In the COVID19 era @ScottHalpernMD reminded me that the most common refrain nowadays is "All models are wrong but some are useful."
Here& #39;s a walkthrough of how we built a hopefully useful epidemic model to inform hospital planning @PennMedNews
https://bit.ly/2xaV1qU
/1">https://bit.ly/2xaV1qU&q...
Here& #39;s a walkthrough of how we built a hopefully useful epidemic model to inform hospital planning @PennMedNews
https://bit.ly/2xaV1qU
/1">https://bit.ly/2xaV1qU&q...
Second and only slightly less well known, is "Just because you can build a model doesn& #39;t mean you should."
Well in this case, our health system was faced with questions like how many beds will we need? How many ICU beds? How many ventilators? How soon will we need them?
/2
Well in this case, our health system was faced with questions like how many beds will we need? How many ICU beds? How many ventilators? How soon will we need them?
/2
So we did need a model to help answer these questions. But this isn& #39;t a Kaggle tournament, or a bet against Vegas odds, so different rules apply. Decisions on resources, staffing, machines must be made weeks in advance with layers of contingencies.
/3
/3
So we needed to be able, still early in the epidemic in our region, to be able to explore different scenarios and understand the *range* of likely possibilities. It didn& #39;t matter of the model predicted 100 or 101 beds. We needed to know if the real number was likely
/4
/4
between X and Y, & prepare for those scenarios accordingly. The interface needed to be intuitive. And it needed to be operational yesterday. Enter @mdraugelis @cranedroesch @CjBayesian @beckerfuffle @therealthaibinh et al from Penn Predictive Healthcare to make it happen
/5
/5
So how to choose a modeling approach that is useful, adaptable, and readily parameterizable? At one extreme of complexity, epidemic dynamics rely heavily on the structure of contact networks ( https://arxiv.org/pdf/cond-mat/0102028.pdf)">https://arxiv.org/pdf/cond-... but obtaining necessary data is very challenging
