1/ #Lymphopenia has recently been under the spotlight with the ongoing COVID-19 pandemic.
This is a quick #Tweetorial attempting to decypher the mechanisms behind lymphopenia, its causes and potential consequences.
What is the most common cause of transient lymphopenia?
This is a quick #Tweetorial attempting to decypher the mechanisms behind lymphopenia, its causes and potential consequences.
What is the most common cause of transient lymphopenia?
2/ Lymphocytes are predominantly T cells (~70%, CD4/8), followed by B cells (~10-20%) and NK cells (~10%).
Normal ALC (absolute lymphocyte count) ranges between 4000 and 10000 cells/microL.
Lymphopenia (or lymphocytopenia) is defined by an ALC of <1000 cells/microL for adults.
Normal ALC (absolute lymphocyte count) ranges between 4000 and 10000 cells/microL.
Lymphopenia (or lymphocytopenia) is defined by an ALC of <1000 cells/microL for adults.
3/ Lymphopoiesis:
- Production in the bone marrow. All lymphocytes arise from a CLP (common lymphoid progenitor).
- Differentiation, selection of T cells in the thymus.
- All lymphocytes (B, T, NK) then continue their maturation in the periphery (lymph nodes, spleen, MALT).
- Production in the bone marrow. All lymphocytes arise from a CLP (common lymphoid progenitor).
- Differentiation, selection of T cells in the thymus.
- All lymphocytes (B, T, NK) then continue their maturation in the periphery (lymph nodes, spleen, MALT).
4/ As you can imagine, any insult (central or peripheral) during this process can lead to decreased production of mature lymphocytes (known as lymphopenia).
Mechanisms of lymphopenia:
- immune damage of progenitor/blood cells or impaired lymphopoiesis (e.g. viral diseases)
Mechanisms of lymphopenia:
- immune damage of progenitor/blood cells or impaired lymphopoiesis (e.g. viral diseases)
5/
- direct infection of blood cells, inducing cell apoptosis and growth inhibition (e.g. viral diseases)
- antibody-dependent cytotoxicity (ADCC) (e.g. SLE)
- complement mediated cytolysis of lymphocytes (e.g. SLE)
- lymphocyte sequestration (e.g. siponimod)
- https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">apoptosis
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow">apoptosis
- direct infection of blood cells, inducing cell apoptosis and growth inhibition (e.g. viral diseases)
- antibody-dependent cytotoxicity (ADCC) (e.g. SLE)
- complement mediated cytolysis of lymphocytes (e.g. SLE)
- lymphocyte sequestration (e.g. siponimod)
-
6/ Common causes of lymphopenia:
- Infection: HIV, coronavirus, influenza, hepatitides, rubeola, polioviruses, varicella-zoster, typhoid fever, brucellosis, malaria, widespread TB, rickettsia, ehrlichia.
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="⛔️" title="No entry" aria-label="Emoji: No entry">Sepsis is the most common cause of transient
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⛔️" title="No entry" aria-label="Emoji: No entry">Sepsis is the most common cause of transient  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Downwards arrow" aria-label="Emoji: Downwards arrow">ALC.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Downwards arrow" aria-label="Emoji: Downwards arrow">ALC.
- Infection: HIV, coronavirus, influenza, hepatitides, rubeola, polioviruses, varicella-zoster, typhoid fever, brucellosis, malaria, widespread TB, rickettsia, ehrlichia.
7/
- Auto-immune diseases: SLE, RA, Sjogren& #39;s disease, sarcoidosis
- Malignancy: lymphoma, metastatic solid tumors
- Severe malnutrition (most common cause worldwide, related to reduced production.)
- Severe trauma
- Alcohol abuse
- Cushing& #39;s syndrome
- Zinc deficiency
- Auto-immune diseases: SLE, RA, Sjogren& #39;s disease, sarcoidosis
- Malignancy: lymphoma, metastatic solid tumors
- Severe malnutrition (most common cause worldwide, related to reduced production.)
