I’m going to go out on a limb and hypothesize that glucose-6-phosphate dehydrogenase (G6PD) enzyme level/function plays a central pathophysiologic role in host cell response to SARS-CoV2 infection. Explains a lot of clinical observations. #Coronavirus #COVID19.
I’m a little rusty on my #biochemistry, but I did get a degree in it back in the day from @Harvard, & I do remember enough about G6PD deficiency from #USMLE #Step1 @YaleMed before becoming a #Radiologist. So here it goes...
A few population-level observations about the demographics of COVID19. First, disease incidence/prevalence/case-fatality rates seem to be particularly high in Iran, Italy, & Spain, i.e. Mediterranean populations, as tracked by the the @JohnsHopkinsSPH map. https://coronavirus.jhu.edu/map.html ">https://coronavirus.jhu.edu/map.html&...
Second, hospitalized men have a 75% higher mortality than hospitalized women. Sure, men may have more underlying risk factors like history of smoking and other comorbidities, but 75% is high! https://www.latimes.com/science/story/2020-03-21/why-is-the-coronavirus-more-deadly-for-men-than-for-women">https://www.latimes.com/science/s...
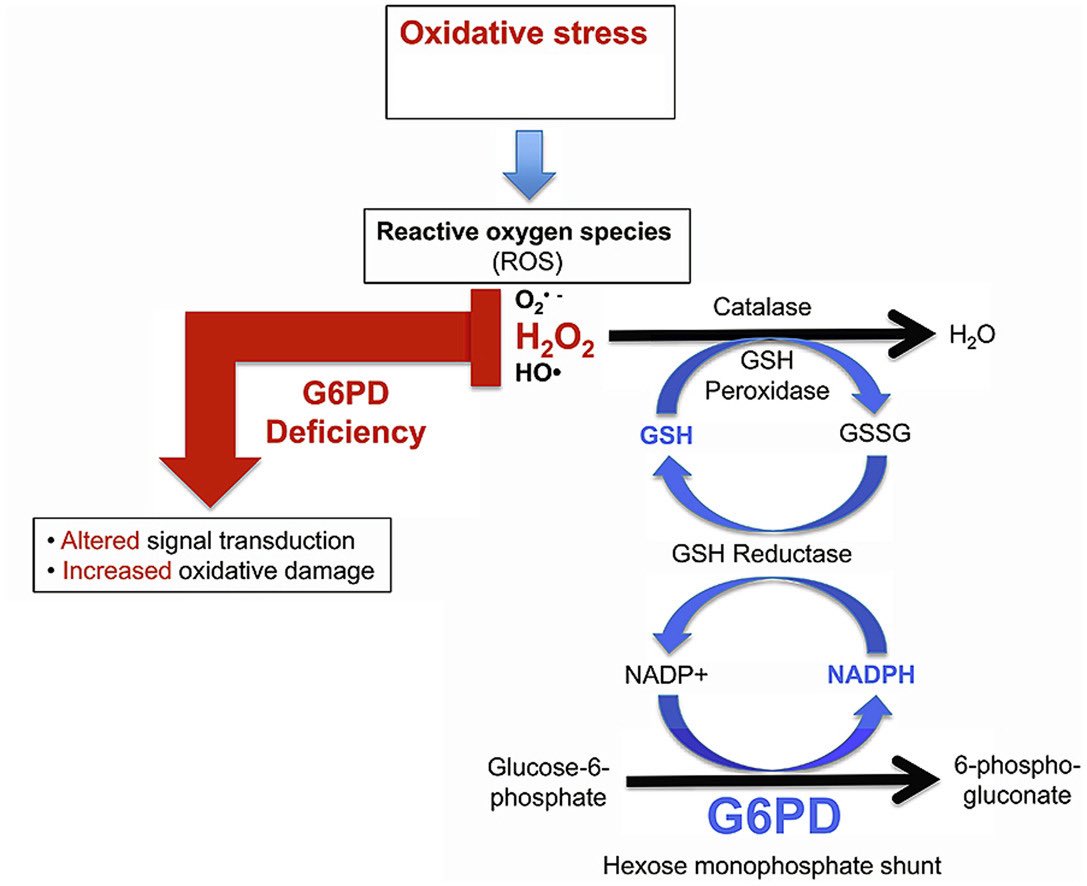
So what is G6PD? It is an enzyme which acts as a fire extinguisher for cytotoxic reactive oxygen species, which can be thought of as hand grenades used by our white blood cells to destroy the lipid membranes of pathogens. But like grenades, they can injure us, too.