/6
/6
The Susceptible-Infected-Removed model, based on a system of differential equations and three distinct populations, has been around for decades and is a very simplified approximation of early dynamics of an epidemic, with exponential growth ( https://en.wikipedia.org/wiki/Kermack%E2%80%93McKendrick_theory)">https://en.wikipedia.org/wiki/Kerm...
/7
/7
Other intermediately complex approaches include SEIR models (an adaptation of SIR with an additional population of Exposed individuals), e.g. https://alhill.shinyapps.io/COVID19seir/ ,">https://alhill.shinyapps.io/COVID19se... or polynomial curve fitting further-along epidemics and recalibrating locally e.g. https://covid19.healthdata.org/
/8">https://covid19.healthdata.org/">...
/8">https://covid19.healthdata.org/">...
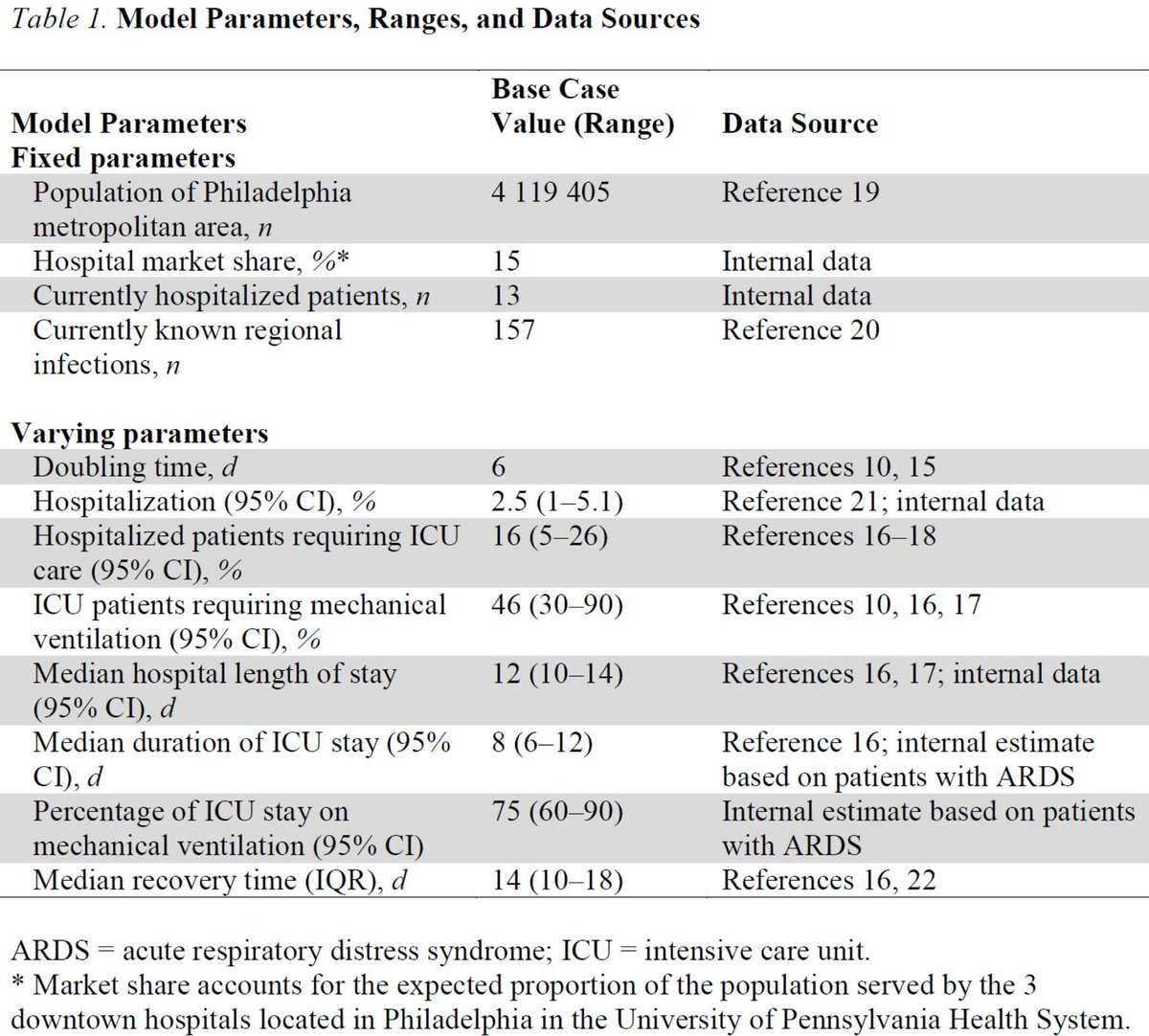
Regardless of the underlying model, none of these approaches translate case counts into numbers of hospital or ICU beds, or ventilators, so we relied on published case series out of China and Italy,
http://www.nejm.org/doi/10.1056/NEJMoa2002032
https://www.nejm.org/doi/10.10... href=" https://linkinghub.elsevier.com/retrieve/pii/S0140673620305663
https://linkinghub.elsevier.com/retrieve/... href=" http://jamanetwork.com/journals/jama/fullarticle/2763188
/9">https://jamanetwork.com/journals/...
http://www.nejm.org/doi/10.1056/NEJMoa2002032
/9">https://jamanetwork.com/journals/...
And combined based on data from prior cohorts and clinical experience with patients with acute respiratory failure, including based on studies of triage patterns by @georgeanesi who has been leading our division efforts in COVID19 preparations. But we didn& #39;t select
/10
/10
one number for each of these parameters, rather a range of possibilities from which we sampled to run 1000 simulated epidemics. And one particular number is critical to the epidemic dynamics: the doubling time. That is, how long does it take for the number of cases to double?