- Severe trauma
- Alcohol abuse
- Cushing& #39;s syndrome
- Zinc deficiency
8/
- Organ transplants
- GVHD
- Medication-induced: chemotherapy (fludarabine, cladribine), steroids (even inhaled), MTX, AZA, rituximab, carbamazepine, MS drugs (siponimod, NTZ), etc.
- Total body irradiation
- Congenital immunodeficiencies (SCID, DiGeorge syndrome)
- Idiopathic
- Organ transplants
- GVHD
- Medication-induced: chemotherapy (fludarabine, cladribine), steroids (even inhaled), MTX, AZA, rituximab, carbamazepine, MS drugs (siponimod, NTZ), etc.
- Total body irradiation
- Congenital immunodeficiencies (SCID, DiGeorge syndrome)
- Idiopathic
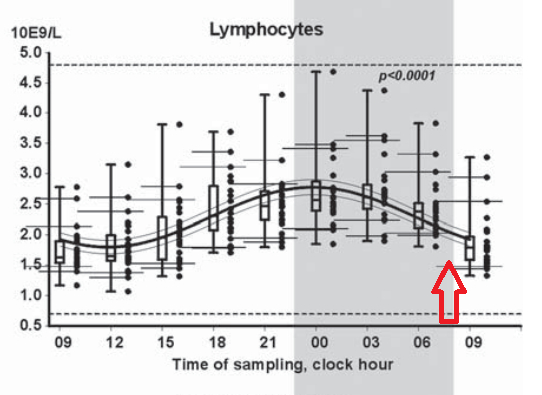
9/ Lymphopenia is usually reversible and most frequently associated with acute illness (sepsis, trauma, major surgery). https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="White heavy check mark" aria-label="Emoji: White heavy check mark">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="White heavy check mark" aria-label="Emoji: White heavy check mark">
There is a diurnal variation in lymphocyte counts, probably related to a change in corticosteroid levels. https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔃" title="Clockwise downwards and upwards open circle arrows" aria-label="Emoji: Clockwise downwards and upwards open circle arrows">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔃" title="Clockwise downwards and upwards open circle arrows" aria-label="Emoji: Clockwise downwards and upwards open circle arrows">
There is a diurnal variation in lymphocyte counts, probably related to a change in corticosteroid levels.
10/ Early morning venous sampling from patients resting in bed has important physiological influences on the lymphocyte count and subset numbers.
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="⛔️" title="No entry" aria-label="Emoji: No entry">Careful with interpretation of moderately-low ALC in hospitalized patients in early AM (nadir): doi:10.3109/00365513.2011.602422
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⛔️" title="No entry" aria-label="Emoji: No entry">Careful with interpretation of moderately-low ALC in hospitalized patients in early AM (nadir): doi:10.3109/00365513.2011.602422
11/ Prolonged and severe lymphopenia (~6% of total cases) predisposes to opportunistic viral (PML, CMV reactivation, hepatitis B reactivation, VZV reactivation), fungal (PJP, disseminated Cryptococcus & Candida) and mycobacterial infections (TB, MAC).
12/ When faced with prolonged lymphopenia:
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="1⃣" title="Keycap digit one" aria-label="Emoji: Keycap digit one">Evaluate medication list for unnecessary medications that could be contributing to the problem.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="1⃣" title="Keycap digit one" aria-label="Emoji: Keycap digit one">Evaluate medication list for unnecessary medications that could be contributing to the problem.
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="2⃣" title="Keycap digit two" aria-label="Emoji: Keycap digit two">Assess HIV status.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="2⃣" title="Keycap digit two" aria-label="Emoji: Keycap digit two">Assess HIV status.
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="3⃣" title="Keycap digit three" aria-label="Emoji: Keycap digit three">Measure lymphocyte subpopulations by flow cytometry and immunoglobulin levels to further characterize deficiency.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="3⃣" title="Keycap digit three" aria-label="Emoji: Keycap digit three">Measure lymphocyte subpopulations by flow cytometry and immunoglobulin levels to further characterize deficiency.