It turns out that G6PD is encoded on the X Chromosome, giving men (46XY) only 1 copy of the enzyme and women 2 copies (46XX). G6PD deficiency is a well-understood X-linked recessive disease. https://ghr.nlm.nih.gov/condition/glucose-6-phosphate-dehydrogenase-deficiency">https://ghr.nlm.nih.gov/condition...
G6PD deficiency is prevalent in Middle Eastern/Mediterranean populations (ie, Iran, Italy, Spain, etc.) and is known to have variable expressivity depending on the exact mutation involved. It is classically diagnosed with symptoms triggered by fava bean consumption (my favorite!)
G6PD deficiency causes ROS to damage our own cells’ lipid membranes, leading to lysis https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol"> . Elevated serum levels of Lactate dehydrogenase (LDH) are known to reflect this process, & high LDH has been shown to be prognostic of severe disease in COVID19. https://www.medrxiv.org/content/10.1101/2020.03.24.20040162v1">https://www.medrxiv.org/content/1...
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💥" title="Collision symbol" aria-label="Emoji: Collision symbol"> . Elevated serum levels of Lactate dehydrogenase (LDH) are known to reflect this process, & high LDH has been shown to be prognostic of severe disease in COVID19. https://www.medrxiv.org/content/10.1101/2020.03.24.20040162v1">https://www.medrxiv.org/content/1...
Sometimes being G6PD deficient is a good thing! For example, in regions where malaria is endemic, this is a protective trait against the disease, termed a “balanced polymorphism” in genetics. https://www.thelancet.com/pdfs/journals/lanhae/PIIS2352-3026(15)00191-X.pdf">https://www.thelancet.com/pdfs/jour...
When lipid membrane damage occurs to red boood cells, they take on abnormal shapes known as schistocytes, seen on peripheral blood smears, and causative of microvascular angiopathy and thrombosis. These findings are being recognized & reported in COVID19. https://www.hematology.org/covid-19/covid-19-and-coagulopathy">https://www.hematology.org/covid-19/...
Along that same vein (no pun intended), lymphopenia is being reported as a specific finding in COVID19, in part because SARS-CoV2 may directly infect/lyse lymphocytes, but also because lymphocytes are particularly susceptible to oxidative stress. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4608155/">https://www.ncbi.nlm.nih.gov/pmc/artic...
ARDS is the severe lung disease to which many COVID19 patients succumb, & is characterized by extensive inflammatory injury to lung parenchyma by ROS. Surfactant is the special chemical made by Type 2 Pneumocytes & plays a key protective role against ROS. https://academic.oup.com/toxsci/article/166/1/108/5061323">https://academic.oup.com/toxsci/ar...
Unfortunately SARS-CoV2 has a particular predilection to attack Type 2 Pneumocytes, causing surfactant deficiency. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2312501/">https://www.ncbi.nlm.nih.gov/pmc/artic...
So how does hydroxychloroquine, the drug conventionally used to treat malaria and autoimmune diseases like Lupus, fit into all of this exactly? This paper nicely ties it all together. https://www.ahajournals.org/doi/full/10.1161/HYPERTENSIONAHA.114.03587">https://www.ahajournals.org/doi/full/...
N-acetyl-cysteine (NAC) is a medication used to restore cells’ glutathione levels, a reductive agent used to quench ROS. I am cautiously optimistic that it may have some therapeutic benefit in treating COVID19. I just learned this is going to be trialed: https://www.biospace.com/article/releases/new-covid-19-hope-clinical-trial-recommendations-introduced-today-may-reduce-or-eliminate-mechanical-ventilation-for-coronavirus-patients/">https://www.biospace.com/article/r...

 Read on Twitter
Read on Twitter