/11
/11
The doubling time is tricky b/c it changes over the course of the epidemic as different populations are exposed, as social distancing measures are put into place, as testing and quarantining programs are implemented. Early on we saw other countries with ranges of 2-10 days
/12
/12
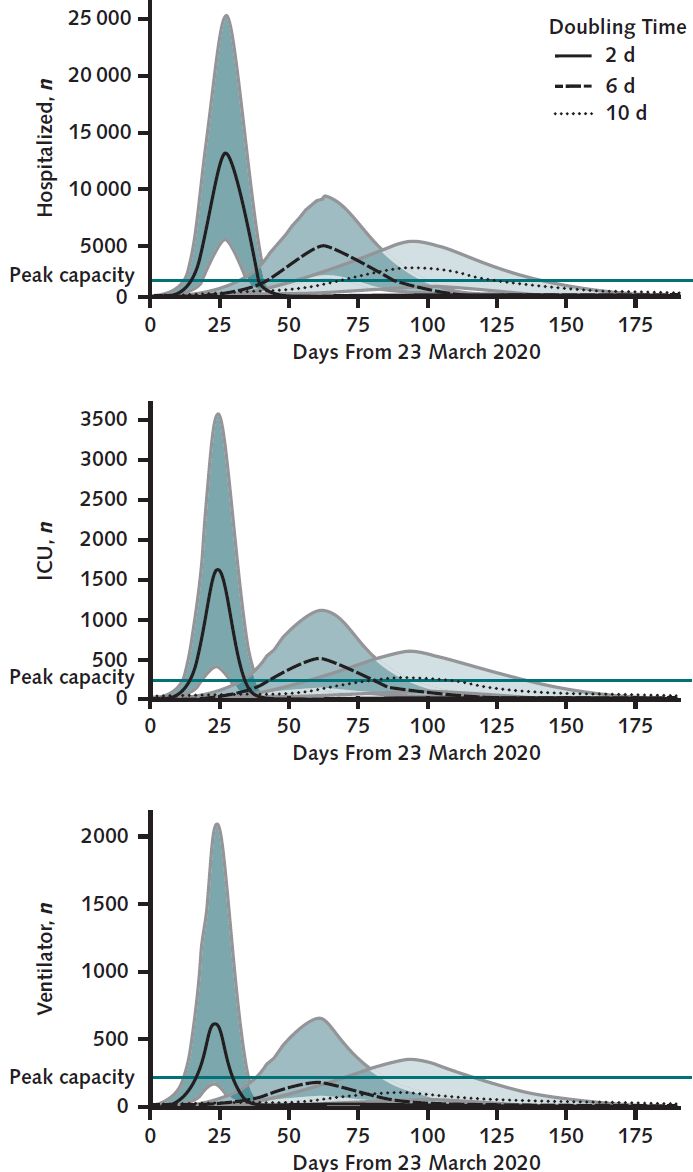
So we looked at extremes, best and worst cases, and a middling case to see how dramatically the doubling time would inform our hospital predictions for needed resources. The results were dramatically different based on different doubling time scenarios.
/13
/13
But these scenarios offered a glimpse into the ranges we were considering, rough estimates on the bounds of best and worst scenarios for the next couple of weeks, acknowledging that the epidemic dynamics would change during that time, requiring new predictions along the way
/14
/14
With updated regional and local data. Hence the role for a flexible, quickly adaptable interface to explore these dynamics that could be quickly reparameterized with new data and augmented with additional layers of complexity as needed. Check it here: https://penn-chime.phl.io/
/15">https://penn-chime.phl.io/">...
/15">https://penn-chime.phl.io/">...
One note on the social distancing parameter: As stated above, SIR models don& #39;t account for the structure of contact networks, and assume that everyone mixes homogeneously, which is of course not true in real life.
/16
/16
So the CHIME social distancing parameter is a linear scaling factor on the overall amount of social mixing (beta in the SIR model) while still assuming homogeneous mixing. This is difficult to parameterize even with recently published Google mobility data
/17
/17
So this approach is limited, & we didn& #39;t include it in the paper, but reinforces at the least the magnitude of the effect that distancing will have on the eventual epidemic dynamics, even though quantifying this effect empirically is challenging for any modeling approach.
/18
/18
So we estimated the COVID19 course in our health system would be anywhere from extremely challenging and burdensome to grim beyond imagination. Expanded ICUs, cancelling elective cases and transfers, all decisions aided by exploring CHIME scenarios.
/19
/19
Grateful to @AnnalsofIM for the opportunity to share our experience and the chance to work with leaders at @PAIRCenter @PennMedNews who are responding to the pandemic with nothing but earnestness, care, grace, and tremendous compassion for our patients and healthcare workers.
/20
/20
The response and preparation has been inspiring. So we made a wrong, necessary, and useful model, and we& #39;re continuing to update CHIME and assess its performance prospectively, results forthcoming.
Contribute to CHIME here: https://github.com/CodeForPhilly/chime
/21">https://github.com/CodeForPh...
Contribute to CHIME here: https://github.com/CodeForPhilly/chime
/21">https://github.com/CodeForPh...

 Read on Twitter
Read on Twitter