1B, NRLP3)https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Severe #COVID19 monocytes express https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">IL6 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤒" title="Face with thermometer" aria-label="Emoji: Face with thermometer">" title="https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">there is a monocyte cluster specific enriched in severe #COVID19 and receding during recovery/anti-IL6R...https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Expressing LOADS of cytokines & chemokineshttps://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol"> #Inflammasome gene upregulation (Il1B, NRLP3)https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Severe #COVID19 monocytes express https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">IL6 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤒" title="Face with thermometer" aria-label="Emoji: Face with thermometer">">
there is a monocyte cluster specific enriched in severe #COVID19 and receding during recovery/anti-IL6R...https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Expressing LOADS of cytokines & chemokineshttps://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol"> #Inflammasome gene upregulation (Il1B, NRLP3)https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Severe #COVID19 monocytes express https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">IL6 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤒" title="Face with thermometer" aria-label="Emoji: Face with thermometer">" title="https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">there is a monocyte cluster specific enriched in severe #COVID19 and receding during recovery/anti-IL6R...https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Expressing LOADS of cytokines & chemokineshttps://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol"> #Inflammasome gene upregulation (Il1B, NRLP3)https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Severe #COVID19 monocytes express https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">IL6 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤒" title="Face with thermometer" aria-label="Emoji: Face with thermometer">">
 Another #COVID19 #singlecell @medrxivpreprint on patients shows https://www.medrxiv.org/content/1... inflammatory monocyte/macrophage population in bronchoalveolar lavage fluidhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="⁉️" title="Exclamation question mark" aria-label="Emoji: Exclamation question mark">Does the severe-mono population in the blood look like any of these BAL populations?" title="https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Another #COVID19 #singlecell @medrxivpreprint on patients shows https://www.medrxiv.org/content/1... inflammatory monocyte/macrophage population in bronchoalveolar lavage fluidhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="⁉️" title="Exclamation question mark" aria-label="Emoji: Exclamation question mark">Does the severe-mono population in the blood look like any of these BAL populations?" class="img-responsive" style="max-width:100%;"/>
Another #COVID19 #singlecell @medrxivpreprint on patients shows https://www.medrxiv.org/content/1... inflammatory monocyte/macrophage population in bronchoalveolar lavage fluidhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="⁉️" title="Exclamation question mark" aria-label="Emoji: Exclamation question mark">Does the severe-mono population in the blood look like any of these BAL populations?" title="https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol">Another #COVID19 #singlecell @medrxivpreprint on patients shows https://www.medrxiv.org/content/1... inflammatory monocyte/macrophage population in bronchoalveolar lavage fluidhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="⁉️" title="Exclamation question mark" aria-label="Emoji: Exclamation question mark">Does the severe-mono population in the blood look like any of these BAL populations?" class="img-responsive" style="max-width:100%;"/>