13/ No interventions are generally necessary for patients with asymptomatic lymphocytopenia without an associated illness.
Degree of #COVID19-related lymphopenia is proportional to severity of disease (more common with ARDS) & improves with resolution of disease.
Degree of #COVID19-related lymphopenia is proportional to severity of disease (more common with ARDS) & improves with resolution of disease.
14/ Remember that lymphopenia is not specific to #COVID19. Ask for medication list and look for underlying immunosuppression.
15/ For further reading:
Kipps TJ. Chapter 81. Lymphocytosis and Lymphocytopenia. Williams Hematology, 8e New York, NY: McGraw-Hill; 2010.
Castelino et. al: https://www.ncbi.nlm.nih.gov/pubmed/9145181
Davids:
https://www.ncbi.nlm.nih.gov/pubmed/91... href=" https://www.uptodate.com/contents/approach-to-the-adult-with-lymphocytosis-or-lymphocytopenia">https://www.uptodate.com/contents/...
Kipps TJ. Chapter 81. Lymphocytosis and Lymphocytopenia. Williams Hematology, 8e New York, NY: McGraw-Hill; 2010.
Castelino et. al: https://www.ncbi.nlm.nih.gov/pubmed/9145181
Davids:

 Read on Twitter
Read on Twitter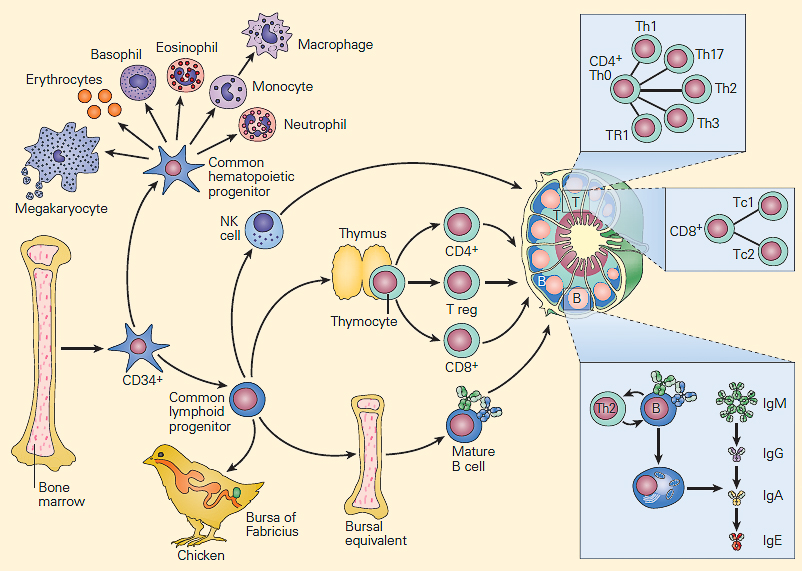
 Careful with interpretation of moderately-low ALC in hospitalized patients in early AM (nadir): doi:10.3109/00365513.2011.602422" title="10/ Early morning venous sampling from patients resting in bed has important physiological influences on the lymphocyte count and subset numbers. https://abs.twimg.com/emoji/v2/... draggable="false" alt="⛔️" title="No entry" aria-label="Emoji: No entry">Careful with interpretation of moderately-low ALC in hospitalized patients in early AM (nadir): doi:10.3109/00365513.2011.602422" class="img-responsive" style="max-width:100%;"/>
Careful with interpretation of moderately-low ALC in hospitalized patients in early AM (nadir): doi:10.3109/00365513.2011.602422" title="10/ Early morning venous sampling from patients resting in bed has important physiological influences on the lymphocyte count and subset numbers. https://abs.twimg.com/emoji/v2/... draggable="false" alt="⛔️" title="No entry" aria-label="Emoji: No entry">Careful with interpretation of moderately-low ALC in hospitalized patients in early AM (nadir): doi:10.3109/00365513.2011.602422" class="img-responsive" style="max-width:100%;"/>


